- Patient Care & Health Information
- Diseases & Conditions
- Traveler's diarrhea
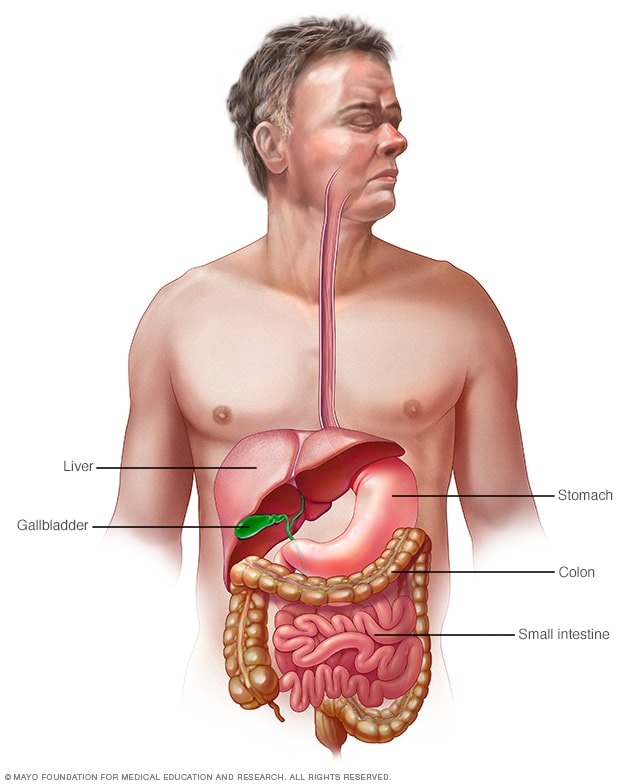

Gastrointestinal tract
Your digestive tract stretches from your mouth to your anus. It includes the organs necessary to digest food, absorb nutrients and process waste.
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant.
When you visit a place where the climate or sanitary practices are different from yours at home, you have an increased risk of developing traveler's diarrhea.
To reduce your risk of traveler's diarrhea, be careful about what you eat and drink while traveling. If you do develop traveler's diarrhea, chances are it will go away without treatment. However, it's a good idea to have doctor-approved medicines with you when you travel to high-risk areas. This way, you'll be prepared in case diarrhea gets severe or won't go away.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
- A Book: Mayo Clinic on Digestive Health
Traveler's diarrhea may begin suddenly during your trip or shortly after you return home. Most people improve within 1 to 2 days without treatment and recover completely within a week. However, you can have multiple episodes of traveler's diarrhea during one trip.
The most common symptoms of traveler's diarrhea are:
- Suddenly passing three or more looser watery stools a day.
- An urgent need to pass stool.
- Stomach cramps.
Sometimes, people experience moderate to severe dehydration, ongoing vomiting, a high fever, bloody stools, or severe pain in the belly or rectum. If you or your child experiences any of these symptoms or if the diarrhea lasts longer than a few days, it's time to see a health care professional.
When to see a doctor
Traveler's diarrhea usually goes away on its own within several days. Symptoms may last longer and be more severe if it's caused by certain bacteria or parasites. In such cases, you may need prescription medicines to help you get better.
If you're an adult, see your doctor if:
- Your diarrhea lasts beyond two days.
- You become dehydrated.
- You have severe stomach or rectal pain.
- You have bloody or black stools.
- You have a fever above 102 F (39 C).
While traveling internationally, a local embassy or consulate may be able to help you find a well-regarded medical professional who speaks your language.
Be especially cautious with children because traveler's diarrhea can cause severe dehydration in a short time. Call a doctor if your child is sick and has any of the following symptoms:
- Ongoing vomiting.
- A fever of 102 F (39 C) or more.
- Bloody stools or severe diarrhea.
- Dry mouth or crying without tears.
- Signs of being unusually sleepy, drowsy or unresponsive.
- Decreased volume of urine, including fewer wet diapers in infants.
It's possible that traveler's diarrhea may stem from the stress of traveling or a change in diet. But usually infectious agents — such as bacteria, viruses or parasites — are to blame. You typically develop traveler's diarrhea after ingesting food or water contaminated with organisms from feces.
So why aren't natives of high-risk countries affected in the same way? Often their bodies have become used to the bacteria and have developed immunity to them.
Risk factors
Each year millions of international travelers experience traveler's diarrhea. High-risk destinations for traveler's diarrhea include areas of:
- Central America.
- South America.
- South Asia and Southeast Asia.
Traveling to Eastern Europe, South Africa, Central and East Asia, the Middle East, and a few Caribbean islands also poses some risk. However, your risk of traveler's diarrhea is generally low in Northern and Western Europe, Japan, Canada, Singapore, Australia, New Zealand, and the United States.
Your chances of getting traveler's diarrhea are mostly determined by your destination. But certain groups of people have a greater risk of developing the condition. These include:
- Young adults. The condition is slightly more common in young adult tourists. Though the reasons why aren't clear, it's possible that young adults lack acquired immunity. They may also be more adventurous than older people in their travels and dietary choices, or they may be less careful about avoiding contaminated foods.
- People with weakened immune systems. A weakened immune system due to an underlying illness or immune-suppressing medicines such as corticosteroids increases risk of infections.
- People with diabetes, inflammatory bowel disease, or severe kidney, liver or heart disease. These conditions can leave you more prone to infection or increase your risk of a more-severe infection.
- People who take acid blockers or antacids. Acid in the stomach tends to destroy organisms, so a reduction in stomach acid may leave more opportunity for bacterial survival.
- People who travel during certain seasons. The risk of traveler's diarrhea varies by season in certain parts of the world. For example, risk is highest in South Asia during the hot months just before the monsoons.
Complications
Because you lose vital fluids, salts and minerals during a bout with traveler's diarrhea, you may become dehydrated, especially during the summer months. Dehydration is especially dangerous for children, older adults and people with weakened immune systems.
Dehydration caused by diarrhea can cause serious complications, including organ damage, shock or coma. Symptoms of dehydration include a very dry mouth, intense thirst, little or no urination, dizziness, or extreme weakness.
Watch what you eat
The general rule of thumb when traveling to another country is this: Boil it, cook it, peel it or forget it. But it's still possible to get sick even if you follow these rules.
Other tips that may help decrease your risk of getting sick include:
- Don't consume food from street vendors.
- Don't consume unpasteurized milk and dairy products, including ice cream.
- Don't eat raw or undercooked meat, fish and shellfish.
- Don't eat moist food at room temperature, such as sauces and buffet offerings.
- Eat foods that are well cooked and served hot.
- Stick to fruits and vegetables that you can peel yourself, such as bananas, oranges and avocados. Stay away from salads and from fruits you can't peel, such as grapes and berries.
- Be aware that alcohol in a drink won't keep you safe from contaminated water or ice.
Don't drink the water
When visiting high-risk areas, keep the following tips in mind:
- Don't drink unsterilized water — from tap, well or stream. If you need to consume local water, boil it for three minutes. Let the water cool naturally and store it in a clean covered container.
- Don't use locally made ice cubes or drink mixed fruit juices made with tap water.
- Beware of sliced fruit that may have been washed in contaminated water.
- Use bottled or boiled water to mix baby formula.
- Order hot beverages, such as coffee or tea, and make sure they're steaming hot.
- Feel free to drink canned or bottled drinks in their original containers — including water, carbonated beverages, beer or wine — as long as you break the seals on the containers yourself. Wipe off any can or bottle before drinking or pouring.
- Use bottled water to brush your teeth.
- Don't swim in water that may be contaminated.
- Keep your mouth closed while showering.
If it's not possible to buy bottled water or boil your water, bring some means to purify water. Consider a water-filter pump with a microstrainer filter that can filter out small microorganisms.
You also can chemically disinfect water with iodine or chlorine. Iodine tends to be more effective, but is best reserved for short trips, as too much iodine can be harmful to your system. You can purchase water-disinfecting tablets containing chlorine, iodine tablets or crystals, or other disinfecting agents at camping stores and pharmacies. Be sure to follow the directions on the package.
Follow additional tips
Here are other ways to reduce your risk of traveler's diarrhea:
- Make sure dishes and utensils are clean and dry before using them.
- Wash your hands often and always before eating. If washing isn't possible, use an alcohol-based hand sanitizer with at least 60% alcohol to clean your hands before eating.
- Seek out food items that require little handling in preparation.
- Keep children from putting things — including their dirty hands — in their mouths. If possible, keep infants from crawling on dirty floors.
- Tie a colored ribbon around the bathroom faucet to remind you not to drink — or brush your teeth with — tap water.
Other preventive measures
Public health experts generally don't recommend taking antibiotics to prevent traveler's diarrhea, because doing so can contribute to the development of antibiotic-resistant bacteria.
Antibiotics provide no protection against viruses and parasites, but they can give travelers a false sense of security about the risks of consuming local foods and beverages. They also can cause unpleasant side effects, such as skin rashes, skin reactions to the sun and vaginal yeast infections.
As a preventive measure, some doctors suggest taking bismuth subsalicylate, which has been shown to decrease the likelihood of diarrhea. However, don't take this medicine for longer than three weeks, and don't take it at all if you're pregnant or allergic to aspirin. Talk to your doctor before taking bismuth subsalicylate if you're taking certain medicines, such as anticoagulants.
Common harmless side effects of bismuth subsalicylate include a black-colored tongue and dark stools. In some cases, it can cause constipation, nausea and, rarely, ringing in your ears, called tinnitus.
- Feldman M, et al., eds. Infectious enteritis and proctocolitis. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 25, 2021.
- LaRocque R, et al. Travelers' diarrhea: Microbiology, epidemiology, and prevention. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Ferri FF. Traveler diarrhea. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed April 28, 2023.
- Diarrhea. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea. Accessed April 27, 2023.
- Travelers' diarrhea. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/preparing-international-travelers/travelers-diarrhea. Accessed April 28, 2023.
- LaRocque R, et al. Travelers' diarrhea: Clinical manifestations, diagnosis, and treatment. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Khanna S (expert opinion). Mayo Clinic. May 29, 2021.
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- GP practice services
- Health advice
- Health research
- Medical professionals
- Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
- Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Motion sickness
Travel sickness.
Peer reviewed by Dr Hayley Willacy, FRCGP Last updated by Dr Colin Tidy, MRCGP Last updated 16 Mar 2023
Meets Patient’s editorial guidelines
In this series: Health advice for travel abroad Travelling to remote locations Ears and flying Jet lag Altitude sickness
Motion sickness (travel sickness) is common, especially in children. It is caused by repeated unusual movements during travelling, which send strong (sometimes confusing) signals to the balance and position sensors in the brain.
In this article :
What causes motion sickness, how long does motion sickness last, motion sickness symptoms, how to stop motion sickness, natural treatments for motion sickness, motion sickness medicines, what can a doctor prescribe for motion sickness, what should i do if i'm actually sick, what is mal de debarquement syndrome.
Continue reading below
Motion sickness is a normal response to repeated movements, such as going over bumps or around in a circle, send lots of messages to your brain. If you are inside a vehicle, particularly if you are focused on things that are inside the vehicle with you then the signals that your eyes send to the brain may tell it that your position is not changing, whilst your balance mechanisms say otherwise.
Your balance mechanisms in your inner ears sense different signals to those that your eyes are seeing which then sends your brain mixed, confusing messages. This confusion between messages then causes people to experience motion sickness.
Is motion sickness normal?
Motion sickness is a normal response that anyone can have when experiencing real or perceived motion. Although all people can develop motion sickness if exposed to sufficiently intense motion, some people are rarely affected while other people are more susceptible and have to deal with motion sickness very often.
Triggers for motion sickness
Motion sickness can also be triggered by anxiety or strong smells, such as food or petrol. Sometimes trying to read a book or a map can trigger motion sickness. Both in children and adults, playing computer games can sometimes cause motion sickness to occur.
Motion sickness is more common in children and also in women. Fortunately, many children grow out of having motion sickness. It is not known why some people develop motion sickness more than others. Symptoms can develop in cars, trains, planes and boats and on amusement park rides, etc.
Symptoms typically go when the journey is over; however, not always. In some people they last a few hours, or even days, after the journey ends.
There are various symptoms of motion sickness including::
Feeling sick (nausea and vomiting).
Sweating and cold sweats.
Increase in saliva.
Headaches .
Feeling cold and going pale.
Feeling weak.
Some general tips to avoid motion sickness include the following.
Prepare for your journey
Don't eat a heavy meal before travelling. Light, carbohydrate-based food like cereals an hour or two before you travel is best.
On long journeys, try breaking the journey to have some fresh air, drink some cold water and, if possible, take a short walk.
For more in-depth advice on travelling generally, see the separate leaflets called Health Advice for Travel Abroad , Travelling to Remote Locations , Ears and Flying (Aeroplane Ear) , Jet Lag and Altitude Sickness .
Plan where you sit
Keep motion to a minimum. For example, sit in the front seat of a car, over the wing of a plane, or on deck in the middle of a boat.
On a boat, stay on deck and avoid the cafeteria or sitting where your can smell the engines.
Breathe fresh air
Breathe fresh air if possible. For example, open a car window.
Avoid strong smells, particularly petrol and diesel fumes. This may mean closing the window and turning on the air conditioning, or avoiding the engine area in a boat.
Use your eyes and ears differently
Close your eyes (and keep them closed for the whole journey). This reduces 'positional' signals from your eyes to your brain and reduces the confusion.
Don't try to read.
Try listening to an audio book with your eyes closed. There is some evidence that distracting your brain with audio signals can reduce your sensitivity to the motion signals.
Try to sleep - this works mainly because your eyes are closed, but it is possible that your brain is able to ignore some motion signals when you are asleep.
Do not read or watch a film.
It is advisable not to watch moving objects such as waves or other cars. Don't look at things your brain expects to stay still, like a book inside the car. Instead, look ahead, a little above the horizon, at a fixed place.
If you are the driver you are less likely to feel motion sickness. This is probably because you are constantly focused on the road ahead and attuned to the movements that you expect the vehicle to make. If you are not, or can't be, the driver, sitting in the front and watching what the driver is watching can be helpful.
Treat your tummy gently
Avoid heavy meals and do not drink alcohol before and during travelling. It may also be worth avoiding spicy or fatty food.
Try to 'tame your tummy' with sips of a cold water or a sweet, fizzy drink. Cola or ginger ale are recommended.
Try alternative treatments
Sea-Bands® are acupressure bands that you wear on your wrists to put pressure on acupressure points that Chinese medicine suggests affects motion sickness. Some people find that they are effective.
Homeopathic medicines seem to help some people, and will not make you drowsy. The usual homeopathic remedy is called 'nux vom'. Follow the instructions on the packet.
All the techniques above which aim to prevent motion sickness will also help reduce it once it has begun. Other techniques, which are useful on their own to treat motion sickness but can also be used with medicines if required, are:
Breathe deeply and slowly and, while focusing on your breathing, listening to music. This has been proved to be effective in clinical trials.
Ginger - can improve motion sickness in some people (as a biscuit or sweet, or in a drink).
There are several motion sickness medicines available which can reduce, or prevent, symptoms of motion sickness. You can buy them from pharmacies or, in some cases, get them on prescription. They work by interfering with the nerve signals described above.
Medicines are best taken before the journey. They may still help even if you take them after symptoms have begun, although once you feel sick you won't absorb medicines from the stomach very well. So, at this point, tablets that you put against your gums, or skin patches, are more likely to be effective.
Hyoscine is usually the most effective medicine for motion sickness . It is also known as scopolamine. It works by preventing the confusing nerve messages going to your brain.
There are several brands of medicines which contain hyoscine - they also come in a soluble form for children. You should take a dose 30-60 minutes before a journey; the effect can last up to 72 hours. Hyoscine comes as a patch for people aged 10 years or over. (This is only available on prescription - see below.) Side-effects of hyoscine include dry mouth , drowsiness and blurred vision.
Side-effects of motion sickness medicines
Some medicines used for motion sickness may cause drowsiness. Some people are extremely sensitive to this and may find that they are so drowsy that they can't function properly at all. For others the effects may be milder but can still impair your reactions and alertness. It is therefore advisable not to drive and not to operate heavy machinery if you have taken them. In addition, some medicines may interfere with alcohol or other medication; your doctor or the pharmacist can advise you about this.
Antihistamines
Antihistamines can also be useful , although they are not quite as effective as hyoscine. However, they usually cause fewer side-effects. Several types of antihistamine are sold for motion sickness. All can cause drowsiness, although some are more prone to cause it than others; for example, promethazine , which may be of use for young children on long journeys, particularly tends to cause drowsiness. Older children or adults may prefer one that is less likely to cause drowsiness - for example, cinnarizine or cyclizine.
Remember, if you give children medicines which cause drowsiness they can sometimes be irritable when the medicines wear off.
See the separate article called How to manage motion sickness .
There are a number of anti-sickness medicines which can only be prescribed by your doctor. Not all of them always work well for motion sickness, and finding something that works may be a case of trial and error. All of them work best taken up to an hour before your journey, and work less well if used when you already feel sick. See also the separate leaflet called Nausea (Causes, Symptoms, and Treatment) for more detailed information about these medicines .
Hyoscine patch
Hyoscine, or scopolamine, patches are suitable for adults and for children over 10 years old. The medicine is absorbed through your skin, although this method of medicine delivery is slow so the patch works best if applied well before your journey.
You should stick the patch on to the skin behind the ear 5-6 hours before travelling (often this will mean late on the previous night) and remove it at the end of the journey.
Prochlorperazine
Prochlorperazine is a prescription-only medicine which works by changing the actions of the chemicals that control the tendency to be sick (vomit), in your brain. One form of prochlorperazine is Buccastem®, which is absorbed through your gums and does not need to be swallowed. Buccastem® tastes rather bitter but it can be effective for sickness when you are already feeling sick, as it doesn't have to be absorbed by the stomach.
Metoclopramide
Metoclopramide is a tablet used to speed up the emptying of your tummy. Slow emptying of the tummy is something that happens when you develop nausea and vomiting, so metoclopramide can help prevent this. It prevents nausea and vomiting quite effectively in some people. It can occasionally have unpleasant side-effects, particularly in children (in whom it is not recommended). Metoclopramide is often helpful for those who tend to have gastric reflux, those who have slow tummy emptying because of previous surgery, and those who have type 1 diabetes. Your GP will advise whether metoclopramide is suitable for you.
Domperidone
Domperidone , like metoclopramide, is sometimes used for sickness caused by slow tummy emptying. It is not usually recommended for motion sickness but is occasionally used if other treatments don't help. Domperidone is not a legal medicine in some countries, including the USA.
Ondansetron
Ondansetron is a powerful antisickness medicine which is most commonly used for sickness caused by chemotherapy, and occasionally used for morning sickness in pregnancy. It is not usually effective for motion sickness. This, and its relatively high cost means that it is not prescribed for motion sickness alone. However, for those undergoing chemotherapy, and for those who have morning sickness aggravated by travel, ondansetron may be helpful.
If you're actually sick you may find that this relieves your symptoms a little, although not always for very long. If you've been sick:
Try a cool flannel on your forehead, try to get fresh air on your face and do your best to find a way to rinse your mouth to get rid of the taste.
Don't drink anything for ten to twenty minutes (or it may come straight back), although (very) tiny sips of very cold water, coke or ginger ale may help.
After this, go back to taking all the prevention measures above.
Once you reach your destination you may continue to feel unwell. Sleep if you can, sip cold iced water, and - when you feel ready - try some small carbohydrate snacks. Avoid watching TV (more moving objects to watch!) until you feel a little better.
The sensation called 'mal de debarquement' (French for sickness on disembarking) refers to the sensation you sometimes get after travel on a boat, train or plane, when you feel for a while as though the ground is rocking beneath your feet. It is probably caused by the overstimulation of the balance organs during your journey. It usually lasts only an hour or two, but in some people it can last for several days, particularly after a long sea journey. It does not usually require any treatment.
Persistent mal de debarquement syndrome is an uncommon condition in which these symptoms may persist for months or years.
Dr Mary Lowth is an author or the original author of this leaflet.
Further reading and references
- Spinks A, Wasiak J ; Scopolamine (hyoscine) for preventing and treating motion sickness. Cochrane Database Syst Rev. 2011 Jun 15;(6):CD002851.
- Lackner JR ; Motion sickness: more than nausea and vomiting. Exp Brain Res. 2014 Aug;232(8):2493-510. doi: 10.1007/s00221-014-4008-8. Epub 2014 Jun 25.
- Leung AK, Hon KL ; Motion sickness: an overview. Drugs Context. 2019 Dec 13;8:2019-9-4. doi: 10.7573/dic.2019-9-4. eCollection 2019.
- Zhang LL, Wang JQ, Qi RR, et al ; Motion Sickness: Current Knowledge and Recent Advance. CNS Neurosci Ther. 2016 Jan;22(1):15-24. doi: 10.1111/cns.12468. Epub 2015 Oct 9.
- Van Ombergen A, Van Rompaey V, Maes LK, et al ; Mal de debarquement syndrome: a systematic review. J Neurol. 2016 May;263(5):843-854. doi: 10.1007/s00415-015-7962-6. Epub 2015 Nov 11.
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 14 Mar 2028
16 mar 2023 | latest version.
Last updated by
Peer reviewed by

