
- Mobile Apps
- Journal Club
- Antibiotics
- Quick Critical Care
- Residency Directory
- Recent Changes
- About WikEM
- Getting Started
- Creating & Editing
- Needed Pages
- Editorial Levels
- Contribution Score
- Elective Guide
- Citing WikEM
- What links here
- Related changes
- Special pages
- Printable version
- Permanent link
- Page information
- Browse properties

- View source
- View history
- Create account

We need you! See something you could improve? Make an edit and help make WikEM better for everyone.
- Wandering atrial pacemaker
- 2 Clinical Features
- 3.1 Palpitations
- 4.2 Diagnosis
- 5 Management
- 6 Disposition
- 8 External Links
- 9 References
- Three or more ectopic foci within the atrial myocardium serve as the pacemaker
- Rate is less than 100bpm (in contrast to MAT )
- Is irregularly irregular therefore sometimes confused with atrial fibrillation and sinus arrhythmia
- Intrinsic cardiac or pulmonary disease
- Metabolic derangements
- Drug toxicity (including Digoxin )

Clinical Features
- Often seen in the extremes of age and in athletes
- Rarely causes symptoms
Differential Diagnosis
Palpitations.
- Narrow-complex tachycardias
- Wide-complex tachycardias
- Second Degree AV Block Type I (Wenckeback)
- Second Degree AV Block Type II
- Third Degree AV Block
- Premature atrial contraction
- Premature junctional contraction
- Premature ventricular contraction
- Sick sinus syndrome
- Acute coronary syndrome
- Cardiomyopathy
- Congenital heart disease
- Congestive heart failure (CHF)
- Mitral valve prolapse
- Pacemaker complication
- Pericarditis
- Myocarditis
- Valvular disease
- Panic attack
- Somatic Symptom Disorder
- Drugs of abuse (e.g. cocaine )
- Medications (e.g. digoxin , theophylline )
- Thyroid storm
- Pulmonary embolism
- Dehydration
- Pheochromocytoma

- ECG should show three distinct P wave morphologies with a ventricular rate <100bpm
- Rarely requires treatment
Disposition
- Outpatient management
- Multifocal atrial tachycardia
- Dysrhythmia
External Links
- Richard Cunningham
- fardis tavangary
- Ross Donaldson
- Privacy policy
- Disclaimers
- Patient Resources
- Heart Information Topics A-Z
- Know Your Numbers
- BMI Calculator
- Women's Heart Health
- Project Heart Smart K-6
- Heart Health Information
- Video Education

Available in English and Spanish, this e-newsletter separates fact from fiction on over 40 heart topics by Texas Heart Medical Group's Dr. Stephanie Coulter.
- Core Services
- Applied Engineering
- Biorepository Core
- Cell Profiling Core
- Flow Cytometry and Sorting
- Medicinal Chemistry
- Pathology Services
- Preclinic Surgical and Interventional Testing Services
- Scientific Publications & Grants
- Communications
- Editorial Services
- Office of Research Administration
- Departments & Labs
- Cardiomyocyte Renewal Lab
- Electrophysiology Basic Research
- Electrophysiology Clinical Research & Innovations
- Flow Cytometry & Imaging
- Gene Editing Lab
- Innovative Device & Engineering Applications Lab (IDEA)
- Molecular Cardiology Research
- Pathology Research
- Regenerative Medicine Research
- Center for Clinical Research
- Center for Women's Heart & Vascular Health
- Center for Preclinical Surgical & Interventional Research
- Stem Cell Center
- Office of Education
- Fellowships + Residencies
- School of Perfusion Tech
- THI Journal
- Cardiac Society
- Student Engagement
- Events Calendar
- CME Live Events
- CME On Demand
- CME My Portal
- Information Technology
- Office of Research & Administration
- Public Affairs
Can you explain if/when junctional rhythm is a serious issue?
Doesn’t junctional rhythm mean the sino-atrial node has failed and one is relying on the AV node for the heart’s pacing?
In the last two years, I seem to be in a junctional rhythm constantly, sometimes with sinus rhythm as well….Seen several MDs and had a fairly comprehensive workup in last several years including normal echo, CMRI, and Holter/Event studies showed nothing alarming….Just completed a 30 day event study and saw the EP yesterday…He said nothing was life threatening on it. The events I submitted on the monitor ended up being junctional rhythm issues…
Submitted by Rich from Pennsylvania on 03/26/2014