Feeling unwell?
Assess your symptoms online for free
Travel-Related Diagnoses Among U.S. Nonmigrant Travelers or Migrants Presenting to U.S. GeoSentinel Sites — GeoSentinel Network, 2012–2021
Surveillance Summaries / June 30, 2023 / 72(7);1–22
Please note: This report has been corrected. An erratum has been published.
Ashley B. Brown, MPH 1 ; Charles Miller, MSOR 1 ; Davidson H. Hamer, MD 2 ,3 ; Phyllis Kozarsky, MD 4 ; Michael Libman, MD 5 ; Ralph Huits, MD, PhD 6 ; Aisha Rizwan, MPH 7 ; Hannah Emetulu, MPH 7 ; Jesse Waggoner, MD 8 ; Lin H. Chen, MD 9 ,10 ; Daniel T. Leung, MD 11 ; Daniel Bourque, MD 3 ; Bradley A. Connor, MD 12 ; Carmelo Licitra, MD 13 ; Kristina M. Angelo, DO 1 ( View author affiliations )
Views: Views equals page views plus PDF downloads
Introduction, selected worldwide health event notifications, selected health event notifications in geosentinel, limitations, future directions, acknowledgments.
- Full Issue PDF
Problem/Condition: During 2012–2021, the volume of international travel reached record highs and lows. This period also was marked by the emergence or large outbreaks of multiple infectious diseases (e.g., Zika virus, yellow fever, and COVID-19). Over time, the growing ease and increased frequency of travel has resulted in the unprecedented global spread of infectious diseases. Detecting infectious diseases and other diagnoses among travelers can serve as sentinel surveillance for new or emerging pathogens and provide information to improve case identification, clinical management, and public health prevention and response.
Reporting Period: 2012–2021.
Description of System: Established in 1995, the GeoSentinel Network (GeoSentinel), a collaboration between CDC and the International Society of Travel Medicine, is a global, clinical-care–based surveillance and research network of travel and tropical medicine sites that monitors infectious diseases and other adverse health events that affect international travelers. GeoSentinel comprises 71 sites in 29 countries where clinicians diagnose illnesses and collect demographic, clinical, and travel-related information about diseases and illnesses acquired during travel using a standardized report form. Data are collected electronically via a secure CDC database, and daily reports are generated for assistance in detecting sentinel events (i.e., unusual patterns or clusters of disease). GeoSentinel sites collaborate to report disease or population-specific findings through retrospective database analyses and the collection of supplemental data to fill specific knowledge gaps. GeoSentinel also serves as a communications network by using internal notifications, ProMed alerts, and peer-reviewed publications to alert clinicians and public health professionals about global outbreaks and events that might affect travelers. This report summarizes data from 20 U.S. GeoSentinel sites and reports on the detection of three worldwide events that demonstrate GeoSentinel’s notification capability.
Results: During 2012–2021, data were collected by all GeoSentinel sites on approximately 200,000 patients who had approximately 244,000 confirmed or probable travel-related diagnoses. Twenty GeoSentinel sites from the United States contributed records during the 10-year surveillance period, submitting data on 18,336 patients, of which 17,389 lived in the United States and were evaluated by a clinician at a U.S. site after travel. Of those patients, 7,530 (43.3%) were recent migrants to the United States, and 9,859 (56.7%) were returning nonmigrant travelers.
Among the recent migrants to the United States, the median age was 28.5 years (range = <19 years to 93 years); 47.3% were female, and 6.0% were U.S. citizens. A majority (89.8%) were seen as outpatients, and among 4,672 migrants with information available, 4,148 (88.8%) did not receive pretravel health information. Of 13,986 diagnoses among migrants, the most frequent were vitamin D deficiency (20.2%), Blastocystis (10.9%), and latent tuberculosis (10.3%). Malaria was diagnosed in 54 (<1%) migrants. Of the 26 migrants diagnosed with malaria for whom pretravel information was known, 88.5% did not receive pretravel health information. Before November 16, 2018, patients’ reasons for travel, exposure country, and exposure region were not linked to an individual diagnosis. Thus, results of these data from January 1, 2012, to November 15, 2018 (early period), and from November 16, 2018, to December 31, 2021 (later period), are reported separately. During the early and later periods, the most frequent regions of exposure were Sub-Saharan Africa (22.7% and 26.2%, respectively), the Caribbean (21.3% and 8.4%, respectively), Central America (13.4% and 27.6%, respectively), and South East Asia (13.1% and 16.9%, respectively). Migrants with diagnosed malaria were most frequently exposed in Sub-Saharan Africa (89.3% and 100%, respectively).
Among nonmigrant travelers returning to the United States, the median age was 37 years (range = <19 years to 96 years); 55.7% were female, 75.3% were born in the United States, and 89.4% were U.S. citizens. A majority (90.6%) were seen as outpatients, and of 8,967 nonmigrant travelers with available information, 5,878 (65.6%) did not receive pretravel health information. Of 11,987 diagnoses, the most frequent were related to the gastrointestinal system (5,173; 43.2%). The most frequent diagnoses among nonmigrant travelers were acute diarrhea (16.9%), viral syndrome (4.9%), and irritable bowel syndrome (4.1%).
Malaria was diagnosed in 421 (3.5%) nonmigrant travelers. During the early (January 1, 2012, to November 15, 2018) and later (November 16, 2018, to December 31, 2021) periods, the most frequent reasons for travel among nonmigrant travelers were tourism (44.8% and 53.6%, respectively), travelers visiting friends and relatives (VFRs) (22.0% and 21.4%, respectively), business (13.4% and 12.3%, respectively), and missionary or humanitarian aid (13.1% and 6.2%, respectively). The most frequent regions of exposure for any diagnosis among nonmigrant travelers during the early and later period were Central America (19.2% and 17.3%, respectively), Sub-Saharan Africa (17.7% and 25.5%, respectively), the Caribbean (13.0% and 10.9%, respectively), and South East Asia (10.4% and 11.2%, respectively).
Nonmigrant travelers who had malaria diagnosed were most frequently exposed in Sub-Saharan Africa (88.6% and 95.9% during the early and later period, respectively) and VFRs (70.3% and 57.9%, respectively). Among VFRs with malaria, a majority did not receive pretravel health information (70.2% and 83.3%, respectively) or take malaria chemoprophylaxis (88.3% and 100%, respectively).
Interpretation: Among ill U.S. travelers evaluated at U.S. GeoSentinel sites after travel, the majority were nonmigrant travelers who most frequently received a gastrointestinal disease diagnosis, implying that persons from the United States traveling internationally might be exposed to contaminated food and water. Migrants most frequently received diagnoses of conditions such as vitamin D deficiency and latent tuberculosis, which might result from adverse circumstances before and during migration (e.g., malnutrition and food insecurity, limited access to adequate sanitation and hygiene, and crowded housing,). Malaria was diagnosed in both migrants and nonmigrant travelers, and only a limited number reported taking malaria chemoprophylaxis, which might be attributed to both barriers to acquiring pretravel health care (especially for VFRs) and lack of prevention practices (e.g., insect repellant use) during travel. The number of ill travelers evaluated by U.S. GeoSentinel sites after travel decreased in 2020 and 2021 compared with previous years because of the COVID-19 pandemic and associated travel restrictions. GeoSentinel detected limited cases of COVID-19 and did not detect any sentinel cases early in the pandemic because of the lack of global diagnostic testing capacity.
Public Health Action: The findings in this report describe the scope of health-related conditions that migrants and returning nonmigrant travelers to the United States acquired, illustrating risk for acquiring illnesses during travel. In addition, certain travelers do not seek pretravel health care, even when traveling to areas in which high-risk, preventable diseases are endemic. Health care professionals can aid international travelers by providing evaluations and destination-specific advice.
Health care professionals should both foster trust and enhance pretravel prevention messaging for VFRs, a group known to have a higher incidence of serious diseases after travel (e.g., malaria and enteric fever). Health care professionals should continue to advocate for medical care in underserved populations (e.g., VFRs and migrants) to prevent disease progression, reactivation, and potential spread to and within vulnerable populations. Because both travel and infectious diseases evolve, public health professionals should explore ways to enhance the detection of emerging diseases that might not be captured by current surveillance systems that are not site based.
Modern modes of transportation and growing economies have made traveling more efficient and accessible. This progress has resulted in a surge of international travel, including travel to remote destinations and lower-income countries ( 1 ). In 2019, a record 2.4 billion international tourist arrivals globally ( 2 ) were observed by the World Tourism Organization.
Four studies estimated that 43%–79% of travelers to low- and middle-income countries became ill with a travel-related health problem, some of whom needed medical care during or after travel ( 3 ). Certain groups (e.g., travelers visiting friends and relatives [VFRs] and migrants) are particularly at risk for acquiring travel-related diseases because of a lack of risk awareness, access to specialized health care and pretravel consultation, and trust in the health care system ( 4 , 5 ). In addition, travelers might introduce pathogens into new environments and populations, leading to the spread of novel and emerging infectious diseases ( 6 ). The 2019 measles outbreaks across Europe illustrated how travel and poor vaccination coverage among local populations can fuel an epidemic ( 7 ). These outbreaks resulted in the importation of measles to communities with low vaccination coverage in the United States, a country that had eliminated measles in 2000. The rapid spread of disease across international borders also was observed during the Ebola virus disease epidemic in West Africa during 2014–2016 ( 8 ) as well as during the COVID-19 pandemic ( 9 ). These events illustrate the dangers of introducing pathogens into geographic clusters of susceptible populations as well as the importance of vaccination and other preventative strategies to reduce the risk for importation and spread.
Studying illness among travelers improves case identification, clinical management, and public health prevention strategies and also helps to characterize the epidemiology of diseases and control their spread ( 10 ). Because international travel continues to increase, conducting surveillance and research regarding travel-related diseases will be instrumental in reducing global transmission. To identify travel-related diseases and facilitate rapid communication between clinicians and public health professionals globally, a surveillance system (e.g., GeoSentinel) is needed. Such connectivity can reduce the size of outbreaks while promoting the timely sharing of clinical insight regarding the diagnosis and treatment of patients.
The GeoSentinel Network (GeoSentinel) is a global, clinical-care–based surveillance and research network of travel and tropical medicine sites that monitors infectious diseases and other adverse health events that affect international travelers ( https://geosentinel.org/ ). Since its inception in 1995, GeoSentinel has remained at the forefront of travel-related sentinel surveillance and continues to refine its collection of epidemiologic data from ill travelers during and after travel.
This report describes GeoSentinel, key changes in its data collection, its successful detection of sentinel events, and future directions. This report also summarizes the data collected from migrants and returning U.S. nonmigrant travelers presenting for evaluation at a U.S. GeoSentinel site during 2012–2021. The findings in this report underscore the importance of global travel-related disease surveillance so that clinicians and public health professionals are aware of the most common travel-related illnesses and can develop improved treatment and prevention strategies.
The GeoSentinel Network
GeoSentinel is a collaboration between CDC and the International Society of Travel Medicine (ISTM) and was established in the United States in 1995 with nine U.S. sites ( 11 ). During 1996–1997, the GeoSentinel network expanded globally. GeoSentinel’s primary purpose is to coordinate multiple clinical-care–based sites that operate a global, provider-based emerging infections sentinel network, conduct surveillance for travel-related infections, and communicate and help guide public health responses ( 12 ). Sites collaborate to report disease or population-specific findings through retrospective database analyses and the collection of supplemental data to fill specific knowledge gaps.
Sites and Affiliate Members
As of December 2021, GeoSentinel comprised 71 sites in 29 countries located on six continents ( Figure 1 ). GeoSentinel sites are health care facilities led by site directors and codirectors who are medical professionals with expertise in travel and tropical medicine. GeoSentinel also includes 164 affiliate members (formerly referred to as network members) who report sentinel or unusual travel medicine cases but do not enter data into the GeoSentinel database.
Eligible Patients
Patient data can be entered into the GeoSentinel database if the patient has crossed an international border and was seen at a GeoSentinel site with a possible travel-related illness or, in the case of certain migrants, for screening purposes upon entry into their arrival country. Data from patients who develop a complication from pretravel treatments (i.e., adverse effect from vaccinations or antimalarial medication) also might be entered, even if the patients have not yet departed on their trip.
Data Collection
GeoSentinel sites use a standardized data collection form (Supplementary Appendix, https://stacks.cdc.gov/view/cdc/127681 ) to collect demographic, clinical, and travel-related information about patients and the illnesses acquired during travel. These data are collected electronically via a secure web-based data entry application based at CDC. Daily reports are generated for assistance in detecting events (i.e., unusual patterns or clusters of disease). The system emails these reports to both CDC and ISTM partners for review. If an unusual disease pattern or cluster of disease is detected, the GeoSentinel program manager sends an email to the site requesting additional information. Electronic validation is integrated into the database to reduce data entry errors and maintain data integrity. Whereas certain sites enter all travel-related cases into the GeoSentinel database, other sites only enter a convenience sample. Entry of cases into the GeoSentinel database and determination of travel association are at the discretion of the treating clinician. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.* Ethics clearance has been obtained by sites as required by their respective institutions.
Selected Variables and Definitions
The GeoSentinel database contains information obtained from patients evaluated at GeoSentinel sites during and after international travel. The following definitions were used during the study period.
Citizen. A person who is a legally recognized national of a country.
Clinical setting. The timing of the visit related to travel.
- During travel. The trip related to the current illness is in progress. This category includes expatriates seen in their country of residence for illnesses likely acquired in that country or where the country of exposure cannot be ascertained.
- After travel. The trip related to the current illness has been completed. This category also includes expatriates who acquire an illness during travel outside their current country of residence and where the relevant exposure is related to travel.
Diagnosis and diagnosis type. Site directors choose from approximately 475 diagnoses classified as either etiologic or syndromic. A write-in option is available on the data collection form if the diagnosis is not on the list.
- Etiologic. This diagnosis type reflects a specific disease. The “diagnosis status” of etiologic diagnoses might be “confirmed” or “probable” (see Diagnosis status).
- Syndromic. This diagnosis type reflects symptom- or syndrome-based etiologies when a more specific etiology is not known or could not be determined as a result of use of empiric therapy, self-limited disease, or inability to justify additional diagnostic tests beyond standard clinical practice. The “diagnosis status” of all syndromic diagnoses is “confirmed” (see Diagnosis status).
Diagnosis status . The diagnosis is categorized in one of two ways on the basis of available diagnostic methods:
- Confirmed. The diagnosis has been made by an indisputable clinical finding (e.g., removal of larvae of tungiasis) or diagnostic test.
- Probable. The diagnosis is supported by evidence (including diagnostic testing) strong enough to establish presumption but not proof.
Expatriate. A person living in a destination with an independent residence and address and using the same infrastructure as local residents of the same economic class. Expatriates intend to remain in-country for ≥6 months and have no intention to legally change their citizenship or permanent residency status.
Main symptoms. The symptoms associated with the illness that was the reason for the clinic visit.
Migrant. A person who, at some time in their life, has emigrated from their country of birth and has previously or intends to legally change their citizenship or permanent residency status. The resident country is entered on the data collection form as the new home country.
Nonmigrant traveler. A person who is traveling for a purpose unrelated to migration.
Pretravel encounter. Any pretravel health visit or the receipt of travel-related health information.
Resident. A person who has their primary residence in a particular country.
Severity. The highest level of clinical care received for the travel-related diagnosis, including outpatient, inpatient ward, and inpatient intensive care unit (ICU) care.
Syndrome or system groupings of diagnoses. All GeoSentinel diagnoses are categorized into groups according to the type of syndrome or system affected ( Box 1 ).
Travel reason. Primary reason for travel related to the current illness ( Box 2 ).
Travel related. Designates the relation of the main diagnosis to the patient’s travel.
- Travel related. Used when the illness under evaluation, initially suspected to be travel-related, was determined to have been acquired during the patient’s travel.
- Imported infection. Used for infections acquired in the patient’s country of residence if exported to another country and then evaluated at a GeoSentinel site.
- Not travel related. Used when the illness under evaluation, initially suspected to be travel related, was determined to have been acquired before departure from or after returning to the home country.
- Not ascertainable . Used when the illness under evaluation, initially suspected to be travel related, was equally likely to have been acquired during the patient’s travel or before departing from or after returning to the residence country.
Changes to GeoSentinel Data Collection
During 2012–2021, multiple changes were made to the GeoSentinel data entry application ( Box 3 ). New fields and subfields that collect detailed information on patient types, diagnoses, and trip information were added to provide a complete profile of patients and their associated illnesses. Additional fields were added for diseases of interest to provide information (e.g., vaccination status, etiology [e.g., organism genus and species], and cause of death). Case definitions were developed for each diagnosis code, and data collection fields were refined on an ongoing basis to aid clinicians in classifying patients and diagnoses.
Internal validation is now used to ensure that data are collected uniformly and accurately among sites. The collection of diagnostic methods allows for validation of confirmed and probable cases, and quality assurance (QA) alerts prevent sites from classifying diagnoses as confirmed during data entry without required disease-specific diagnostic methods. Other QA alerts prevent the skipping of required fields as well as logical errors.
Before November 16, 2018, the variables of travel reason and exposure country (and region) were not linked to an individual diagnosis. Instances where patients had multiple unrelated diagnoses made it difficult to ascertain what information applied to which diagnosis. As a result, the data collection form and database were updated to specify travel reason and exposure country information for each individual diagnosis.
To fill knowledge gaps, enhanced surveillance projects were deployed throughout the analysis period to collect specific information about a disease or types of travelers that was not collected on the core data collection form. This included projects on antibiotic resistance for selected bacterial pathogens, rickettsioses, mass gatherings ( 13 ), rabies postexposure prophylaxis ( 14 ), planned and unplanned health care abroad ( 15 ), migrants ( 16 ), and respiratory illnesses related to COVID-19.
This report includes GeoSentinel data limited to unique patients with ≥1 confirmed or probable travel-related diagnosis who were evaluated after migration or travel at a GeoSentinel site in the United States during 2012–2021. Each patient might have multiple diagnoses. Patients must have been residents of the United States and evaluated after travel and within 10 years of migrating or returning from a trip outside of the United States. Only migrants with illnesses associated with their migration to the United States were included. The validity of diagnoses was verified by an infectious disease specialist using the diagnostic methods recorded by the sites. Descriptive analyses were performed on data from the 20 GeoSentinel sites in the United States ( Figure 2 ) with patients who met inclusion criteria. Frequencies were calculated on patient demographics (e.g., sex, age, country of birth, citizenship, and residence), travel-related information (e.g., reason for travel and country or region of exposure), diagnosis, diagnostic methods, year of illness onset, and severity of illness. Because of changes in the collection of travel-related information, a subanalysis was done on travel-related information before and after November 16, 2018. This information is reported separately. Geographic regions of exposure are classified based on modified UNICEF groupings ( https://data.unicef.org/regionalclassifications/ ). Data were managed using Microsoft Access (version 2208; Microsoft Corporation), and all analyses were performed using SAS (version 9.4; SAS Institute).
To demonstrate GeoSentinel’s ability to identify sentinel events and emerging disease patterns, three examples (i.e., dengue in Angola [2013], Zika in Costa Rica [2016], and yellow fever in Brazil [2018]) of emerging sentinel health threats that occurred during 2012–2021 are described. These health events were not limited to residents of the United States who were evaluated after travel and ≤10 years of migrating or returning from a trip outside of the United States. Therefore, these patients could be residents of any country and were seen at GeoSentinel sites both inside and outside of the United States.
During 2012–2021, a total of 198,120 unique patients were evaluated at GeoSentinel sites globally and included in GeoSentinel’s database ( Figure 3 ). Of these, 177,703 patients received at least one confirmed or probable travel-related diagnosis, of which 18,336 were reported from 20 GeoSentinel sites in the United States. Of the 17,538 patients evaluated by a clinician after travel, 17,389 were migrants or returning U.S. nonmigrant travelers to the United States, accounting for 25,973 travel-related diagnoses. The remaining 149 patients were non-U.S. residents and were excluded from the analysis. The results of migrants and returning nonmigrant travelers are reported separately.
Patient Demographics
Of the 17,389 patients who were included in this analysis, 7,530 (43.3%) were recent migrants to the United States; <1% of patients were expatriates. Of 7,527 migrants, 47.4% were female ( Table 1 ). The median age was 28.5 years (range = <19 years to 93 years), and the largest proportion of migrants was aged 19–39 years (35.9%). Of 4,672 patients with information available, 88.8% did not receive pretravel health information. Of 2,867 patients with information available on severity, a majority (89.8%) were seen as outpatients, 9.7% were seen in an inpatient ward, and <1% were seen in an ICU.
Of the 13,986 travel-related diagnoses among migrants, the most frequent were vitamin D deficiency (20.2%), Blastocystis (10.9%), latent tuberculosis (10.3%), strongyloidiasis (6.7%), and eosinophilia (5.8%) ( Table 2 ). A total of 43% of diagnoses fell into eight infectious or travel-related syndrome groupings including “other” (18.7%), gastrointestinal (15.7%), dermatological (2.0%), neurologic (1.9%), genitourinary (1.6%), febrile (1.5%), respiratory (1.5%), and musculoskeletal (<1%). No deaths or animal bites or scratches were reported ( Table 3 ).
Of the 2,614 diagnoses in the “other” grouping (Table 3), the most frequent were latent tuberculosis (55.2%), eosinophilia (30.8%), Chagas disease (3.8%), posttraumatic stress disorder (3.6%), and depression (2.9%). Of the 2,202 diagnoses in the gastrointestinal grouping, the most frequent were simple intestinal strongyloidiasis (41.6%), giardiasis (18.9%), Helicobacter pylori infection (8.4%), dientamoebiasis (6.9%), and schistosomiasis (6.5%). Of the 275 diagnoses in the dermatological grouping, the most frequent were fungal infection (42.6%), insect bite/sting (10.9%), rash of unknown etiology (10.2%), cutaneous leishmaniasis (5.8%), and leprosy (4.4%). Of the 263 diagnoses in the neurologic grouping, the most frequent were neurocysticercosis (76.8%), headache (16.4%), ataxia (1.5%), central nervous system tuberculosis (1.5%), and tuberculosis meningitis (1.1%). Of the 229 diagnoses in the genitourinary grouping, the most frequent were schistosomiasis (27.5%), chlamydia (15.3%), syphilis (11.4%), urinary tract infection (10.9%), and HIV (10.0%).
Among the 212 diagnoses in the febrile grouping (Table 3), the most frequent were malaria (25.5%), other extrapulmonary tuberculosis (13.2%), toxoplasmosis (8.0%), tuberculosis lymphadenitis (6.6%), and disseminated tuberculosis (5.2%). Malaria was diagnosed in 54 (<1%) migrants, and 88.5% did not receive pretravel health information (information available for 26 migrants). Of all species of malaria, Plasmodium falciparum was diagnosed most frequently (77.4%).
Among the 204 diagnoses in the respiratory grouping (Table 3), the most frequent was pulmonary tuberculosis (70.6%), which accounted for 68.9% of all active tuberculosis diagnoses; only 1% of migrants received a diagnosis of active tuberculosis disease. The remaining frequent diagnoses in the respiratory grouping were acute otitis media (4.9%), atypical pneumonia (3.4%), otitis externa (2.9%), and unspecified lobar pneumonia (2.9%). Of the 131 diagnoses in the musculoskeletal grouping, the most frequent were arthralgia (48.1%), trauma or injury (43.5%), osteomyelitis (1.5%), knee pain (1.5%), and sprain (1.5%).
Diagnostic Characteristics Before November 16, 2018
Among the 2,892 diagnoses with information available ( Table 4 ), the five most frequent regions of exposure were Sub-Saharan Africa (22.7%), the Caribbean (21.3%), Central America (13.4%), South East Asia (13.1%), and South Central Asia (9.2%). Among the 2,554 diagnoses with information available, the most frequent countries of exposure were Dominican Republic (7.9%), Thailand (6.5%), Haiti (6.2%), Ecuador (4.8%), and Myanmar (4.3%). Of 46 migrants with a malaria diagnosis, 89.3% were exposed in Sub-Saharan Africa (information available for 28 migrants).
Diagnostic Characteristics After November 16, 2018
Among the 2,012 diagnoses with information available (Table 4), the five most frequent regions of exposure were Central America (27.6%), Sub-Saharan Africa (26.2%), South East Asia (16.9%), the Caribbean (8.4%), and South America (7.0%). Among the 1,575 diagnoses with information available, the most frequent countries of exposure were El Salvador (11.2%), Thailand (10.7%), Honduras (9.1%), Guatemala (7.6%), and Dominican Republic (5.9%). Of seven migrants with a malaria diagnosis, all were exposed in Sub-Saharan Africa (information available for seven migrants).
Returning Nonmigrant Travelers
Among the 9,859 nonmigrant travelers returning to the United States, 55.7% were female and 75.3% were born in the United States. The median age was 37 years (range = <19 years to 96 years), and the largest proportion of nonmigrant travelers was aged 19–39 years (44.1%). Among the 8,967 patients with information available, 65.6% did not receive pretravel health information. Among the 5,884 patients with information available on severity, a majority (90.6%) were seen as outpatients, 8.4% were seen in an inpatient ward, and <1% were seen in an ICU. Approximately 1% of patients were expatriates, and 89.4% were U.S. citizens.
Of the 11,987 travel-related diagnoses of returning U.S. nonmigrant travelers (Table 3), 90.7% of diagnoses fell into nine infectious or travel-related syndrome groupings, including gastrointestinal (43.2%), febrile (16.7%), respiratory (13.0%), dermatological (8.9%), “other” (4.1%), animal bites or scratches (1.3%), genitourinary (1.4%), musculoskeletal (1.2%), and neurologic (<1%). The most frequent diagnoses (Table 2) were acute diarrhea (16.9%), viral syndrome (4.9%), irritable bowel syndrome (4.1%), campylobacteriosis (3.1%), and malaria (3.5%). Four deaths were reported, of which two were patients who received a diagnosis of severe P. falciparum malaria. Of the remaining two patients, one received a diagnosis of COVID-19 and the other received a diagnosis of acute unspecified hepatitis with renal failure.
Among the 5,173 diagnoses in the gastrointestinal grouping (Table 3), the most frequent were acute diarrhea (39.3%), irritable bowel syndrome (9.5%), campylobacteriosis (7.2%), giardiasis (5.5%), and chronic diarrhea (5.2%). Among the 2,001 diagnoses in the febrile grouping, the most frequent were viral syndrome (29.0%), malaria (21.0%), dengue (13.7%), chikungunya (6.4%), and unspecified febrile illness (5.0%). Among the 421 nonmigrant travelers with malaria of any species diagnosed, 80.8% had P. falciparum .
Among the 1,554 diagnoses in the respiratory grouping (Table 3), the most frequent were influenza-like illness (16.5%), upper respiratory tract infection (14.9%), acute bronchitis (11.9%), acute sinusitis (9.1%), and unspecified lobar pneumonia (8.4%). Among the 1,071 diagnoses in the dermatological grouping, the most frequent were insect or arthropod bite or sting (31.3%), rash of unknown etiology (8.8%), dermatitis (7.9%), skin and soft tissue infection (e.g., erysipelas, cellulitis, or gangrene [7.4%]), and superficial skin and soft tissue infection (6.0%). Among the 487 diagnoses in the “other” grouping, the most frequent were dehydration (18.7%), jet lag (17.9%), eosinophilia (11.7%), latent tuberculosis (8.8%), and anxiety disorder (7.6%).
Among the 173 diagnoses in the genitourinary grouping (Table 3), the most frequent were urinary tract infection (33.0%), schistosomiasis (11.6%), gonorrhea (9.3%), pyelonephritis (8.7%), and genital chlamydia (8.1%). Among the 142 diagnoses in the musculoskeletal grouping, the most frequent were arthralgia (19.7%), fracture (17.6%), myalgia (10.6%), trauma or injury (9.9%), and contusion (7.8%). Among the 105 diagnoses in the neurologic grouping, the most frequent were headache (26.7%), vertigo (12.4%), acute mountain sickness (10.5%), neurocysticercosis (9.5%), and dizziness (8.6%). Among the 153 diagnoses of bites or scratches, the most frequent were dog bite (50.3%), monkey bite (18.3%), other animal bite (6.5%), monkey exposure (5.9%), and dog exposure (3.9%).
Among the 9,919 diagnoses, 6,518 had information regarding travel reason ( Table 5 ). The most frequent reasons for travel were tourism (44.8%), VFR (22.0%), and business (13.4%). Among the 6,296 diagnoses with information available, the five most frequent regions of exposure were Central America (19.2%), Sub-Saharan Africa (17.7%), the Caribbean (13.0%), South East Asia (10.4%), and South America (9.4%). Among 5,920 diagnoses with information available, the most frequent countries of exposure were Mexico (12.5%), India (7.2%), Dominican Republic (5.3%), China (3.3%), and Costa Rica (3.0%).
Of 300 nonmigrant travelers with malaria, 70.3% were VFRs (information available for 232 nonmigrant travelers), and 88.6% were exposed in Sub-Saharan Africa. Of 163 VFRs with malaria, 70.2% did not receive pretravel health information (information available for 141 nonmigrant travelers), and 88.3% did not take malaria chemoprophylaxis (information available for 103 nonmigrant travelers).
Information regarding travel reason and exposure region was available for all 2,068 diagnoses (Table 5). The most frequent reasons for travel were tourism (53.6%), VFR (21.4%), business (12.3%), and missionary (6.2%). The five most frequent regions of exposure were Sub-Saharan Africa (25.5%), Central America (17.3%), South East Asia (11.2%), the Caribbean (10.9%), and South Central Asia (9.0%). Among the 1,894 diagnoses with information available, the most frequent countries of exposure were Mexico (13.2%), India (5.0%), Dominican Republic (4.2%), Philippines (3.0%), and Ethiopia (3.0%).
Of 121 nonmigrant travelers with malaria, 57.9% were VFRs and 95.9% were exposed in Sub-Saharan Africa. Of 70 VFRs with malaria, 83.3% did not receive pretravel health information (information available for 54 nonmigrant travelers), and none took malaria chemoprophylaxis (information available for three nonmigrant travelers).
Dengue in Angola, 2013
During April–May 2013, GeoSentinel sites in Canada, France, Germany, Israel, and South Africa reported 10 cases of dengue among travelers returning from Luanda, Angola. All patients had classic symptoms of dengue that included headache and joint pain and recovered without complication. Although dengue is endemic in Angola, before 2013, the last outbreak occurred during the 1980s. In the decades that followed, little was known regarding the epidemiology of dengue in Angola because of poor surveillance ( 17 ).
Although six cases of dengue had been reported to the Ministry of Health of Angola by April 1, 2013, the GeoSentinel cases, in combination with other imported cases to Portugal, were among the first indications of a large-scale outbreak. By May 31, there were 517 suspected cases and one death reported; all but two cases were in Luanda province ( 18 ). The GeoSentinel cases in Angola demonstrated that data on travelers’ adverse health events can aid in the detection of outbreaks, offering insight into the epidemiology of infectious disease in countries with suboptimal surveillance and reporting.
Zika in Costa Rica, 2016
On January 26, 2016, a GeoSentinel site in Massachusetts diagnosed dengue in a returned U.S. traveler from Nosara, Costa Rica. The patient returned to the United States with fever, rash, conjunctivitis, arthralgia, and headache; the patient also reported multiple mosquito bites. The patient was referred to a GeoSentinel site where antibody tests for Zika and dengue viruses were conducted by CDC. Plaque reduction neutralization antibody testing confirmed a diagnosis of Zika ( 19 ).
Zika virus emerged in the western hemisphere during 2014–2016 when outbreaks were reported from certain countries in the Americas and Caribbean ( 20 ). This case was the first case of Zika reported from Costa Rica, illustrating the continual geographic spread of a high-consequence pathogen. The Massachusetts GeoSentinel site detected and reported this sentinel case, and it also sent a networkwide notification, alerting clinicians to the risk for Zika in Costa Rica, a popular travel destination with no previous evidence of underlying circulation. By August 2017, a total of 1,920 cases were reported in Costa Rica, mirroring the trends of other countries in the region.
Yellow Fever in Brazil, 2018
In January 2018, a GeoSentinel site in the Netherlands reported a case of yellow fever in a Dutch man aged 46 years with recent travel to São Paulo state, Brazil. He had signs and symptoms of diarrhea, fever, headache, myalgia, and vomiting. By March 15, 2018, four additional GeoSentinel sites reported cases of yellow fever among travelers returning from Brazil, including two deaths. These five cases accounted for one half of all cases reported among international travelers to Brazil during this time. All patients were unvaccinated travelers, many of whom visited Ilha Grande ( 21 ).
Although yellow fever is endemic in Brazil, during 2016–2017 and 2017–2018, a higher incidence does not, by itself, indicate geographic expansion ( 22 ). Cases detected by GeoSentinel in early 2018 were among the first reported in newly identified regions of risk, confirming travelers as sentinels in the expansion of the outbreak and highlighting the importance of yellow fever vaccination in recommended regions ( 21 ).
GeoSentinel is the only surveillance network that operates a global, provider-based emerging infections sentinel network to conduct surveillance for travel-related infections and communicates with public health and clinical partners ( 11 ). From its inception in 1995 to 2011 ( 11 ), efforts were made to increase the size of the network, modernize data collection, and introduce internal validation to improve the quality of the data collected. Since 2012, GeoSentinel has expanded to 71 sites on six continents and has generated approximately 70 peer-reviewed publications. GeoSentinel also has undergone numerous methodologic changes aimed to improve data collection, the validity of resulting conclusions, and the provision of public health recommendations.
GeoSentinel data have been instrumental in the detection of sentinel events, as demonstrated by, but not limited to, the detection of expanded geographic area of yellow fever in Brazil ( 21 ), a large outbreak of dengue in Angola ( 17 ), and the first case of Zika in Costa Rica ( 19 ). These examples illustrate GeoSentinel’s ability to both identify emerging pathogens and communicate findings with clinicians and public health professionals around the world.
The most frequent diagnoses among migrants described in this analysis (e.g., vitamin D deficiency and latent tuberculosis) have been described elsewhere ( 23 , 24 ). Vitamin D deficiency might be because of reduced sun exposure caused by skin-covering clothing as well as low dietary intake ( 23 ). Acquisition of strongyloidiasis and latent tuberculosis might be from crowding, malnutrition, exposure to unsafe food and water, inadequate sanitation, and limited access to health care ( 25 ). Multiple presentations of Mycobacterium tuberculosis (e.g., pulmonary, extrapulmonary, lymphadenitis, disseminated, CNS tuberculoma, and meningitis) also were reported among migrants, highlighting that health care professionals should maintain a high degree of suspicion for M. tuberculosis infection among ill patients whose routine bacterial cultures do not yield a pathogen. Because the United States has the largest population of migrants in the world ( 26 ), health care professionals should continue to advocate for medical care for this underserved population, with the aim to prevent disease reactivation and subsequent spread to and within vulnerable populations.
Gastrointestinal illnesses remain a frequent cause of illness among travelers ( 27 ). In this analysis, acute diarrhea was the most frequent illness among nonmigrant travelers, accounting for 16.9% of their diagnoses. Previous studies have reported attack rates for acute diarrhea among travelers ranging from 30%–70%, most often caused by bacterial pathogens and transmitted because of poor hygiene practices in local restaurants ( 28 ). In other studies, travelers have reported not adhering to prevention practices and drinking unsafe tap water, consuming drinks with ice, eating salads, and consuming unpasteurized dairy products while abroad ( 29 ). Most acute diarrhea cases reported to GeoSentinel were of unknown etiology, illustrating the lack of use of specialized diagnostic tests or culture to determine the cause of diarrhea ( 30 ), despite the widespread availability of multiplex polymerase chain reaction tests for gastrointestinal pathogens ( 31 ), likely because the majority of cases of acute diarrhea resolve without the need for intervention ( 32 ).