A Junctional rhythm can happen either due to the sinus node slowing down or the AV node speeding up. It is generally a benign arrhythmia and in the absence of structural heart disease and symptoms, generally no treatment is required. If symptoms are present and specifically related to the junctional rhythm, then a dual chamber pacemaker may be helpful.
You can see how this popup was set up in our step-by-step guide: https://wppopupmaker.com/guides/auto-opening-announcement-popups/

Visit U.S. News & World Report


Pacemaker Rhythms – Normal Patterns
- Ed Burns and Robert Buttner
- Jul 7, 2022
Pacemaker Components
1. pulse generator.
- Power source
- Control circuitry
- Transmitter / Receiver
- Reed Switch (Magnet activated switch)
- Single or multiple
- Unipolar or bipolar
Pacemaker Classification
- Pacemakers are classified by the nature of their pacing mode.
- Classification follows pacemaker code developed by the North American Society of Pacing and Electrophysiology (NASPE) and the British Pacing and Electrophysiology Group (BPEG).
- The NASPE/BPEG Generic (NBG) Pacemaker Code was last revised in 2002, although many textbooks still use the previous version from 1987.
- The code is expressed as a series of up to five letters.
NBG Pacemaker Code (2002)
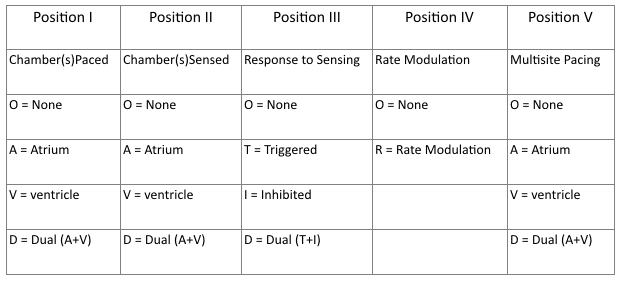
- Refers to chambers paced.
- Refers to the location where the pacemaker senses native cardiac electrical activity.
- Refers to pacemakers response to sensed native cardiac activity.
- T = Sensed activity results in triggering of paced activity
- I = Sensed activity results in inhibition of pacing activity
- Indicates ability for rate modulation designed to altered heart appropriately to meet physiological needs e.g. physical activity. Sensors may measure and respond to variables including vibration, respiration, or acid-base status.
- Allows indication of multiple stimulation sites within one anatomical area e.g. more than one pacing site within the atria or biatrial pacing
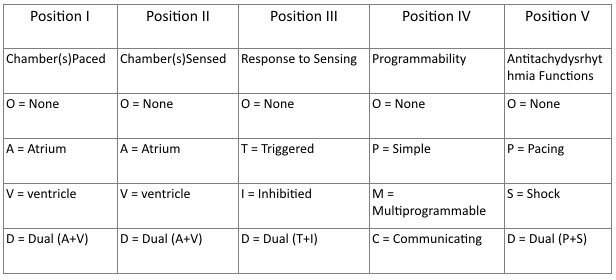
- Same as 2002 guidelines.
- Reflects the programming options available for pacemaker set-up or presence of rate modulation ability.
- Refers to presences of anti-tachydysrhythmia functions. Superseded by the NASPE/BPEG Defibrillator Code.
Common Pacing Modes
AAI – Atrial pacing and sensing
- If native atrial activity sensed then pacing is inhibited.
- If no native activity sensed for pre-determined time then atrial pacing initiated.
- Used in sinus node dysfunction with intact AV conduction.
- Also termed atrial demand mode.
VVI – Ventricle pacing and sensing
- Similar to AAI mode but involving ventricles instead of the atrium.
- Used in patients with chronic atrial impairment e.g. atrial fibrillation or flutter.
DDD – pacing and sensing the atria and ventricles
- Commonest pacing mode.
- Atrial pacing occurs if no native atrial activity for set time.
- Ventricular pacing occurs if no native ventricle activity for set time following atrial activity.
- Atrial channel function is suspend during a fixed periods following atrial and ventricular activity to prevent sensing ventricular activity or retrograde p waves as native atrial activity.
Magnet mode
- Applying a magnet to a pacemaker will initiate the magnet mode.
- This mode varies with pacemaker set-up and manufacturer.
- Usually initiates an asynchronous pacing mode – AOO, VOO, or DOO.
- Asynchronous modes deliver constant rate paced stimuli regardless of native rate of rhythm.
- In asynchronous ventricle pacing there is a risk of pacemaker-induced ventricular tachycardia.
- Note this differs from magnet application to an Implantable Cardioversion Defibrillator (ICD) which results in defibrillator deactivation.
Criteria for Pacemaker Insertion
- The 2002 American College of Cardiology, American Heart Association and North American Society for Pacing and Electrophysiology guidelines for implantation of cardiac pacemakers .
- ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities
Paced ECG – Electrocardiographic Features
The appearance of the ECG in a paced patient is dependent on the pacing mode used, placement of pacing leads, device pacing thresholds, and the presence of native electrical activity. Features of the paced ECG are: Pacing spikes
- Vertical spikes of short duration, usually 2 ms.
- May be difficult to see in all leads.
- Amplitude depends on position and type of lead.
- Bipolar leads result in a much smaller pacing spike than unipolar leads.
- Epicardially placed leads result in smaller pacing spikes than endocardially placed leads.
Atrial Pacing
- Pacing spike precedes the p wave.
- Morphology of p wave dependent of lead placement but may appear normal.
Ventricular Pacing
- Pacing spike precedes the QRS complex.
- Right ventricle pacing lead placement results in a QRS morphology similar to LBBB .
- Left epicardial pacing lead placement results in a QRS morphology similar to RBBB .
- ST segments and T waves should be discordant with the QRS complex i.e. the major terminal portion of the QRS complex is located on the opposite side of the baseline from the ST segment and T wave.
Dual Chamber Pacing
- Dependent on areas begin paced.
- May exhibit features of atrial pacing, ventricular pacing or both.
- Pacing spikes may precede only p wave, only QRS complex, or both.
The absence of paced complexes does not always mean pacemaker failure as it may reflect satisfactory native conduction. ECG Features