Febrile illnesses were another frequent cause of illness among nonmigrant travelers in this analysis, of which viral syndromes and P. falciparum malaria were most frequent. Of nonmigrant travelers with malaria, a majority were exposed in Sub-Saharan Africa; the majority were VFRs, who infrequently received pretravel health advice or took malaria chemoprophylaxis. Inadequate pretravel preparation practices place VFRs at high risk for acquiring malaria during travel. Studies of African VFR travelers indicated they might not be able to afford health care visits, might feel unable to advocate for themselves in a health care setting, and might be culturally opposed to malaria chemoprophylaxis or other preventive measures (e.g., use of bed nets) because of concerns about offending their hosts or a low perception of risk ( 33 , 34 ). CDC recommends that all travelers going to an area where malaria is endemic take chemoprophylaxis before and during travel ( 35 ), but special considerations (e.g., improving accessibility or improving trust in the U.S. health care system) could be prioritized to ensure that VFRs are protected from malaria ( 33 , 36 ).
COVID-19 Pandemic
During 2020–2021, the number of patients presenting at U.S. GeoSentinel sites substantially decreased, mirroring worldwide declines in travel because of the COVID-19 pandemic and associated travel restrictions. Although GeoSentinel historically has been lauded for its ability to detect sentinel events in real time, GeoSentinel only retrospectively identified cases of influenza-like illness as COVID-19 among travelers who returned from China early in the pandemic. Although the outbreak began in China, a popular destination for U.S. travelers, in late 2019, U.S. GeoSentinel sites first reported COVID cases among travelers in March 2020. This lack of early identification of COVID-19 cases was likely because of three main reasons. First, daily reports were generated for assistance in detecting sentinel events, but these were simple line listings of cases and focused primarily on etiologic diagnoses; although cases of “viral illness” were reported from China to GeoSentinel as early as December 2019, these were not identified to be out of the ordinary. Surveillance systems (e.g., GeoSentinel) are most effective in detecting established etiologic illnesses, not novel pathogens ( 37 ). Second, delays in identification and available diagnostics for this novel pathogen meant that testing was not routinely available globally or at GeoSentinel sites early in the pandemic; therefore, etiologic COVID-19 diagnoses were only made retrospectively. Third, many cases of COVID-19 might have had mild symptoms similar to influenza, the common cold, and seasonal allergies, whose symptoms can be treated with over-the-counter medication. Thus, ill travelers might have opted to treat their symptoms at home and not seek health care or visited their primary care provider instead of a travel and tropical medicine site despite their recent travel.
To address these challenges, GeoSentinel has begun to explore other ways to detect and track novel pathogens more rapidly. GeoSentinel is developing automated, real-time data analytics (e.g., machine learning algorithms by likelihood of outbreak origin) to improve the ability to detect outbreaks and unusual clusters of disease together with more classical surveillance approaches ( 38 ).
The findings in this report are subject to at least six limitations. First, GeoSentinel data are not representative of all travelers. Although GeoSentinel tracks illnesses among travelers who are treated at GeoSentinel sites, data are entered at the discretion of the sites, which might lead to underreporting. Second, sites are not evenly dispersed globally and are predominantly located in Europe and North America. This pattern might reflect the travel attributes of persons from these continents. Third, GeoSentinel only collects data on ill travelers who seek care at GeoSentinel sites. The total numbers of travelers, ill travelers who do not seek care, or travelers who seek care outside of the GeoSentinel network is unknown. Thus, GeoSentinel data cannot be used to estimate risk, incidence, prevalence, or other rates because the number of well or unexposed travelers in the denominator is not known. Fourth, the United States does not have many large travel and tropical medicine centers (in comparison with Europe or Asia) and travelers, including migrants, might seek care external to the GeoSentinel network. Fifth, although changes in the information collected, methods, and the sites themselves have made data collection more robust, these changes also make the comparison of periods difficult and, in certain cases, inappropriate. Although all sites use the same standardized data collection form, data entry practices vary by site and over time. Finally, the large number of migrants reported from U.S. GeoSentinel sites might be the result of selection bias because of the migration medicine specialization of many U.S. sites. Diseases detected among migrants might be driven by routine screening on entry to the United States.
As of September 2021, GeoSentinel has incorporated research through its cooperative agreement between CDC and ISTM. This will allow GeoSentinel to conduct hypothesis-driven studies to help guide clinical and public health recommendations. Initial projects include investigation of fever of unknown etiology among travelers, neurocognitive outcomes among travelers with malaria, kinetics of human Mpox infections, and exploration of the distribution and types of antimalarial resistance using malaria genomics.
Over the past decade, GeoSentinel has contributed to the early detection of diseases among international travelers. The information about demographics, traveler types, and frequent diagnoses provides data that clinicians and public health agencies can use to improve pretravel preparedness and enhance guidance for the evaluation and treatment of ill travelers who seek medical care after international travel. The key successes and shortcomings of GeoSentinel serve as references to improve surveillance and expand the capability to detect sentinel events.
The following active members of the GeoSentinel Network contributed data from U.S. sites: Susan Anderson (Palo Alto, California); Kunjana Mavunda (Miami, Florida); Ashley Thomas (Orlando, Florida); Henry Wu (Atlanta, Georgia); Johnnie Yates (Honolulu, Hawaii); Noreen Hynes (Baltimore, Maryland); Anne Settgast, Bill Stauffer (St. Paul, Minnesota); Elizabeth Barnett (Boston, Massachusetts); Christina Coyle, Paul Kelly, Cosmina Zeana (Bronx, New York); John Cahill, Marina Rogova, Ben Wyler; (New York, New York); Terri Sofarelli (Salt Lake City, Utah). All maps were contributed by Marielle Glynn.
Corresponding author: Ashley B. Brown, Division of Global Migration and Quarantine, National Center for Emerging and Zoonotic Infectious Disease, CDC. Telephone: 678-315-3279; Email: [email protected] .
1 Division of Global Migration and Quarantine, National Center for Emerging and Zoonotic Infectious Disease, CDC; 2 Department of Global Health, Boston University School of Public Health, Boston, Massachusetts; 3 Section of Infectious Disease, Department of Medicine, Boston University Chobanian & Avedisian School of Medicine, Boston, Massachusetts; 4 Division of Infectious Diseases (Emerita), Department of Medicine, Emory University, Atlanta, Georgia; 5 J.D. MacLean Centre for Tropical Diseases, McGill University, Montreal, Canada; 6 Department of Infectious Tropical Diseases and Microbiology, IRCCS Sacro Cuore Don Calabria Hospital, Negrar, Verona, Italy; 7 GeoSentinel, International Society of Travel Medicine, Alpharetta, Georgia; 8 Department of Medicine, Emory University School of Medicine, Atlanta, Georgia; 9 Department of Medicine, Mount Auburn Hospital, Cambridge, Massachusetts; 10 Harvard Medical School, Boston, Massachusetts; 11 Division of Infectious Diseases, University of Utah School of Medicine, Salt Lake City, Utah; start highlight 12 Department of Psychology, Colorado State University, Fort Collins, Colorado; end highlight 13 Infectious Diseases, Orlando Health Medical Group, Orlando, Florida
Conflicts of Interest
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
- Glaesser D, Kester J, Paulose H, Alizadeh A, Valentin B. Global travel patterns: an overview. J Travel Med 2017;24:1–5. https://doi.org/10.1093/jtm/tax007 PMID:28637267
- World Tourism Organization. Yearbook of tourism statistics, data 2015–2019, 2021 edn. Madrid, Spain: World Tourism Organization; 2021. https://www.e-unwto.org/doi/book/10.18111/9789284422487
- Angelo KM, Kozarsky PE, Ryan ET, Chen LH, Sotir MJ. What proportion of international travellers acquire a travel-related illness? a review of the literature. J Travel Med 2017;24:1–8. https://doi.org/10.1093/jtm/tax046 PMID:28931136
- Kozarsky PE, Keystone JS. VFR (visiting friends and relatives) travelers [Chapter 5]. In: Schwartz E, ed. Tropical diseases in travelers. Chichester, UK: Wiley-Blackwell; 2010: 35–44.
- Ghent A. Overcoming migrants’ barriers to health. Bull World Health Organ 2008;86:583–4. https://doi.org/10.2471/BLT.08.020808 PMID:18797611
- Findlater A, Bogoch II. Human mobility and the global spread of infectious diseases: a focus on air travel. Trends Parasitol 2018;34:772–83. https://doi.org/10.1016/j.pt.2018.07.004 PMID:30049602
- Angelo KM, Gastañaduy PA, Walker AT, et al. Spread of measles in Europe and implications for US travelers. Pediatrics 2019;144:e20190414. https://doi.org/10.1542/peds.2019-0414 PMID:31209161
- CDC, Guinea Interministerial Committee for Response Against the Ebola Virus, World Health Organization, Liberia Ministry of Health and Social Welfare, Sierra Leone Ministry of Health and Sanitation. Update: Ebola virus disease epidemic—West Africa, February 2015. MMWR Morb Mortal Wkly Rep 2015;64:186–7. PMID:25719681
- Keni R, Alexander A, Nayak PG, Mudgal J, Nandakumar K. COVID-19: emergence, spread, possible treatments, and global burden. Front Public Health 2020;8:216. https://doi.org/10.3389/fpubh.2020.00216 PMID:32574299
- Chen LH, Wilson ME. The role of the traveler in emerging infections and magnitude of travel. Med Clin North Am 2008;92:1409–32, xi. https://doi.org/10.1016/j.mcna.2008.07.005 PMID:19061759
- Harvey K, Esposito DH, Han P, et al.; CDC. Surveillance for travel-related disease—GeoSentinel Surveillance System, United States, 1997–2011. MMWR Surveill Summ 2013;62(No. SS-3):1–23. PMID:23863769
- Hamer DH, Rizwan A, Freedman DO, Kozarsky P, Libman M. GeoSentinel: past, present and future. Alpharetta, GA: International Society of Travel Medicine, Journal of Travel Medicine; 2020. https://academic.oup.com/jtm/article/27/8/taaa219/6007543
- Gautret P, Angelo KM, Asgeirsson H, et al.; GeoSentinel Network. International mass gatherings and travel-associated illness: a GeoSentinel cross-sectional, observational study. Travel Med Infect Dis 2019;32:101504. https://doi.org/10.1016/j.tmaid.2019.101504 PMID:31707112
- Gautret P, Angelo KM, Asgeirsson H, et al.; GeoSentinel Global Surveillance Network. Rabies post-exposure prophylaxis started during or after travel: a GeoSentinel analysis. PLoS Negl Trop Dis 2018;12:e0006951. https://doi.org/10.1371/journal.pntd.0006951 PMID:30422981
- Chen LH, Piyaphanee W, Diaz-Menendez M, et al. Unplanned healthcare during travel: a descriptive analysis from the GeoSentinel Network [Abstract 1398]. In: Proceedings of the American Society of Tropical Medicine and Hygiene Annual Conference; November 18, 2020; Toronto, Canada. Arlington, VA: American Society of Tropical Medicine and Hygiene.
- Barnett ED, Mccarthy A, Coyle CM, et al. Global surveillance of infectious diseases in migrants by the GeoSentinel network [Abstract 110]. In: Proceedings of the International Conference on Migration Health; October 2, 2018: Rome, Italy. Dunwoody, GA: International Society of Travel Medicine.
- Schwartz E, Meltzer E, Mendelson M, et al. Detection on four continents of dengue fever cases related to an ongoing outbreak in Luanda, Angola, March to May 2013. Euro Surveill 2013;18:20488. https://doi.org/10.2807/ese.18.21.20488-en PMID:23725977
- CDC. Ongoing dengue epidemic—Angola, June 2013. MMWR Morb Mortal Wkly Rep 2013;62:504–7. PMID:23784016
- Chen LH. Zika virus infection in a Massachusetts resident after travel to Costa Rica: a case report. Ann Intern Med 2016;164:574–6. https://doi.org/10.7326/L16-0075 PMID:26864175
- Hamer DH, Barbre KA, Chen LH, et al.; GeoSentinel Surveillance Network. Travel-associated Zika virus disease acquired in the Americas through February 2016: a GeoSentinel analysis. Ann Intern Med 2017;166:99–108. https://doi.org/10.7326/M16-1842 PMID:27893080
- Hamer DH, Angelo K, Caumes E, et al. Fatal yellow fever in travelers to Brazil, 2018. MMWR Morb Mortal Wkly Rep 2018;67:340–1. https://doi.org/10.15585/mmwr.mm6711e1 PMID:29565840
- World Health Organization. Yellow fever—Brazil. Geneva, Switzerland: World Health Organization; 2019. https://www.who.int/emergencies/disease-outbreak-news/item/18-april-2019-yellow-fever-brazil-en
- Lips P, de Jongh RT. Vitamin D deficiency in immigrants. Bone Rep 2018;9:37–41. https://doi.org/10.1016/j.bonr.2018.06.001 PMID:30591925
- Dhavan P, Dias HM, Creswell J, Weil D. An overview of tuberculosis and migration. Int J Tuberc Lung Dis 2017;21:610–23. https://doi.org/10.5588/ijtld.16.0917 PMID:28482955
- Castelli F, Sulis G. Migration and infectious diseases. Clin Microbiol Infect 2017;23:283–9. https://doi.org/10.1016/j.cmi.2017.03.012 PMID:28336382
- McAuliffe M, Triandafyllidou A, eds. World migration report 2022. Geneva, Switzerland: International Organization for Migration; 2021. https://publications.iom.int/books/world-migration-report-2022
- Leder K, Torresi J, Libman MD, et al.; GeoSentinel Surveillance Network. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med 2013;158:456–68. https://doi.org/10.7326/0003-4819-158-6-201303190-00005 PMID:23552375
- Conner B. Travelers’ diarrhea [Chapter 2]. In: Brunette GW, Nemhauser JB, eds. CDC yellow book 2020: health information for international travel. New York, NY: Oxford University Press; 2019.
- Stoney RJ, Han PV, Barnett ED, et al. Travelers’ diarrhea and other gastrointestinal symptoms among Boston-area international travelers. Am J Trop Med Hyg 2017;96:1388–93. https://doi.org/10.4269/ajtmh.16-0447 PMID:28719282
- Leder K, Torresi J, Libman MD, et al. ; GeoSentinel Surveillance Network. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med 2013;158:456–68. https://doi.org/10.7326/0003-4819-158-6-201303190-00005 PMID:23552375
- Vila J. New molecular diagnostic tools in traveller’s diarrhea. J Travel Med 2017;24(suppl_1):S23–8. https://doi.org/10.1093/jtm/taw071 PMID:28520995
- Diemert DJ. Prevention and self-treatment of traveler’s diarrhea. Clin Microbiol Rev 2006;19:583–94. https://doi.org/10.1128/CMR.00052-05 PMID:16847088
- Walz EJ, Volkman HR, Adedimeji AA, et al. Barriers to malaria prevention in US-based travellers visiting friends and relatives abroad: a qualitative study of West African immigrant travellers. J Travel Med 2019;26:tay163. https://doi.org/10.1093/jtm/tay163 PMID:30602033
- Neave PE, Behrens RH, Jones COH. “You’re losing your Ghanaianess”: understanding malaria decision-making among Africans visiting friends and relatives in the UK. Malar J 2014;13:287. https://doi.org/10.1186/1475-2875-13-287 PMID:25064713
- Tan KR, Arguin PM. Malaria [Chapter 4]. In: Brunette GW, Nemhauser JB. CDC yellow book 2020: health information for international travel. New York, NY: Oxford University Press; 2019:267.
- Volkman HR, Walz EJ, Wanduragala D, et al. Barriers to malaria prevention among immigrant travelers in the United States who visit friends and relatives in sub-Saharan Africa: a cross-sectional, multi-setting survey of knowledge, attitudes, and practices. PLoS One 2020;15:e0229565. https://doi.org/10.1371/journal.pone.0229565 PMID:32163426
- Christaki E. New technologies in predicting, preventing and controlling emerging infectious diseases. Virulence 2015;6:558–65. https://doi.org/10.1080/21505594.2015.1040975 PMID:26068569
- Dai Y, Wang J. Identifying the outbreak signal of COVID-19 before the response of the traditional disease monitoring system. PLoS Negl Trop Dis 2020;14:e0008758. https://doi.org/10.1371/journal.pntd.0008758 PMID:33001985
FIGURE 1 . GeoSentinel sites and affiliate members — GeoSentinel Network, 2012–2021*
* Sites = 71; affiliate members = 164.
BOX 1 . Syndrome and system groupings of diagnoses for surveillance — GeoSentinel Network, 2012–2021
- Adverse events to medication or vaccine
- Animal bites or scratches
- Dermatological: infectious or potentially travel related
- Dermatological: preexisting or chronic disease or comorbidity
- Febrile or systemic syndrome
- Gastrointestinal: infectious or potentially travel related
- Gastrointestinal: preexisting or chronic disease or comorbidity
- Genitourinary and STDs: infectious or potentially travel related
- Genitourinary and STDs: pre-existing or chronic disease or comorbidity
- Musculoskeletal: infectious or potentially travel related
- Musculoskeletal: pre-existing or chronic disease or comorbidity
- Neurological: infectious or potentially travel related
- Neurological: preexisting or chronic disease or comorbidity
- Other:* infectious or potentially travel related
- Other:* chronic disease or comorbidity
- Respiratory or ENT: infectious or potentially travel related
- Respiratory or ENT: pre-existing or chronic disease or comorbidity
Abbreviations: ENT = ears, nose, and throat; STD = sexually transmitted disease.
* Diseases that do not fall into system groupings.
BOX 2 . Reason for travel — GeoSentinel Network, 2012–2021
- Tourism (vacation): Includes all travel for tourism or leisure. Also includes travel that might involve visiting friends and relatives overseas if the traveler is not a first- or second-generation immigrant returning to his or her country of origin.
- ° Conference: Travel by an employed person for the purpose of attending a conference or convention
- ° Corporate or professional: Travel by an employed person for the purpose of carrying out business, attending meetings, or other work-related events
- ° Business or occupational — research: Travel by an employed person for the purpose of field work, laboratory work, or other type of academic research
- ° Business or occupational — other: Travel for the purpose of business or as part of one’s occupation but where the travel does not fit in the other specific categories of research, study, conference, or seasonal migrant work
- Seasonal or temporary work (migrant worker): Travel for the purpose of pursuing seasonal or other nonpermanent work because of economic opportunities in countries other than the person’s country of birth or place or permanent residence. These persons usually do not have any intention or permission to stay permanently in the country or region in which they are working.
- Student: Travel by a student for the purpose of study abroad, attending a student conference, research, or other educational purpose
- Migration: Main reason for travel is intent or need to resettle outside of birth country or country of secondary migration
- Providing medical care: Travel for the purpose of providing medical care
- VFR: Person is traveling from the region in which they are currently residing (usually as a migrant, expatriate, or long-term visitor) to their region of origin (e.g., a low-income country) to visit friends and relatives. This reason for travel includes persons who are travelling with a child/grandchild (second-generation VFRs) or parent and those traveling with a spouse or partner.
- Military: Main purpose is deployment to the country visited or to participate in military operations
- Missionary, humanitarian aid, volunteer, or community service: Travel to perform humanitarian work, community service, or take part in volunteer work (includes travel prompted by participation in a religious organization). If the purpose is primarily to provide health care, then the reason for travel should instead be providing medical care.