ECG Examples

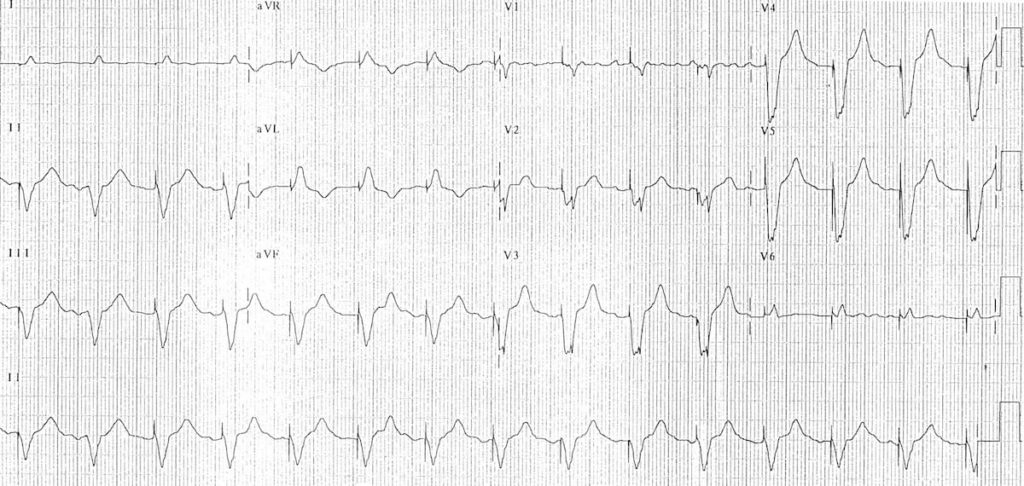
A-V sequential pacing:
- Atrial and ventricular pacing spikes are visible before each QRS complex.
- There is 100% atrial capture — small P waves are seen following each atrial pacing spike.
- There is 100% ventricular capture — a QRS complex follows each ventricular pacing spike.
- QRS complexes are broad with a LBBB morphology, indicating the presence of a ventricular pacing electrode in the right ventricle.

- A-V sequential pacing — atrial and ventricular pacing spikes precede each QRS complex with 100% capture.

- Another example of A-V sequential pacing.
Ventricular paced rhythm:
- Ventricular pacing spikes precede each QRS complex (except perhaps complex #2 — although the QRS morphology in this complex is identical to the rest of the ECG, suggesting that this beat is also paced)
- No atrial pacing spikes are seen.
- The underlying native rhythm is probably coarse atrial fibrillation — there are several possible P waves visible in V1 but otherwise the atrial activity is chaotic.