- Retirement: Travel for the purpose of retiring to a new location. Certain of these persons will be expatriates or long-term visitors.
- Planned medical care : Main purpose of travel is to obtain medical care
- Not ascertainable: Reason for travel cannot be ascertained or is unknown
Abbreviation: VFR = visiting friends and relatives.
BOX 3 . Changes to the GeoSentinel data entry application — GeoSentinel Network, 2012–2021
- Added date of illness onset
- Added preexisting conditions (e.g., HIV, cancer, or diabetes), including use of immunosuppressive drugs
- Added a requirement to mark a “primary diagnosis” if more than one diagnosis was entered
- Added new fields for diagnosis activity (active or resolved) and if diagnosed by screening
October 2015
- Modified function for “complete” records to include only those with infectious diagnoses or those that were travel related
- Added fields to capture the highest level of care required for the illness (severity), where the patient obtained pretravel information, and a write-in field for general comments
- Modified main presenting symptoms
- Updated reason for travel options
- ° Animal exposure
- ° Antibiotic taken during travel
- ° Attended mass gathering
- ° Blood or body fluid exposure
- ° Provided medical care
- ° Staying or eating in local homes
- ° Unplanned medical or dental care
- Added ability to capture diagnosis method(s)
- Created supplemental data form to collect antibiotic resistance data on nine pathogens ( Campylobacter spp., Escherichia coli , Klebsiella pneumoniae , Salmonella spp., S. enterica Typhi, S. enterica Paratyphi, Shigella spp., Staphylococcus aureus , and Streptococcus pneumoniae )
- Initiated special projects for mass gatherings and rabies postexposure prophylaxis
October 2016
- Modified main presenting symptoms and diagnostic methods
- Added ability to collect specimen type and organism genus and species
- Added geographic alerts for certain diseases (Barmah Forest virus, chronic Chagas disease, coccidioidomycosis, filariasis, malaria, paracoccidioidomycosis, Ross River virus, and schistosomiasis) that are reported from unexpected countries and regions
- Added required additional information for certain diseases, including vaccination status, etiology (e.g., organism genus and species), and cause of death
- Deployed enhanced surveillance migrant form to capture detailed information on migrants
November 2017
- Added subcategories for VFRs, identifying the VFR as the person, child or dependent, or spouse or partner
- Added option for secondary reason for travel and country of exposure for VFRs
- Added additional questions for certain diagnoses (i.e., malaria, leishmaniasis, and Zika)
- Added QA alerts to ensure that certain diagnoses meeting the case definition using the diagnosis methods to be marked confirmed
- Began collecting data for enhanced surveillance projects for rickettsioses, planned and unplanned healthcare abroad
August 2018
- Updated production database from Microsoft SQL Server 2008 to Microsoft SQL Server 2016
November 2018
- Combined supplemental migrant data collection form with main data collection form
- Updated expatriate and long-term visitor definitions and added subcategory options
- Added reason for travel, country of exposure, and region of exposure fields to each diagnosis
- Added imported infection as a travel-related option for migrants
- Added new project for respiratory illness in older travelers
October 2019
- Removed variables for primary diagnosis and patient type fields (inpatient, outpatient, tele-consult inpatient, and tele-consult outpatient)
- Removed student subchoices for travel reason field
- Added field for required medical evacuation
- Updated antibiotic resistance drug options
- Revised antibody diagnosis method to specify whether IgM or IgG
- Deployed enhanced surveillance project for respiratory illness in travelers related to COVID-19
August 2020
- Deployed enhanced surveillance project for sentinel identification of respiratory illness in travelers related to COVID-19
November 2021
- Updated COVID-19 vaccination status, including boosters
Abbreviations: IgG = immunoglobulin G; IgM = immunoglobulin M; QA = quality assurance; VFR = visiting friends and relatives.
FIGURE 2 . U.S. GeoSentinel sites* — GeoSentinel Network, 2012–2021
* Sites include Atlanta, GA (1); Baltimore, MD (2); Bethesda, MD (3); Birmingham, AL (4); Boston, MA (5); Bronx, NY (6); Bronx Lebanon, NY (7); Cambridge, MA (8); Hollywood, CA (9); Honolulu, HI (10); Miami, FL (11); New York City, NY (12); New York Northwest, NY (13); New York West, NY (14); Orlando, FL (15); Palo Alto, CA (16); Peekskill, NY (17); Salt Lake City, UT (18); Seattle, WA (19); and St. Paul, MN (20).
FIGURE 3 . U.S. nonmigrant travelers or migrants presenting to U.S. GeoSentinel sites — GeoSentinel Network, 2012–2021*
* A total of 149 non-U.S. residents were excluded from the analysis.
* Information available for 7,527 migrants and 9,852 other travelers. † Information available for 7,490 migrants and 9,793 other travelers. § Information available for 7,488 migrants and 9,841 other travelers. ¶ Information available for 4,672 migrants and 8,967 other travelers.
Abbreviations: CNS = central nervous system; ENT = ear, nose, and throat; STD = sexually transmitted disease. * The five most common diagnoses are provided for the most common travel-related syndrome and system groupings. † No deaths were observed among migrants; four deaths were observed among nonmigrant travelers.
* Information available for 2,892 diagnoses. † Five countries or regions with highest number of patient exposures. § Information available for 2,554 diagnoses. ¶ Information available for 1,575 diagnoses.
* Information available for 6,518 diagnoses. † Information available for 6,296 diagnoses. § Five countries or regions with highest number of patient exposures. ¶ Information available for 5,920 diagnoses. ** Information available for 1,894 diagnoses.
Suggested citation for this article: Brown AB, Miller C, Hamer DH, et al. Travel-Related Diagnoses Among U.S. Nonmigrant Travelers or Migrants Presenting to U.S. GeoSentinel Sites — GeoSentinel Network, 2012–2021. MMWR Surveill Summ 2023;72(No. SS-7):1–22. DOI: http://dx.doi.org/10.15585/mmwr.ss7207a1 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Motion Sickness: Symptoms, Who's at Risk, and How to Prevent It
- Who Is at Risk
- Medications
- Health Conditions
- When to Get Help
Motion sickness ( kinetosis ) causes symptoms that include dizziness, nausea , and headache . It occurs when you're moving (in a car, for example) and your brain receives mixed signals from your body, inner ear, and eyes about its surroundings. For instance, if you're below deck on a boat, your inner ear may sense rolling waves but your eyes don't see them. It is also called vertigo or seasickness , and is common in both children and adults, though some risk factors make it more likely.
Motion sickness also can occur due to flight simulators, gaming, amusement park rides, and other "virtual reality" experiences. Self-driving (automated) vehicles also lead to episodes of motion sickness, as people read or work on other tasks rather than driving themselves.
This article explains the symptoms of motion sickness, their causes, and who's at risk. It presents tips on managing your symptoms and ways to prevent motion sickness before it happens.
Illustration by Maritsa Patrinos for Verywell Health
Who Is at Higher Risk for Motion Sickness?
Studies have shown that essentially everyone has the potential to get motion sickness because it's related to the vestibular system (and its ear-related role in motion, balance, and coordination). It's common, with one study finding up to 25% of large ship passengers (even more on smaller boats) will develop motion sickness within two to three days of the start of an ocean voyage.
For some people, it starts right away, while others only feel sick after they’ve been moving for a long time. Some people are more likely to get motion sickness, including:
- Children aged 2 to 12 years (it can occur in younger children)
- Younger adults (compared with those over age 60)
- People who are pregnant
- People who get migraine headaches
Other factors that contribute to risk include:
- Alcohol and drug use
- Being sleep deprived
- Poor airflow in a vehicle
- Certain odors, including diesel fuel or cigarette smoke
A small study has shown that people who don't know when or how motion will occur may have more difficulty. Facing forward and watching the horizon may help deal with unpredictable motion and motion sickness.
Hormones and Motion Sickness
Females are more likely than males to get motion sickness, partly because of hormones. Estrogen , the primary female sex hormone, can contribute to symptoms of nausea and dizziness. Studies have shown that the menstrual cycle, as well as estrogen drugs or supplements, can affect how someone experiences motion sickness.
Symptoms of Motion Sickness
Symptoms of motion sickness can vary significantly from person to person, and the degree to which you feel ill can be less severe or more severe than other people who suffer from vertigo.
Nausea and vomiting are common, but they are not the only symptoms of motion sickness. Other symptoms may include:
- Cold sweats and clammy hands
- Hyperventilation (rapid breathing)
- Sensitivity to smells
- Loss of appetite (clinically called anorexia )
- Excessive salivation
- Warm, flushed sensation
Sopite Syndrome
Some people have a subcategory of motion sickness called sopite syndrome. The main symptoms of sopite syndrome include:
- Drowsiness and lethargy
- Mild depression
- Reduced ability to focus on an assigned task
Nausea and vomiting are not symptoms of sopite syndrome, which is one way it’s different from more common types of motion sickness. Sopite symptoms also may occur alone, or they may last longer than other motion sickness symptoms. The precise cause remains unclear, but it's possible another mechanism (including ear-related) is at work.
Medications Can Cause Motion Sickness
Motion sickness symptoms (or their increased severity) can be caused by certain medications. Both prescription drugs and over-the-counter (OTC) medications can cause side effects that result in motion sickness symptoms even when you’re not actually moving.
Nausea, dizziness, and feeling off balance are the vertigo-like side effects that can occur with a wide range of medications. Some of the common medications that may cause these symptoms include:
- Antibiotics such as penicillin, Suprax (cefixime), and Cipro (ciprofloxacin)
- Estrogen-containing medications such as birth control pills and hormone replacement therapy
- Bisphosphonates , such as Binosto (alendronate)
- Lanoxin ( digoxin )
- Inbrija (levodopa)
- Narcotic pain medications like Kadian (morphine), OxyContin ( oxycodone ), or Hysingla ER (hydrocodone)
- Non-steroidal anti-inflammatories like Advil (ibuprofen) and Aleve (naproxen)
- Selective serotonin reuptake inhibitors such as Paxil (paroxetine), Prozac (fluoxetine), and Zoloft (sertraline)
- Statins such as Crestor (rosuvastatin) and Zocor (simvastatin)
Even if you do feel discomfort, do not skip or stop taking your medications without talking to your provider.
If you will be traveling and are worried about motion sickness occurring or being more severe with a medication, talk to your healthcare provider. They may say that you can safely take your dose in a different way (for example, at a different time) to help prevent symptoms.
Motion Sickness Symptoms and Health Conditions
Motion sickness usually stops within eight hours of ending the activity or movement. If your symptoms do not get better when you stop moving, it could be another condition that causes the same symptoms as motion sickness and you should talk to your provider.
Conditions that can cause similar symptoms to motion sickness include:
- Fluid in the ear
- Benign paroxysmal positional vertigo (BPPV)
- Meniere’s disease
Talk to your healthcare provider about your symptoms to ensure an accurate diagnosis.
Treatment for Motion Sickness
There are a few treatment options for motion sickness. If you're taking medication before traveling, your healthcare provider may suggest a small dose before your trip to see how well it works.
Common medications for treating motion sickness include:
- Bonine (meclizine)
- Dramamine (dimenhydrinate)
- Phenergan ( promethazine )
Other options include:
- Anticholinergic drugs , including scopolamine (like the Transderm Scop patch)
- Benzodiazepines like Valium (diazepam)
- Dopamine receptor antagonists like Reglan (metoclopramide)
Acupuncture and other complementary medicine options, such as using the P6 pressure point to control nausea , exist for treating motion sickness. Some experts recommend ginger. However, there is limited research support for their benefits, and motion sickness remains easier to prevent than treat.
Preventing Motion Sickness
Changing your activities or position can help with motion sickness, though reading often leads to motion sickness. Lying down can help, as does limiting your visual input (for example, trees that seem to move as you pass them).
You can also try:
- Sitting in the front seat, if in a vehicle
- Turning air vents toward your face
- Keeping your head still
- Avoiding heavy meals or alcohol use
Natural remedies may help with motion sickness symptoms and their prevention. Try deep breathing exercises, which have been shown to help with seasickness in simulated exercises.
Physical therapy to help you adapt to motion may help, as can transcutaneous electrical nerve stimulation ( TENS ) using a small device that generates impulses. Cognitive behavioral therapy also may help to treat anxiety related to motion sickness.
Try Not to Think About Motion Sickness
Research has suggested that people who think they will get motion sickness are more likely to. You might be able to avoid or at least prevent motion sickness from getting worse by changing your thoughts and finding a distraction.
When to See a Healthcare Provider
Most people see a healthcare provider for motion sickness ahead of planned travel, in order to seek preventive treatment, but other situations do arise. The most common complications of motion sickness include vomiting that leads to dehydration and electrolyte imbalances , which can be treated easily. These conditions can, however, cause serious illness in some people.
Other conditions with symptoms similar to motion sickness include:
- Low blood sugar ( hypoglycemia ), which requires immediate care in people diagnosed with diabetes
- Stroke , a life-threatening condition that requires immediate intervention
- Traumatic head injury and concussion, commonly caused by sports injuries or accidents
If you feel sick after you hit your head or were in an accident, go to the emergency room or call 911.
Keep in mind that motion sickness usually goes away fairly quickly once you’ve stopped moving. If it’s been more than eight hours and you’re still having symptoms, call your provider.
While nausea and vomiting are common, they are not the only symptoms of motion sickness. Some people have other symptoms like fatigue and mood changes. Medications, hormones, and certain activities can make you more likely to get motion sickness.
It's easier to prevent motion sickness than treat it, so talk to your healthcare provider about medication and other treatment options.
If feelings of illness do not go away after the motion stops, your symptoms could be due to another condition. See your healthcare provider if you have motion sickness symptoms that last longer than eight hours.
Icahn School of Medicine at Mount Sinai. Motion Sickness .
Golding JF. Motion sickness . Handb Clin Neurol. 2016;137:371-390. doi:10.1016/B978-0-444-63437-5.00027-3
Li D, Chen L. Mitigating motion sickness in automated vehicles with vibration cue system . Ergonomics . 2022 Oct;65(10):1313-1325. doi:10.1080/00140139.2022.2028902.
Foster M, Singh N, Kwok K, Macefield VG. Vestibular modulation of skin sympathetic nerve activity in sopite syndrome induced by low-frequency sinusoidal motion. J Neurophysiol . 2020 Dec 1;124(6):1551-1559. doi: 10.1152/jn.00177.2020.
Leung AK, Hon KL. Motion sickness: an overview . Drugs Context . 2019 Dec 13;8:2019-9-4. doi: 10.7573/dic.2019-9-4.
Lipson S, Wang A, Corcoran M, Zhou G, Brodsky JR. Severe motion sickness in infants and children . Eur J Paediatr Neurol . 2020 Sep;28:176-179. doi:10.1016/j.ejpn.2020.06.010.
Laitinen L, Nurmi M, Ellilä P, Rautava P, Koivisto M, Polo-Kantola P. Nausea and vomiting of pregnancy: associations with personal history of nausea and affected relatives . Arch Gynecol Obstet . 2020 Oct;302(4):947-955. doi: 10.1007/s00404-020-05683-3.
Jones MLH, Le VC, Ebert SM, Sienko KH, Reed MP, Sayer JR. Motion sickness in passenger vehicles during test track operations . Ergonomics . 2019 Oct;62(10):1357-1371. doi: 10.1080/00140139.2019.1632938.
Peddareddygari LR, Kramer PD, Hanna PA, Levenstien MA, Grewal RP. Genetic Analysis of a Large Family with Migraine, Vertigo, and Motion Sickness . Can J Neurol Sci . 2019 Sep;46(5):512-517. doi: 10.1017/cjn.2019.64.
Kuiper OX, Bos JE, Schmidt EA, Diels C, Wolter S. Knowing What's Coming: Unpredictable Motion Causes More Motion Sickness . Hum Factors . 2020 Dec;62(8):1339-1348. doi: 10.1177/0018720819876139.
Smith PF, Agrawal Y, Darlington CL. Sexual dimorphism in vestibular function and dysfunction . J Neurophysiol . 2019;121(6):2379-2391. doi:10.1152/jn.00074.2019
Centers for Disease Control and Prevention. Motion Sickness .
Varis N, Leinonen A, Perälä J, Leino TK, Husa L, Sovelius R. Delayed Drowsiness After Normobaric Hypoxia Training in an F/A-18 Hornet Simulator . Aerosp Med Hum Perform . 2023 Sep 1;94(9):715-718. doi:10.3357/AMHP.6238.2023.
Altissimi G, Colizza A, Cianfrone G, et al. Drugs inducing hearing loss, tinnitus, dizziness and vertigo: an updated guide . Eur Rev Med Pharmacol Sci . 2020;24(15):7946-7952. doi:10.26355/eurrev_202008_22477
Seattle Children's Hospital. Motion sickness .
Hromatka BS, Tung JY, Kiefer AK, Do CB, Hinds DA, Eriksson N. Genetic variants associated with motion sickness point to roles for inner ear development, neurological processes and glucose homeostasis . Hum Mol Genet . 2015;24(9):2700-2708. doi:10.1093/hmg/ddv028
Golding JF, Patel M. Meniere's, migraine, and motion sickness . Acta Otolaryngol. 2017;137(5):495-502. doi:10.1080/00016489.2016.1255775
Koch A, Cascorbi I, Westhofen M, Dafotakis M, Klapa S, Kuhtz-Buschbeck JP. The neurophysiology and treatment of motion sickness . Dtsch Arztebl Int . 2018;115(41):687-696. doi:10.3238/arztebl.2018.0687
Stromberg SE, Russell ME, Carlson CR. Diaphragmatic breathing and its effectiveness for the management of motion sickness . Aerosp Med Hum Perform. 2015;86(5):452-7.
Huppert D, Benson J, Brandt T. A historical view of motion sickness - a plague at sea and on land, also with military impact . Front Neurol . 2017;8:114. doi:10.3389/fneur.2017.00114
Shen Y, Qi X. Update on diagnosis and differential diagnosis of vestibular migraine . Neurol Sci . 2022;43(3):1659-1666. doi:10.1007/s10072-022-05872-9
By Kristin Hayes, RN Kristin Hayes, RN, is a registered nurse specializing in ear, nose, and throat disorders for both adults and children.
Motion sickness
Motion sickness is feeling dizzy, or feeling or being sick when travelling by car, boat, plane or train. You can do things to prevent it or relieve the symptoms.
Check if you have motion sickness
Symptoms of motion sickness may include:
- feeling sick (nausea)
- feeling cold and going pale
How to ease motion sickness yourself
Do reduce motion – sit in the front of a car or in the middle of a boat look straight ahead at a fixed point, such as the horizon breathe fresh air if possible – for example, by opening a car window close your eyes and breathe slowly while focusing on your breathing distract children by talking, listening to music or singing songs break up long journeys to get some fresh air, drink water or take a walk try ginger, which you can take as a tablet, biscuit or tea don’t.
do not read, watch films or use electronic devices
do not look at moving objects, such as passing cars or rolling waves
do not eat heavy meals, spicy foods or drink alcohol shortly before or during travel
do not go on fairground rides if they make you feel unwell