- Ventricular pacing spikes precede most of the QRS complexes.
- The 6th and 7th beats are narrower, with a different morphology — these are non-paced (“capture”) beats, probably supraventricular in origin.
- There is a pacing spike superimposed on beat #6, but this does not appear to alter its morphology — i.e. no evidence of a fusion complex.

- Ventricular pacing spikes precede the QRS complexes, most of which exhibit LBBB morphology consistent with a RV pacing electrode.
- The 5th, 6th and 11th complexes are narrower with a different morphology — these are fusion beats produced when the ventricle is simultaneously activated by both paced and supraventricular (native) impulses. You can see how the pacing spike is shortened and the QRS duration narrowed by the co-incident native impulse.
- The 4th complex is probably a supraventricular capture beat , although there may still be some hybridisation with a pacing spike.
Atrially paced patients often have evidence of 1st degree AV block or Wenckebach conduction on their paced ECG that is not apparent on their baseline tracing.
This is because the sort of patients that require atrial pacing (e.g. post-op cardiac surgery) commonly have some degree of AV node dysfunction (e.g. due to age-related AV-nodal degeneration / their underlying cardiac condition / post-operative ischaemia / AV-nodal blocking drugs).
When these patients are paced at a faster rate than their AV node can handle, the AV node becomes “fatigued” resulting in 1st degree AV block or Wenckebach phenomenon on the paced ECG. This abnormality is not clinically important provided that the patient’s cardiac output is not compromised.

Atrial paced rhythm with 1st degree AV block:
- There are regular pacing spikes at 90 bpm.
- Each pacing spike is followed by a P wave, indicating 100% atrial capture.
- P waves are conducted to the ventricles with a prolonged PR interval (280 ms).

Atrial paced rhythm with Wenckebach conduction:
- There are regular atrial pacing spikes at 90 bpm; each one is followed by a small P wave indicating 100% atrial capture.
- However, not every P wave results in a QRS complex — the PR interval progressively lengthens, culminating in failure of AV conduction (“dropped QRS complexes”).
- There is a co-existent 2nd degree AV block with Mobitz I conduction (Wenckebach phenomenon).
- The Mobitz I is due to the patient being paced at a rate faster than his AV node can handle — at his own intrinsic rate of 50-60 bpm he had only a 1st degree AV block.
To find out the story behind this ECG, check out ECG Exigency 011 .
Pacemaker Puzzler
Can you work out what is going on in this ECG?

- There is an irregularly irregular rhythm with multiple atrial and ventricular pacing spikes.
- The majority of the QRS complexes are broad (120ms) and preceded by ventricular pacing spikes.
- The LBBB morphology is consistent with a ventricular pacing electrode located in the right ventricle.
The varying relationship between the atrial and ventricular pacing spikes is best understood by examining the lead II rhythm strip (below):
- Beat 1 is narrow — this appears to be a native ventricular complex triggered by an atrial pacing spike. This indicates that AV conduction is intact to some degree (i.e. 3rd degree AV block cannot be present).
- Beat 9 is broad with a completely different morphology and axis to the rest of the strip — this is a ventricular ectopic beat.
- Beats 3, 6, 8, 10 and 12 are preceded by both atrial and ventricular pacing spikes — sequential A-V pacing.
- Beats 2, 4, 5, 7 and 11 are preceded by ventricular pacing spikes only. The absence of atrial pacing spikes suggests that the pacemaker is responding to native supraventriclar impulses.
- Given the absence of discernible P waves and the very irregular rhythm, it is likely that the underlying native rhythm is atrial fibrillation.

- Atrial fibrillation with DDD pacing and occasional ventricular ectopics.

Related Topics
- Pacemaker essentials: Medmastery
- Pacemaker malfunction
- Left bundle branch block
- Right bundle branch block
- Sgarbossa Criteria
- Bernstein AD, Camm AJ, Fletcher RD, Gold RD, Rickards AF, Smyth NP, Spielman SR, Sutton R. The NASPE/BPEG generic pacemaker code for antibradyarrhythmia and adaptive-rate pacing and antitachyarrhythmia devices . Pacing Clin Electrophysiol. 1987 Jul;10(4 Pt 1):794-9.
- Bernstein AD, Daubert JC, Fletcher RD, Hayes DL, Lüderitz B, Reynolds DW, Schoenfeld MH, Sutton R. The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. North American Society of Pacing and Electrophysiology/British Pacing and Electrophysiology Group . Pacing Clin Electrophysiol. 2002 Feb;25(2):260-4
- Gregoratos G et al. ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/NASPE Committee to Update the 1998 Pacemaker Guidelines) . Circulation. 2002 Oct 15;106(16):2145-61
Advanced Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course : Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop . Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog .
- Zimmerman FH. ECG Core Curriculum . 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations , 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine . 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care . 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG . 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |

Robert Buttner
MBBS (UWA) CCPU (RCE, Biliary, DVT, E-FAST, AAA) Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Editor-in-chief of the LITFL ECG Library . Twitter: @rob_buttner
One comment
[…] Review on pacemaker modes at: https://litfl.com/pacemaker-rhythms-normal-patterns/ […]
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Privacy Overview
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Anaesth
- v.60(6); 2016 Jun
Intraoperative wandering atrial pacemaker with isoflurane anaesthesia
Sulagna bhattacharjee.
Department of Anaesthesiology, All India Institute of Medical Sciences, New Delhi, India
Puneet Khanna
Sumit bansal, souvik maitra, associated data.
Wandering atrial pacemaker is an arrhythmia originating from the shifting pacemaker sites from the sinoatrial node to the atria and/or atrioventricular node and back to the sinoatrial node.[ 1 ] We report an incident of wandering atrial pacemaker occurring intraoperatively during surgery for testicular torsion.
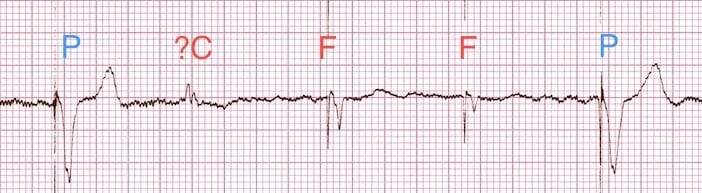
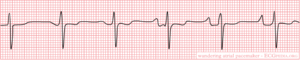
A 10-year-old boy, American Society of Anesthesiologists (ASA) physical status I, undergoing surgery for a right-sided testicular torsion had received fentanyl, propofol and atracurium for anaesthesia management. After securing his airway with a ProSeal™ laryngeal mask airway, anaesthesia was maintained with isoflurane, air and oxygen under standard ASA monitoring. During manipulation of the testis, he had an episode of bradycardia with heart rate decreasing from 88/min to 54/min without any hypotension or oxygen desaturation that persisted for about 15 s. This was followed by an arrhythmia with rate of 74–78/min having varyingP wave morphology and PR interval that resolved spontaneously [ Figure 1 and Video 1 ]. We diagnosed it to be a case of wandering atrial pacemaker as the heart rate was between 60 and 100/min, with slight irregularity, beat to beat changing shape and size ofP wave of at least three different forms, varying PR interval but normally appearing QRS complexes.[ 2 ] The likely cause of occurrence of arrhythmia was vagal stimulation caused by testicular manipulation. All commonly used volatile anaesthetic agents including isoflurane are known to cause enhanced automaticity of subsidiary atrial pacemakers,[ 3 ] thereby predisposing to the development of atrial arrhythmias and wandering pacemaker phenomenon. Monitoring and recognising this event for possible haemodynamic compromise are important.

Variant morphology of P wave in lead II
Video available on www.ijaweb.org
Financial support and sponsorship, conflicts of interest.
There are no conflicts of interest.
Wandering Pacemaker
When several pacemakers are competing, p-waves with different origins and thus configurations occur. The rhythm is slightly different from beat to beat.
note If the heart rate increases to above 100bpm, it is called Multifocal Atrial Tachycardia . Possible causes are hypoxia, COPD and medication such as digoxin.
Navigation menu
Electrical Injury and Wandering Atrial Pacemaker
Affiliation.
- 1 Internal Medicine, Anti-Retroviral Therapy Centre, District Hospital, Khagaria, IND.
- PMID: 34725597
- PMCID: PMC8553291
- DOI: 10.7759/cureus.18335
The supply of household electricity remains a low-voltage (110-220 V) energy source, and its effects on the human body depend on several factors, including the type of contact and duration of contact, among other things. In a significant number of cases, direct contact with household electricity causes reversible cardiac arrhythmia-ventricular fibrillation, ventricular premature beats, atrial tachycardia, and atrial fibrillation. Wandering atrial pacemaker (WAP) is a benign atrial arrhythmia observed in elderly patients suffering from obstructive pulmonary diseases that result from an ischemic heart. This report discusses WAP as observed in a patient who suffered an electrical injury.
Keywords: ampere; arrhythmia; electrical injury; voltage; wandering atrial pacemaker.
Copyright © 2021, Singh et al.
Publication types
- Case Reports
Wandering Atrial Pacemaker ECG Interpretation #312
Description.
- Rhythms are often named according to the origin of the electrical activity in the heart or the structure where the problem is occurring.
- Wandering Atrial Pacemaker is aptly named due to the electrical impulses causing the atrial activity are moving or wandering.
- These changes in the locus of stimulation affect the morphology of the P waves.
- In Wandering Atrial Pacemaker ECG, you must observe at least three different shaped P waves. No other changes in the tracing may be observed. The rhythm may or may not be regular.
- The PR interval is often affected, but does not have to be.
- The bottom line, is you must observe at least three different shaped P waves.
Practice Strip
Analyze this tracing using the five steps of rhythm analysis.
- Rhythm: Irregular
- P wave: Changing Shapes (3 or more)
- PR interval: Variable
- Interpretation: Wandering Atrial Pacemaker
Authors and Reviewers
- ECG heart rhythm modules: Thomas O'Brien.
- ECG monitor simulation developer: Steve Collmann
- 12 Lead Course: Dr. Michael Mazzini, MD .
- Spanish language ECG: Breena R. Taira, MD, MPH
- Medical review: Dr. Jonathan Keroes, MD
- Medical review: Dr. Pedro Azevedo, MD, Cardiology
- Last Update: 11/8/2021
- Electrocardiography for Healthcare Professionals, 6th Edition Kathryn Booth and Thomas O'Brien ISBN10: 1265013470, ISBN13: 9781265013479 McGraw Hill, 2023
- Rapid Interpretation of EKG's, Sixth Edition Dale Dublin Cover Publishing Company
- EKG Reference Guide EKG.Academy
- 12 Lead EKG for Nurses: Simple Steps to Interpret Rhythms, Arrhythmias, Blocks, Hypertrophy, Infarcts, & Cardiac Drugs Aaron Reed Create Space Independent Publishing
- Heart Sounds and Murmurs: A Practical Guide with Audio CD-ROM 3rd Edition Elsevier-Health Sciences Division Barbara A. Erickson, PhD, RN, CCRN
- The Virtual Cardiac Patient: A Multimedia Guide to Heart Sounds, Murmurs, EKG Jonathan Keroes, David Lieberman Publisher: Lippincott Williams & Wilkin) ISBN-10: 0781784425; ISBN-13: 978-0781784429
- Project Semilla, UCLA Emergency Medicine, EKG Training Breena R. Taira, MD, MPH
- ECG Reference Guide PracticalClinicalSkills.com
This website provides professional medical education. For medical care contact your doctor. 2024 ©MedEdu LLC. All Rights Reserved. Terms & Conditions | About Us | Privacy | Email Us | 1