A pharmacist can help with motion sickness
You can buy remedies from pharmacies to help prevent motion sickness, including:
- tablets – dissolvable tablets are available for children
- patches – can be used by adults and children over 10
- acupressure bands – these do not work for everyone
A pharmacist will be able to recommend the best treatment for you or your child.
Causes of motion sickness
Motion sickness is caused by repeated movements when travelling, like going over bumps in a car or moving up and down in a boat, plane or train.
The inner ear sends different signals to your brain from those your eyes are seeing. These confusing messages cause you to feel unwell.
Page last reviewed: 19 June 2023 Next review due: 19 June 2026

- New? Start Here
- Try For Free
10 Common Travel Diseases & How To Prevent Them

2020 has changed the way we travel.
It’s taught us that staying healthy and keeping each other safe while at home and while traveling are the most important things.
COVID-19 has enforced masks, social distancing, and stocking up on hand sanitizer and hand soap, along with several other germ-free items .
By following strict guidelines from the CDC and the WHO, we will begin to see a safe, healthy, happy world once again and we can’t wait to explore it!
But for now, let’s stay educated on COVID-19 with the help of WHO , as well as other risks and diseases we face when we travel.
Here are 10 common travel diseases and how to prevent them.
West Nile Virus

The West Nile Virus is a virus that is most commonly caused by the bite of a mosquito that has been infected by a bird.
According to the CDC , 8 out of 10 people infected do not show symptoms, about 1 in 150 people develop a severe case. The severe case symptoms can include encephalitis (inflammation of the brain) or meningitis (inflammation of the membranes that surround the brain and spinal cord), and high fever, headache, neck stiffness, stupor, disorientation, coma, tremors, convulsions, muscle weakness, vision loss, numbness, and paralysis.
The West Nile Virus is common in temperate and tropical regions like East Africa, Latin America and the Caribbean.
To protect yourself from mosquito bites, use Environmental Protection Agency (EPA)-registered insect repellents , wear long-sleeved shirts and pants, stay in places with screens on the windows and doors, and use a bed net .
Typhoid Fever

Typhoid Fever is caused by Salmonella Typhi bacteria. According to the CDC, typhoid fever occurs in countries with poor sanitation.
The person who is infected can spread this bacteria to others when they do not wash their hands and touch things that others touch. The water used to rinse and prepare food and drink can also become contaminated and infect others. People with typhoid fever usually have a high fever of 103–104°F (39–40°C).
Other symptoms include weakness, stomach pain, a rash, headache, diarrhea or constipation, cough, and loss of appetite. Paratyphoid fever is a similar disease also caused by bacteria.
The best ways to prevent getting typhoid fever include getting vaccinated, choosing food and drinks carefully when you travel, and washing your hands ! (sounds familiar, eh?).

Cholera is a diarrheal illness caused by infection of the intestine. According to the CDC, the cholera bacterium is usually found in water or food sources that have been contaminated by feces from a person infected with cholera.
Cholera is most likely to be spread in places with poor water treatment, poor sanitation, and poor hygiene. This disease is usually mild with no symptoms but can cause profuse watery diarrhea, vomiting, and leg cramps.
The five basic cholera prevention steps include drinking and using safe water, washing your hands often, using latrines or burying your poop, cooking food well (can be found in few fish), and cleaning up safely.

Malaria is caused by a mosquito bite and is found most commonly in Africa, Central, and South America, the Caribbean, Asia, Eastern Europe, and the South Pacific.
Malaria is categorized as either uncomplicated or complicated (severe). Malaria is curable if it is treated and diagnosed properly. Uncomplicated malaria generally presents itself as a cold stage (cold, shivering), a hot stage (fever, headaches, vomiting) and a sweating stage (sweats, returns to normal temperature, tiredness).
More commonly, these symptoms are reported: fever, chills, sweats, headaches, nausea and vomiting, body aches, and general malaise.
Severe malaria occurs when infections are complicated by serious organ failures or abnormalities in the patient’s blood or metabolism. Those symptoms can include cerebral malaria, severe anemia, hemoglobinuria, acute respiratory distress syndrome (ARDS), an inflammatory reaction in the lungs that inhibits oxygen exchange, abnormalities in blood coagulation, low blood pressure, acute kidney injury, hyperparasitemia, metabolic acidosis, and hypoglycemia.
Check out the CDC site for diagnosis and treatment of malaria.

Norovirus is a contagious virus that causes vomiting and diarrhea in all ages. You can catch this virus from direct contact with an infected person, consuming contaminated food or water and by touching contaminated surfaces and then putting your unwashed hands in your mouth!
The most common symptoms include diarrhea, vomiting, nausea, stomach pain, and is commonly called the ‘stomach bug’ or the ‘stomach flu.’ However, it is not related to the flu.
According to the CDC, it is the leading cause of illness and outbreaks from contaminated food in the United States.
In order to prevent the norovirus, you need to follow a few preventative measures including washing your hands, handling food properly and safely, cleaning and disinfecting surfaces, and washing laundry thoroughly.

Dengue is another common travel disease spread through mosquito bites. It is common in tropical and subtropical regions, including the Caribbean, Central and South America, Western Pacific Islands, Australia, Southeast Asia, and Africa.
Symptoms include fever, headache, nausea, vomiting, rash, pain in the eyes, joints, and muscles, and minor bleeding. They may take up to two weeks develop, but usually only last about a week, according to the CDC.
To prevent being bitten by a mosquito, use proper insect repellent, wear long sleeved shirts and pants, use permethrin-treated clothing and gear , sleep in air conditioned rooms, and use bed nets.

Tetanus is an infection caused by a bacteria called Clostridium tetani . This common travel disease causes painful muscle contractions and is commonly known as “lockjaw” because it causes a person’s neck and jaw muscles to lock, making it hard to open the mouth or swallow.
What’s different about this common travel disease is that it does not transfer from person to person, the bacteria are usually found in soil, dust, and manure and enter the body through breaks in the skin — cuts or wounds caused by contaminated objects.
It’s common in countries that don’t have access to immunization and very rare in the United States.
Tuberculosis

Tuberculosis is common in Asia, Sub-Saharan Africa and South and Central America. Symptoms of tuberculosis depend on where in the body the TB bacteria are growing – most commonly in the lungs.
TB in the lungs includes a bad cough that lasts 3 weeks or longer, pain in the chest, and coughing up blood or phlegm. Other symptoms can include weakness or fatigue, weight loss, no appetite, chills, fever, and night sweats.
You can get TB by being exposed to someone who already has it, however, it is not spread by shaking someone’s hand, sharing food or drink, touching bed linens or toilet seats, sharing toothbrushes, or kissing. It is spread through the air – so when someone who is infected coughs, speaks or sings.
Getting TB during air travel is very low risk. If you are in contact with someone who has TB, ask about administrative and environmental procedures for preventing exposure to TB. Additional measures include using personal respiratory protective devices.
Pertussis (Whooping Cough)
Pertussis , also known as Whooping Cough, is a disease that spreads to others when those infected with the bacteria cough, sneeze, or share the same breathing space. Early symptoms can include runny nose, low fever, and mild cough.
Later symptoms of the disease may include “fits” of many rapid coughs followed by a high-pitched “whoop,” vomiting, and exhaustion. The coughing fits can last for 10 weeks or more. While the disease is found worldwide, more whooping cough is seen in developing countries where very few people get vaccinated.
Babies can get whooping cough if their relatives have the disease, and it can cause serious and sometimes deadly complications for them.
The best way to prevent whooping cough is to stay up-to-date with whooping cough vaccines.
Yellow Fever

Yellow Fever is a disease caused by a virus that is spread through, you guessed it, mosquito bites!
Symptoms generally include fever, chills, headache, backache, and muscle aches. Severe cases result in bleeding, shock, organ failure, and sometimes death – but this is rare.
You are at risk for Yellow Fever when visiting parts of South America and Africa, getting a vaccine is highly encouraged. The vaccine is recommended at least 10 days before your trip.
In addition, to prevent mosquito bites, cover exposed skin with long sleeves, pants, use the appropriate insect repellent, reapply the repellent as directed, use permethrin-treated clothing and gear, sleep in air-conditioned rooms, and use a bed net when needed.
Now that you’ve seen our list of common travel diseases, what do you think? Did anything surprise you? Leave us a comment below!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Related Posts:

Advertiser Disclosure
This site is part of an affiliate sales network and receives compensation for sending traffic to partner sites, such as CreditCards.com. This compensation may impact how and where links appear on this site. This site does not include all financial companies or all available financial offers. We appreciate your support!
Editorial Note: Opinions expressed here are the author’s alone, not those of any bank, credit card issuer, airlines or hotel chain, and have not been reviewed, approved or otherwise endorsed by any of these entities.
Travel Tips, Tricks, & Hacks — Straight To Your Inbox
No spam, only the goods. And we would never share your info with anyone.
- Bucket List
- Travel Tips
- Remote Work
- Gift Guides
Most Popular Stories

11 Proven Ways To Be A Responsible Traveler
We want to be responsible adults, responsible citizens, but what about responsible travelers? Are there things we can do that protect us and those around
7 Literary Cities for the Book Lover
We read books to learn new skills, understand our world better, and get lost in the incredible stories of authors from all walks of life.

14 Tips for Anyone Traveling Alone
In these challenging times, our schedules are out of whack and we are itching to explore. You may find that significant others and close friends

13 Unique Gift Ideas For Father’s Day
Our fathers hold a special place in our hearts. Whether you’re able to spend this Father’s Day with yours or not, we hope to help
Travel More, Remember Better.
- Journo Travel Journal
- Currency Converter
- Become An Insider
- Digital Nomad Secrets
- Remote Work Wealth Club
- Travel Hacker's Toolkit
- Travel Fund Challenge
- Insider Adventures
- Shop Travel Goods
- TERMS & CONDITIONS
- PRIVACY POLICY
Sat 27 Apr 2024
2024 newspaper of the year
@ Contact us
Your newsletters
The science behind travel sickness, and how to avoid it
Gp offers advice on the best way to stay illness-free on long journeys.

For many families the summer holidays bring the opportunity to venture out on exciting road trips to far flung places.
But for some, long drives to holiday destinations or to visit family bring the unpleasant prospect of car sickness.
Ranging from a generally unwell feeling to nausea and vomiting, travel sickness can make holidays a misery for many but there are steps you can take to avoid it or at least reduce the symptoms.
What causes travel sickness?
According to GP and author, Dr Sarah Brewer, travel and motion sickness can be triggered by any form of transport and is caused when motion-detecting cells in the inner ears are excessively stimulated and send messages to the brain which don’t match the degree of movement detected by the eyes.
“Your eyes tell your brain that the environment is stationary but your balance organs say that it isn’t – this triggers travel sickness”, says Dr Brewer.

Read more: The 10 best traditional car games for the whole family
“Most people have experienced it at some point in their lives, however some people, particularly children, are especially sensitive as their nerve pathways involved are not fully developed. Before the age of ten, children are especially susceptible.”
According to research by Euro Car Parts, reading, watching a screen, travelling backwards and sitting in the back seat of a car are among the most common causes of feeling car sick. And small cars were the worst form of transport for instigating a bout of illness, to blame for 44 per cent of cases.

10 most common causes of travel sickness Reading (39%) Travelling backwards (38%) Sitting in the back seat (31%) Travelling while tired (17%) After drinking alcohol (16%) Watching a screen (15%) Dehydration (15%) Travelling while hungry (14.7%) Standing while travelling eg on public transport (11%) After eating (6%)
How to stop travel sickness
To help those who suffer from car sickness, Dr Brewer has come up with some tips to help avoid its onset or mimimise its effects
Watch what and when you eat and drink
When travelling, it can be tempting to buy quick and easy fast food from service stations en route. However, greasy, fatty and spicy food can cause nausea and trigger or worsen travel sickness. Likewise, alcohol can act as a diuretic and dehydrate you – further exacerbating your motion sickness.
You should however avoid travelling on an empty stomach – have a light meal instead 45 to 60 minutes before travelling, and top yourself up with light snacks which are bland and low in fat and acid.

Position is everything
If possible, offer to drive – drivers are less likely to suffer from travel sickness as they are concentrating on the outside. If driving isn’t an option, try to sit in the front seats and open the windows to get fresh air circulating.
Keep your attention focused on the distant horizon to reduce your sensory input. To help children, use car seats to ensure children can sit high enough to see out of the window.
To reduce nausea-inducing movement in other vehicles, try and sit between the wheels on buses or coaches where movement is less, or in the area above the wings on an aeroplane.
If all else fails, try medication
For travel sickness, prevention is easier than treating symptoms once they start. Try taking the antihistamine cinnarizine, which works on the vomiting centre in the brain, two hours before a journey, and it will reduce your susceptibility to motion sickness for at least eight hours.
If you are already feeling sick, however, you can suck a tablet rather than swallowing it for a more rapid effect. Just make sure you don’t take sedating travel sickness medication or drive if you feel drowsy.
If you prefer a more natural option, Dr Brewer recommends trying ginger tablets or wearing acupressure bands on your wrists.

Chris Barella, digital services director at Euro Car Parts said: “Unfortunately, motion sickness is something that most of us have dealt with at some point in our life and will probably have to continue to deal with.
“No one wants to experience that nauseous feeling while travelling. Hopefully the advice offered by Dr Brewer will help sufferers, particularly if you have no choice but to travel.”
Most Read By Subscribers

4 COMMON TRAVEL DISORDERS AND HOW TO MANAGE THEM
A practical guide to travel-related disorders.
While travel can be fun, it can expose you to obvious as well as hidden hazards, possibly causing illness or exacerbating existing health issues. Lack of sleep combined with stress, dehydration, increased exertion levels, musculoskeletal stresses and a change in medical-care delivery systems could have an impact on the traveler.
A few disorders, however, are actually caused by the process of getting from one place to another around the globe.
- Jet Lag
- Motion Sickness
- Deep Vein Thrombosis
- High Altitude Illness
The following sections of this guide provide a summary of the causes and symptoms of each condition as well as tips for prevention and instructions for treatment.
— Contributors — James M. Chimiak, MD Petar Denoble, MD
Download this guide
See more Travel Health and Safety guides >>
What is Jet Lag?
Long-distance travel in which humans cross several time zones in a short time can cause what is commonly known as jet lag, also called rapid time zone change syndrome or desynchronosis. This condition results from your circadian rhythm — your internal clock, which is attuned to the day-night cycle at your departure location — being out of sync with the day-night cycle at your destination with little or no time to adjust.
Jet lag primarily affects air travelers because of the greater distances and time zones covered in a relatively short time. Boaters may have some difficulty with this condition if they do not make regular accommodations as they travel across the globe.
Symptoms of Jet Lag
Feeling sleepy, hungry and alert at the wrong times are common symptoms of jet lag, which may affect your social life and your ability to work, exercise or sleep. Fortunately, your internal clock will synchronize with your new environment within a few days. The more times zones you cross, the more intense your symptoms are likely to be and the longer they will take to diminish.

Prevention and Treatment of Jet Lag
A few days to a week before your departure, try to gradually move your bedtime to what it will be at your destination — i.e., if you are traveling east, where night comes sooner than at your departure location, go to bed one hour earlier than you usually would for as many days as the number of time zones you will travel through. To make it easier to fall asleep early, avoid coffee, tea, chocolate, alcohol, and exercise for three to four hours before your new bedtime. Then wake up earlier in the morning and try to catch some sunshine to help your body's internal rhythm adjust. If you are traveling west, you should do the reverse routine — gradually go to bed and wake up later in the days leading up to your departure.
Jet lag may be exacerbated by poor sleep during an overnight flight. Falling asleep on a plane can be difficult for several reasons. During sleep, your body temperature falls, and the activity of some hormones changes. This process usually occurs at a similar time every day, prompted by changes in surrounding light and noise. With the onset of darkness, the pineal gland in the brain starts to secrete melatonin, known as the "hormone of darkness." Melatonin helps the body fall asleep and stay asleep, but it is not strong enough to do so on its own.

To sleep well during a flight, it is important to avoid excessive consumption of caffeine and alcohol. Caffeine may prevent you from falling asleep, and alcohol will prevent you from staying asleep and experiencing normal restorative stages of sleep. The use of earplugs and an eye mask to reduce noise and mimic darkness may also help.

Upon arrival at your destination, stay active during daylight hours, and go to bed in the evening at your usual time. You might also consider taking melatonin before your bedtime for the first few days at your destination. In the morning, going out in the sunlight will help your circadian rhythm adjust. If weather prohibits exposure to sunshine or if you are traveling from a summer climate to a winter one, try to start your morning with exercise at a gym or swimming pool.
If these measures are not sufficient, try taking between 0.3 mg and 1.0 mg of melatonin 30 minutes before your bedtime.
About Melatonin
Classified as a food supplement, melatonin is available without a prescription and is not regulated by the U.S. Food and Drug Administration (FDA). The amount of active hormone in one dose may vary slightly from what is declared on the box, and response to melatonin varies individually. Excessive melatonin may interfere with your sleep. Avoid taking more than 3.0 mg at once, as too much melatonin can cause headaches, nausea, dizziness or irritability.
Considered nonaddictive and safe for short-term use, melatonin can interact with certain medications, however, including anticoagulants, immune suppressants, diabetes medications, and birth-control pills. If you have any health conditions, check with your doctor before using melatonin.
Refrain from activities that require alertness — such as driving, boating or diving — for four to five hours after taking melatonin.
Tips For Boaters About Jet Lag
Observe members of a boat crew for evidence of drowsiness and jet lag, as its effects will be cumulative if not addressed. Just one crew member's impairment can result in increased burdens and fatigue on a small crew. If the conditions are left undetected, an impaired watchstander can have catastrophic consequences for the boat.
For advice on getting enough sleep while onboard, read Importance of Sleep While Boating (and How to Do It Safely) .
MOTION SICKNESS
What is motion sickness.
Kinetosis — commonly known as motion sickness — is any disorder caused by motion, such as seasickness, airsickness or carsickness, as defined by Taber's Cyclopedic Medical Dictionary. It is a common complaint of travelers on boats or planes, in motor vehicles, and even while riding animals such as horses.
Most people, including experienced boaters and frequent air travelers, have experienced motion sickness at some time. All that is needed is a strong enough stimulus, which can vary widely from one person to another. Most people acclimate — or "get their sea legs" — with time, but the process can take up to two or three days.

Symptoms of Motion Sickness
The most distressing symptoms of motion sickness are nausea and vomiting, generally caused by an overstimulation of your inner ear's vestibular balance organs and/or by a discrepancy between the sensory inputs from your eyes and inner ears. Other symptoms include excessive sweating, pallor (pale skin), a mild headache and malaise.
Motion sickness is not a serious medical problem, but it may lead to more significant health issues or incidents because affected individuals can develop an almost desperate inattentiveness and a reduced ability to perform simple tasks. Assume that any tasks assigned to those affected by motion sickness require supervision. Reassign critical tasks to others who are less impaired.
Prevention and Treatment of Motion Sickness
It is best to plan ahead to reduce the risk of motion sickness . Prepare by being well-rested, nourished and adequately hydrated. If you feel anxious or uneasy, avoid consuming food for two hours before you embark for a short sail, as you will likely be more comfortable with an empty stomach than with a full one. For boaters, stow and prepare your gear before the boat leaves the dock to limit the time spent below decks.
While underway, position yourself on the boat where the motion is least, such as midline on the boat, low and close to the waterline or on the stern (if minimal or no exhaust is present). Avoid areas where the vertical motion is more pronounced, such as the bow or upper decks. Closing your eyes or sitting where the rocking motion of a boat is clearly visible can help prevent motion sickness. Gazing at the horizon rather than at objects in your immediate vicinity is widely accepted as helpful. Staying away from areas with strong fumes, particularly fuel or exhaust, is also a good idea. Avoid reading, looking at electronic devices or moving your head continuously back and forth because this can worsen symptoms.

Advertisements promote numerous medications, herbs, foods and devices to prevent or treat motion sickness. Although many of these aids have proved to be successful, none are known to be completely effective. Taking an over-the-counter antihistamine such as meclizine, dimenhydrinate or cyclizine before you feel sick can be helpful, but it may cause some degree of drowsiness. Antihistamines interact with many drugs, so if you have chronic health issues and are taking other medications, consult your physician before you travel so there is enough time to make any necessary adjustments. As always, it is wise to test new medications or supplements days to weeks before using them away from home. Motion-sickness medications typically are most effective when taken before symptoms begin and are less effective after symptom onset.

If necessary, motion sickness can be treated with either oral drugs or a transdermal patch, which delivers medication through the skin. On the rare occasion when nausea and vomiting are severe and not improving after several days and other problems begin to appear, the person may need to be returned to shore for medical attention.
Drugs used to prevent and treat motion sickness vary in their effectiveness and side effects from one individual to another, so it is not possible to make a generalized recommendation. Use such medications with caution during certain activities, as most of these drugs cause mild drowsiness and inhibit mucous secretions.
Motion sickness usually subsides as the body adapts or when the motion stops. Fortunately, the more frequently one travels, the easier it becomes to adjust to being in motion.
About Prescription Scopolamine
For many people, transdermal delivery of the prescription drug scopolamine can be effective. The patch, which goes by the brand name Transderm Scop®, contains 1.5 mg of scopolamine. When placed on the skin (typically just behind the ear), the patch delivers the drug at a constant rate for three days. Remove the patch after that period. Those who are still in an environment where motion sickness could be a problem can apply another patch. Wear only one patch at a time, even if you think one patch is depleted, to avoid too much medication entering the bloodstream and causing undesirable side effects.
Possible side effects of scopolamine include dry mouth, drowsiness, and blurred vision. Disorientation, memory disturbances, dizziness, and restlessness may occur but are less common. Scopolamine should be used with caution in patients with narrow-angle glaucoma, a pyloric obstruction or a urinary bladder neck obstruction (such as from an enlarged prostate). Rare side effects include hallucinations, confusion, difficulty urinating, skin rashes, and eye pain.
It is impossible to know in advance who scopolamine will affect and how. Therefore, before using a patch to prevent motion sickness, it is recommended to wear one on dry land for at least 24 hours to test its effects. Once you open the foil wrapper, avoid touching the patch under the plastic strip. If some of the medication gets on your finger and inadvertently contaminates your eye, the drug will produce unilateral pupil dilation, which has caused confusion with a number of serious medical emergencies by those who are unaware of this association. Do not consume alcohol while wearing a scopolamine patch.
If side effects occur, remove the patch. If you experience severe allergic reactions, difficulty urinating, pain in the eyes or dilated pupils, seek immediate medical attention.
If a patch is worn for more than three days, withdrawal symptoms can occur after removal. These symptoms, which generally do not occur until 24 hours after removal, include dizziness, nausea, vomiting, headache and balance disturbances.
Why Boaters Need a "Plan B" for Motion Sickness
Whether you are planning an ocean crossing, a leisurely sail to the islands for a few weeks, or a day or two of deep-sea fishing, under certain circumstances motion sickness can be a potential hazard to recreational boaters.
Consider, for example, getting seasick while traveling offshore with your small children or your first bareboat charter vacation. In both cases, the severity of your symptoms could negatively affect your reaction times and your ability to concentrate. You may not be able to keep as close a watch on your kids' safety as you normally would. You may be too distracted to notice weather changes or objects lurking below the waterline. You may be unable to provide timely or appropriate assistance if someone falls overboard or gets injured. Many people with motion sickness will express that during the first few days of travel they experience apathy and a decreased attention to detail even if they never experience nausea or vomiting.
You cannot always anticipate the onset or severity of motion sickness, but with a bit of preparation, you can develop a plan to help manage the situation in case it occurs. Your "Plan B" could be as simple as ensuring that someone else on board has the ability to take over or help when needed. If you are new to boating or if you are planning an expensive trip, consider taking a short, inexpensive day trip prior to your excursion, especially if it is one in which your best efforts are required for the safety of the trip. That way you have time to consider other options if you are susceptible to motion sickness.
The possibility of disordered sleep, watchstanding, inexperienced or rusty sailors, medications, and seasickness should require everyone to be vigilant and double-check themselves and each other.
DEEP VEIN THROMBOSIS (DVT)
What is deep vein thrombosis.
Deep vein thrombosis (DVT) is an acute condition in which a blood clot (also known as a thrombus) forms in one or more of the body's deep veins, usually in the legs. These blood clots can then break free, travel through the bloodstream and cause life-threatening conditions such as a pulmonary embolism — a blood clot that lodges in the lungs. The blockage can be great enough to reduce the heart's ability to circulate blood to the lungs, impairing vital functions such as the elimination of carbon dioxide and the delivery of oxygen.

Symptoms of Deep Vein Thrombosis
- swelling of the affected leg, ankle, and foot
- pain in the calf that spreads to the ankle and foot
- warmth across the affected area
- change in skin color to pale, red or blue
These symptoms are not exclusive to DVT, and at least half of people with similar symptoms may have conditions other than DVT.
DVT often reoccurs and in many cases causes long-term complications such as postthrombotic syndrome (PTS) or pulmonary hypertension after a pulmonary embolism. PTS includes leg swelling, pain, skin discoloration and sometimes skin ulceration due to abnormal local circulation. It is caused by inflammation of veins and incomplete resolution of thrombi, which make veins less efficient at circulating blood out of the affected leg.
These complications can occur without a previous diagnosis of a DVT, which may be asymptomatic. Indeed, even when a DVT is suspected, its diagnosis is quite uncertain.
Travel is thought to increase the likelihood of a DVT. Most DVTs related to air travel occur within the first two weeks after a flight and resolve within eight weeks. In about 25 percent of cases, an untreated DVT of the calf can spread upward into the veins of the thigh and pelvis. If a DVT of the thigh or pelvis is left untreated, there is a risk of a blood clot that originated as a lower-extremity DVT moving centrally and lodging in a pulmonary vessel, resulting in pulmonary embolism. A massive pulmonary embolism is usually fatal.
About Pulmonary Embolism

- sudden shortness of breath
- chest pain or discomfort that worsens with a deep breath or cough
- lightheadedness, dizziness or fainting
- rapid pulse
- coughing up blood
- anxiety or nervousness
Pulmonary embolism is an emergency that requires immediate medical care. In remote locations, an emergency medical evacuation may be needed. In scuba diving situations, the diagnosis may be confused with dive-related injuries.
Another complication of a DVT is a condition called paradoxical embolism — in which a traveling blood clot passes directly into the arterial circulation instead of lodging in or being filtered through the pulmonary circulatory system.

Paradoxical embolism may occur in individuals who have a congenital condition such as patent foramen ovale (PFO) or atrial septal defect (ASD), in which a hole is in the wall separating the heart's right and left upper chambers — this enables venous blood to bypass the lung and pass directly to the arterial system. A clot that may have traveled from the calf to the heart through an atrial wall opening, for example, and into the arterial circulation is a paradoxical embolism. A paradoxical embolism that enters the brain may cause a stroke.
Prevention and Treatment of DVT

The risk of DVT in healthy, active people is small. Most cases of DVT occur in people with preexisting risk factors who are forced to sit still for a long time (such as travelers who take long plane, car, boat or train journeys), bedridden patients and office workers who sit at their desks for many hours. Immobility slows down the blood flow in the veins (a condition known as venous stasis), and pressure exerted on the calf by poorly designed seats can injure the vein walls. After sitting for 90 minutes, the blood flow in the calf drops by half, which doubles the chance of developing a clot. In individuals with preexisting risk factors, for every hour spent sitting, the risk of a blood clot increases by 10 percent.
The incidence of DVT in the general population is only 0.1 percent, but it is higher in high-risk subpopulations. Long-distance air travel — for which this condition is well studied — is thought to increase the risk of DVT two- to four-fold. The incidence for travelers on flights lasting more than four hours is between 1 per 4,650 flights and 1 per 6,000 flights. This risk is lower than for the general population because people who take long trips generally are healthier on average since very sick individuals tend to avoid long-distance travel.
After a trip of more than eight hours, the incidence of DVT among travelers with a low to intermediate preexisting risk for a DVT was found to be 0.3 percent for symptomatic cases and 0.5 percent when including asymptomatic cases. Again, remaining sedentary while traveling on a boat can share some of the same risks as those for air or motor vehicle travel.
DVT Risk Factors

- age (risk rises after age 40)
- obesity (risk rises in individuals with a body mass index (BMI) of more than 30 kg/m2)
- estrogen use (either with hormonal contraceptives or hormone replacement therapy)
- pregnancy or recent childbirth (within two to three months)
- thrombophilia (an abnormally increased tendency to develop clots)
- previous DVT or a family history of DVT
- active cancer
- serious medical illness
- recent surgery, hospitalization or trauma
- limited mobility
- central venous catheterization
Airline passengers who are shorter than 5 feet, 3 inches (1.6 meters) or taller than 6 feet, 3 inches (1.9 meters) are at an increased risk of DVT because plane seats cannot be adjusted to their height. In addition to immobility, shorter passengers may experience seat-edge pressure on the backs of their knees, and taller passengers may be cramped due to insufficient legroom, increasing the likelihood of vein-wall injury, venous stasis, and activation of the blood's natural clotting mechanisms.
People with a predisposition to blood clots should wear compression socks (knee high) or stockings (thigh-high) when traveling and should consult their physician regarding the use of an anticoagulant medication such as aspirin.

Compression footwear reduces the chance that your blood will pool and clot, and anticoagulants inhibit your blood's ability to clot. Regular use of compression socks or stockings can also help prevent the swelling associated with DVT. It is usually advisable to wear compression footwear for at least a year after experiencing a DVT.
Anticoagulants (blood thinners) are drugs that inhibit your blood's ability to clot, thus reducing your risk of developing a clot. They range from over-the-counter medications such as aspirin to much stronger drugs such as warfarin (brand name Coumadin®) as well as newer direct oral anticoagulants. There is no evidence, however, that healthy people without preexisting risks for DVT benefit from compression footwear or anticoagulants.
People who cannot take anticoagulants, who have a DVT recurrence despite taking anticoagulants or who have repeated pulmonary embolisms can have a filter inserted in their inferior vena cava — the vessel that returns venous blood from the lower body to the heart. This filter, which is sometimes referred to as an umbrella because of its appearance, prevents clots that break loose from lodging in the lungs. Individuals with vena cava filters may return to a normal day-to-day life.
Everyone should avoid long periods of immobility — it is good practice to periodically get up and walk around while traveling. Exercising or flexing your feet and calf muscles while you are seated and staying well hydrated can also be helpful.
DVT is a serious medical condition that can result in death or major disability due to pulmonary embolism or PTS. Thus, it is an emergency that requires appropriate diagnosis and treatment to improve the chances of healing and to prevent life- and limb-threatening complications. In the hospital environment, early thrombus clearance rapidly resolves symptoms, preserves veins and restores their normal function.
Tips for Boaters on DVT
Most boat crews will be actively moving about the boat, completing their tasks for a successful voyage and minimizing such stasis. Some crew members may be immobile for prolonged periods due to physical condition or status, but this practice should be discouraged to mitigate the risk of DVT.
This information is applicable to a companion who remains seated next to a boat captain, who is standing at the helm, while the companion may be relatively dehydrated, sedentary, sitting with feet dangling and with pressure on the back of the thighs — a setup for a DVT.
On a boat, getting up and "making rounds" not only may help prevent a DVT but also may help detect a problem with the boat early.
HIGH ALTITUDE ILLNESS
What is high altitude illness.
Traveling to high altitudes exposes people to increasingly rarefied air and progressively decreasing amounts of oxygen, resulting in declining levels of oxygen in the blood, which can lead to impaired physical and mental performance. Responses to high altitudes vary, but most people can function normally at heights up to 8,000 feet (2,438 meters) above sea level. At altitudes greater than that, the oxygen deficit can begin to cause a condition known as acute mountain sickness (AMS). At elevations higher than 10,000 feet (3,048 meters), 75 percent of people will experience at least mild AMS symptoms.