IMAGES
VIDEO
COMMENTS
A wandering atrial pacemaker is usually found with an electrocardiogram ( EKG or ECG). It's a test that lets your doctor see a record of the electrical signals in your heart. If the irregular ...
Wandering atrial pacemaker (WAP) is an atrial rhythm where the pacemaking activity of the heart originates from different locations within the atria. This is different from normal pacemaking activity, where the sinoatrial node (SA node) is responsible for each heartbeat and keeps a steady rate and rhythm. Causes of wandering atrial pacemaker are unclear, but there may be factors leading to its ...
Wandering Atrial Pacemaker (WAP) is a cardiac rhythm disorder that causes irregular and variable heartbeats. Learn the Heart - Healio provides a comprehensive ECG review of this condition ...
This rhythm and multifocal atrial tachycardia are similar except for heart rate. The other possible explanation is that there is significant respiratory sinus arrhythmia, with uncovering of latent foci of pacemaker activity. Usually, it is associated with underlying lung disease. In the elderly, it may be a manifestation of sick sinus syndrome.
The atrial rate can be slower than the typical 300 bpm (cycle length 200 ms) in the presence of antiarrhythmic drugs or scarring. It is also known as "typical atrial flutter" or "cavotricuspid isthmus-dependent atrial flutter" or "counterclockwise atrial flutter." • Cavotricuspid isthmus-dependent atrial flutter: reverse typical
Wandering atrial pacemaker. Mechanisms and causes. There are three or more ectopic atrial pacemakers. This arrhythmia is typically seen in young healthy persons, particularly athletes. The etiology is uncertain. Heart rate—the heart rate is 60-100 and is usually irregular. ECG morphology
Wandering atrial pacemaker. Non-arrhythmic cardiac causes: Acute coronary syndrome. Cardiomyopathy. Congenital heart disease. Congestive heart failure (CHF) Mitral valve prolapse. Pacemaker complication. Pericarditis.
A junctional rhythm is a heart rhythm problem that can make your heartbeat too slow or too fast. If you have a junctional rhythm, you may not have any symptoms. But sometimes, this condition can make you feel faint, weak or out of breath. If symptoms interfere with your daily life, your provider may recommend treatment to regulate your heartbeat.
Wandering atrial pacemaker (WAP) is a benign atrial arrhythmia observed in elderly patients suffering from obstructive pulmonary diseases that result from an ischemic heart. This report discusses WAP as observed in a patient who suffered an electrical injury. Keywords: wandering atrial pacemaker, voltage, electrical injury, arrhythmia, ampere.
A Junctional rhythm can happen either due to the sinus node slowing down or the AV node speeding up. It is generally a benign arrhythmia and in the absence of structural heart disease and symptoms, generally no treatment is required. If symptoms are present and specifically related to the junctional rhythm, then a dual chamber pacemaker may be helpful.
A pacemaker is a small battery-operated device that helps the heart beat in a regular rhythm. Traditional pacemakers have three parts: a generator, wires (leads) and sensors (electrodes). Some newer pacemakers are wireless. It produces electrical impulses to help control abnormal heartbeats. It's implanted under the skin through a small ...
Wandering atrial pacemaker (WAP) occurs when the pacemaker site shifts back and forth between the sinus node and ectopic atrial sites. The P-wave morphology will vary as the pacemaker "wanders" between the multiple sites. Generally, at least three different P-wave morphologies should be identified before making the diagnosis of WAP.
Figure 1. Imaging of the Migrated Temporary Epicardial Pacemaker Wire. (A) Transesophageal echocardiogram revealing a linear density (W) in the left ventricle (LV) attached to the mitral valve (MV) traveling through the bioprosthetic aortic valve (AV) and into the ascending aorta (A). (B) Computed tomography angiogram showing the 15-cm density ...
Diagnose Wandering Atrial Pacemaker with confidence! This video explores the shifting pacemaker sites and the resulting "multifocal P waves" observed on an E...
Atrial channel function is suspend during a fixed periods following atrial and ventricular activity to prevent sensing ventricular activity or retrograde p waves as native atrial activity. Magnet mode. Applying a magnet to a pacemaker will initiate the magnet mode. This mode varies with pacemaker set-up and manufacturer.
Sir, Wandering atrial pacemaker is an arrhythmia originating from the shifting pacemaker sites from the sinoatrial node to the atria and/or atrioventricular node and back to the sinoatrial node. [ 1] We report an incident of wandering atrial pacemaker occurring intraoperatively during surgery for testicular torsion.
Wandering Pacemaker. Wandering pacemaker. Every p-wave is different and thus has a different origin. When several pacemakers are competing, p-waves with different origins and thus configurations occur. The rhythm is slightly different from beat to beat. note If the heart rate increases to above 100bpm, it is called Multifocal Atrial Tachycardia.
Wandering atrial pacemaker (WAP) is a benign atrial arrhythmia observed in elderly patients suffering from obstructive pulmonary diseases that result from an ischemic heart. This report discusses WAP as observed in a patient who suffered an electrical injury. Keywords: ampere; arrhythmia; electrical injury; voltage; wandering atrial pacemaker ...
Analysis. In Wandering Atrial Pacemaker ECG, you must observe at least three different shaped P waves. No other changes in the tracing may be observed. The rhythm may or may not be regular. The PR interval is often affected, but does not have to be. The bottom line, is you must observe at least three different shaped P waves.
Ellis W. Lader MD, FACC, FAHA, FACP. Search for more papers by this author. Book Author(s):
Wandering Atrial Pacemaker (WAP) SPECIAL NOTE: Usually, you will have some NORMAL P wave configurations and two (or more) other Pwave configurations with a WAP (such as shown below). However, to call the EKG a WAP, you must see THREE different P wave configurations in your EKG Strip. Ectopic means 'other' sites (than SA node).