Symptoms of High Altitude Illness
The onset of AMS symptoms varies according to the altitude, the rate of ascent and the individual's susceptibility to the disease. A slow ascent may allow the body to acclimate by establishing a more rapid spontaneous breathing rate to make up for the decreased oxygen in the atmosphere. Symptoms usually start 12 to 24 hours after arrival at altitude and begin to decrease in severity around the third day at a given elevation.
AMS causes travelers to feel generally unwell. They may also experience a loss of appetite, headaches, lightheadedness, fatigue, breathlessness, rapid heartbeat, nausea or difficulty sleeping. Symptoms tend to be worse at night. Mild AMS does not interfere with normal activities, and symptoms generally subside within two to four days as the body acclimates.
Severe HAI manifests as serious conditions known as high-altitude pulmonary edema (HAPE) or high-altitude cerebral edema (HACE), caused by the accumulation of excess fluid in the lungs or brain. Symptoms of HAPE and HACE include a gray or pale complexion, a blue tinge to the skin (cyanosis), chest tightness or congestion, cough, coughing up blood, difficulty walking, shortness of breath when at rest, withdrawal from social interaction, confusion or decreased consciousness. These conditions can be fatal if not treated or if the victim is not returned to a lower altitude.
AMS Prevention and Treatment
- severe breathing problems
- altered level of alertness
If you cannot count on EMS aid, move the affected individual to a lower altitude as quickly and as safely as possible, and administer oxygen if it is available. Keep victims warm, and be sure they stay well hydrated if they are conscious.
To avoid high altitude illness, it is important to ascend slowly enough to allow time for your body to acclimate. Some people also find it beneficial to take prophylactic medication to help with the acclimatization process or to prevent some ill effects. If you plan to travel to a high-altitude location, visit your doctor or a travel clinic before your trip to evaluate your risk of HAI and to obtain prophylactic medication that may prevent or alleviate AMS.

Risk Factors for Acute Mountain Sickness
- You live at or near sea level and travel to a high altitude.
- You have had AMS before.
- You have preexisting medical conditions.
- You ascend quickly to a high elevation.
Consult your doctor before traveling to a high-altitude location if you have a heart, lung or blood disorder. You may need to travel with supplemental oxygen.

- Ascend slowly above 8,000 feet.
- If you travel to high altitudes, choose a slow transportation method or walk.
- If you get there by flying, do not overexert yourself or travel still higher for the first 24 hours.
- If you travel above 10,000 feet (3,048 meters), increase your altitude by no more than 1,000 feet (305 meters) per day.
- After every 3,000 feet (914 meters) of elevation gained, take a rest day.
- After daily excursions, return to a lower altitude for the night, if possible.
- Do not go higher if you experience any AMS symptoms; wait for the symptoms to decrease before ascending.
- If your symptoms worsen, go to a lower altitude.
- Stay properly hydrated. Drink at least three to four quarts of fluids per day, and be sure to quench your thirst. Make sure to urinate regularly.
- Engaging in light activity during the day is better than sleeping, because respiration decreases during sleep, exacerbating AMS symptoms.
- Avoid tobacco, alcohol and depressant drugs (such as barbiturates, tranquilizers, and sleeping pills), all of which worsen AMS symptoms.
- Eat a high-carbohydrate diet while at altitude, but do not overeat.
- Boating and diving are not recommended.
HAI can affect those engaging in mountain climbing, mountaineering, rock climbing and hiking at higher elevations. Often these locations make medical evacuation difficult and delayed. Moving the victim to lower elevations becomes a priority for those who are accompanying the victim.
LEARN MORE ABOUT TRAVEL-RELATED DISORDERS
- Jet Lag (Centers for Disease Control and Prevention, CDC)
- What is Circadian Rhythm? (National Sleep Foundation)
- Melatonin (Mayo Clinic)
- Motion Sickness (CDC)
- Deep Vein Thrombosis and Pulmonary Embolism (CDC)
- Travel to High Altitudes (CDC)
- Altitude Illness (CDC)

ABOUT DAN BOATER
Since its inception in 1980, DAN® has spent more than 300,000 medical resource hours on duty, fielding more than 100,000 emergency calls and coordinating more than 10,000 emergency evacuations worldwide, making it one of the world’s most trusted resources for traveler safety.
As a natural evolution of DAN’s successful 35+ years of service to the diving community, our new DAN Boater membership program is committed to helping recreational boaters in need of emergency assistance while traveling the globe, and to promoting smart travel health and safety practices through research and education.
- 24/7 Emergency hotline
- Medical information line
- Worldwide medical evacuation and repatriation services
- Search and rescue expense coverage
- Travel health and safety guides
- Global medical referrals, prescription assistance, and more
Learn how an affordable annual DAN Boater membership is helping thousands of travelers just like you every day.

NICHOLAS A. RATHJEN, DO, AND S. DAVID SHAHBODAGHI, MD, MPH
Am Fam Physician. 2023;108(4):396-403
Author disclosure: No relevant financial relationships.
Approximately 1.8 billion people will cross an international border by 2030, and 66% of travelers will develop a travel-related illness. Most travel-related illnesses are self-limiting and do not require significant intervention; others could cause significant morbidity or mortality. Physicians should begin with a thorough history and clinical examination to have the highest probability of making the correct diagnosis. Targeted questioning should focus on the type of trip taken, the travel itinerary, and a list of all geographic locations visited. Inquiries should also be made about pretravel preparations, such as chemoprophylactic medications, vaccinations, and any personal protective measures such as insect repellents or specialized clothing. Travelers visiting friends and relatives are at a higher risk of travel-related illnesses and more severe infections. The two most common vaccine-preventable illnesses in travelers are influenza and hepatitis A. Most travel-related illnesses become apparent soon after arriving at home because incubation periods are rarely longer than four to six weeks. The most common illnesses in travelers from resource-rich to resource-poor locations are travelers diarrhea and respiratory infections. Localizing symptoms such as fever with respiratory, gastrointestinal, or skin-related concerns may aid in identifying the underlying etiology.
Globally, it is estimated that 1.8 billion people will cross an international border by 2030. 1 Although Europe is the most common destination, tourism is increasing in developing regions of Asia, Africa, and Latin America. 2 Less than one-half of U.S. travelers seek pretravel medical advice. It is estimated that two-thirds of travelers will develop a travel-related illness; therefore, the ill returning traveler is not uncommon in primary care. 3 Although most of these illnesses are minor and relatively insignificant clinically, the potential exists for serious illness. The advent of modern and interconnected travel networks means that a rare illness or nonendemic infectious disease is never more than 24 hours away. 4 Travelers over the past 10 years have contributed to the increase of emerging infectious diseases such as chikungunya, Zika virus infection, COVID-19, mpox (monkeypox), and Ebola disease. 3
Although most travel-related illnesses are self-limiting and do not require medical evaluation, others could be life-threatening. 5 The challenge for the busy physician is successfully differentiating between the two. Physicians should begin with a thorough history and clinical examination to have the highest probability of making the correct diagnosis. Travelers at the highest risk are those visiting friends and relatives who stay in a country for more than 28 days or travel to Africa. Most travel-related illnesses become apparent soon after arriving home because incubation periods are rarely longer than four to six weeks. 3 , 6 The most common illnesses in travelers from resource-rich to resource-poor locations are travelers diarrhea and respiratory infections. 7 , 8 The incubation period of an illness relative to the onset of symptoms and the length of stay in the foreign destination can exclude infections in the differential diagnosis ( eTable A ) .
General questions should determine the patient’s pertinent medical history, focusing on any unique factors, such as immunocompromising illnesses or underlying risk factors for a travel-related medical concern. Targeted questioning should focus on the type of trip taken and the travel itinerary that includes accommodations, recreational activities, and a list of all geographic locations visited ( Table 1 3 , 6 , 9 and Table 2 3 , 6 ) . Patients should be asked about any medical treatments received in a foreign country. Modern travel itineraries often require multiple stopovers, and it is not uncommon for the casual traveler to visit several locations with different geographically linked illness patterns in a single trip abroad.
Travel History
Travelers visiting friends and relatives are at a higher risk of travel-related illnesses and more severe infections. 10 , 11 These travelers rarely seek pretravel consultation, are less likely to take chemoprophylaxis, and engage in more risky travel-related behaviors such as consuming food from local sources and traveling to more remote locations. 3 Overall, travelers visiting friends and relatives tend to have extended travel stays and are more likely to reside in non–climate-controlled dwellings.
During the clinical history, inquiries should be made about pretravel preparations, including chemoprophylactic medications, vaccinations, and personal protective measures such as insect repellents or specialized clothing. 12 , 13 Accurate knowledge of previous preventive strategies allows for appropriate risk stratification by physicians. Even when used thoroughly, these measures decrease the likelihood of certain illnesses but do not exclude them. 6 Adherence to dietary precautions and pretravel immunization against typhoid fever do not necessarily eliminate the risk of disease. Travelers often have no control over meals prepared in foreign food establishments, and the currently available typhoid vaccines are 60% to 80% effective. 14 Although all travel-related vaccines are important, the two most common vaccine-preventable illnesses in travelers are influenza and hepatitis A. 12 , 15
Travel duration is also an important but often overlooked component of the clinical history because the likelihood of illness increases directly with the length of stay abroad. The longer travelers stay in a non-native environment, the more likely they are to forego travel precautions and adherence to chemoprophylaxis. 3 The use of personal protective measures decreases gradually with the total amount of time in the host environment. 3 A thorough medical and sexual history should be obtained because data show that sexual contact during travel is common and often occurs without the use of barrier contraception. 16
Clinical Assessment
The severity of the illness helps determine if the patient should be admitted to the hospital while the evaluation is in progress. 3 Patients with high fevers, hemorrhagic symptoms, or abnormal laboratory findings should be hospitalized or placed in isolation ( Figure 1 ) . For patients with a higher severity of illness, consultation with an infectious disease or tropical/travel medicine physician is advised. 3 Patients with symptoms that suggest acute malaria (e.g., fever, altered mental status, chills, headaches, myalgias, malaise) should be admitted for observation while the evaluation is expeditiously completed. 13
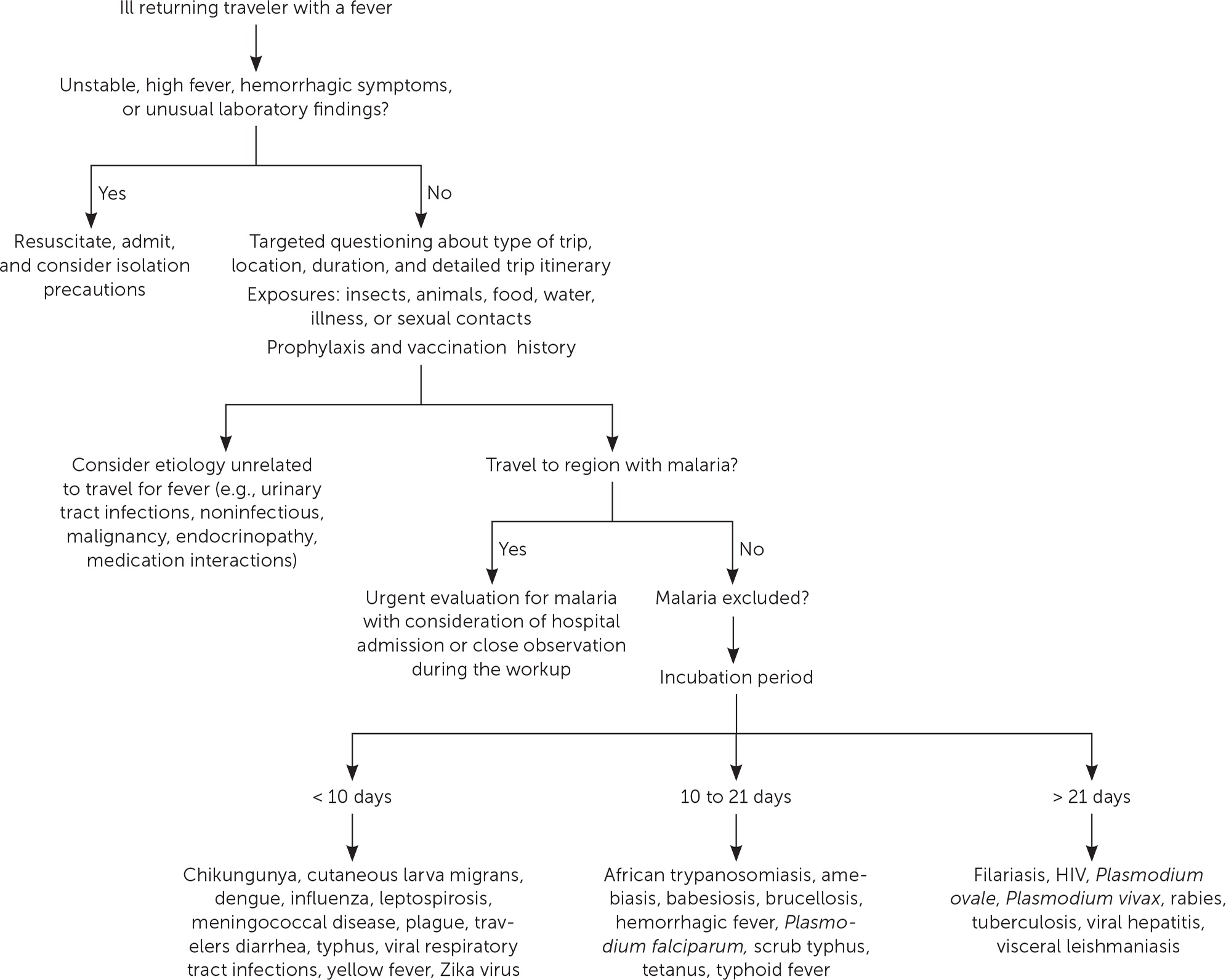
Many tools can assist physicians in making an accurate diagnosis. The GeoSentinel is a worldwide data collection network for the surveillance and research of travel-related illnesses; however, this service requires a subscription. The network can guide physicians to the most likely illness based on geographic location and top diagnoses by geography. 4 For example, Plasmodium falciparum malaria is the most common serious febrile illness in travelers to sub-Saharan Africa. 17
Ill returning travelers should have a laboratory evaluation performed with a complete blood count, comprehensive metabolic panel, and C-reactive protein. Additional testing may include blood-based rapid molecular assays for malaria and arboviruses; blood, stool, and urine cultures; and thick and thin blood smears for malaria. 3 Emerging polymerase chain reaction technologies are becoming widely available across the United States. Multiplex and biofilm array polymerase chain reaction platforms for bacterial, viral, and protozoal pathogens are now available at most tertiary health care centers. 4 Multiplex and biofilm platforms include dedicated panels for respiratory and gastrointestinal illnesses and bloodborne pathogens. These tests allow for real-time or near real-time diagnosis of agents that were previously difficult to isolate outside of the reference laboratory setting.
Table 3 lists common tropical diseases and associated vectors. 3 , 6 , 18 Physicians should be aware of unique and emerging infections, such as viral hemorrhagic fevers, COVID-19, and novel respiratory pathogens, in addition to common illnesses. Testing for infections of public health importance can be performed with assistance from local public health authorities. 19 In cases of short-term travel, previously acquired non–travel-related conditions should be on any list of applicable differential diagnoses. References on infectious diseases endemic in many geographic locations are accessible online. The Centers for Disease Control and Prevention (CDC) Travelers’ Health website provides free resources for patients and health care professionals at https://www.cdc.gov/travel .
Febrile Illness
A fever typically accompanies serious illnesses in returning travelers. Patients with a fever should be treated as moderately ill. One barrier to an accurate and early diagnosis of travel-related infections is the nonspecific nature of the initial symptoms of illness. Often, these symptoms are vague and nonfocal. A febrile illness with a fever as the primary presenting symptom could represent a viral upper respiratory tract infection, acute influenza, or even malaria, typhoid, or dengue, which are the most life-threatening. According to GeoSentinel data, 91% of ill returning travelers with an acute, life-threatening illness present with a fever. 20 All travelers who are febrile and have recently returned from a malarious area should be urgently evaluated for the disease. 13 , 21 Travelers who have symptoms of malaria should seek medical attention, regardless of whether prophylaxis or preventive measures were used. Suspicion of P. falciparum malaria is a medical emergency. 13 Clinical deterioration or death can occur in a malaria-naive patient within 24 to 36 hours. 22 Dengue is an important cause of fever in travelers returning from tropical locations. An estimated 50 million to 100 million global cases of dengue are reported annually, with many more going undetected. 23 eTable B lists the most common causes of fever in the returning traveler.
Respiratory Illness
Respiratory infections are common in the United States and throughout the world. Ill returning travelers with respiratory concerns are statistically most likely to have a viral respiratory tract infection. 24 Influenza circulates year-round in tropical climates and is one of the most common vaccine-preventable illnesses in travelers. 3 , 12 Influenza A and B frequently present with a low-grade fever, cough, congestion, myalgia, and malaise. eTable C lists the most common causes of respiratory illnesses in the returning traveler.
Gastrointestinal Illness
Gastrointestinal symptoms account for approximately one-third of returning travelers who seek medical attention. 25 Most diarrhea in travelers is self-limiting, with travelers diarrhea being the most common travel-related illness. 7 Diarrhea linked to travel in resource-poor areas is usually caused by bacterial, viral, or protozoal pathogens.
The most often encountered diarrheal pathogens are enterotoxigenic Escherichia coli and enteroaggregative E. coli , which are easily treated with commonly available antibiotics. 26 Physicians should be aware of emerging antibiotic resistance patterns across the globe. The CDC offers up-to-date travel information in the CDC Yellow Book . 3 Although patients are often concerned about parasites, they should be reassured that helminths and other parasitic infections are rare in the casual traveler. 3
The disease of concern in the setting of gastrointestinal symptoms is typhoid fever. Physicians should be aware that typhoid fever and paratyphoid fever are clinically indistinguishable, with cardinal symptoms of fever and abdominal pain. 3 Typhoid fever should be considered in ill returning travelers who do not have diarrhea, because typhoid infection may not present with diarrheal symptoms. The likelihood of typhoid fever also correlates with travel to endemic regions and should be considered an alternative diagnosis in patients not responding to antimalarial medications. A diagnosis of enteric fever can be confirmed with blood or stool cultures. Although less common, community-acquired Clostridioides difficile should be considered in the differential diagnosis in the setting of recent travel and potential antimicrobial use abroad. 27
Another important travel-related pathogen is hepatitis A due to its widespread distribution in the developing world and the small pathogen dose necessary to cause illness. Hepatitis A is a more serious infection in adults; however, many U.S. adults have been vaccinated because the hepatitis A vaccine is included in the recommended childhood immunization schedule. 28 eTable D lists the most common causes of gastrointestinal illnesses in the returning traveler.
Dermatologic Concerns
Dermatologic concerns are common among returning travelers and include noninfectious causes such as sun overexposure, contact with new or unfamiliar hygiene products, and insect bites. The most common infections in returning travelers with dermatologic concerns include cutaneous larva migrans, infected insect bites, and skin abscesses. Cutaneous larva migrans typically presents with an intensely pruritic serpiginous rash on the feet or gluteal region. 3 Questions about bites and bite avoidance measures should be asked of patients with symptomatic skin concerns; however, physicians should remember that many bites go unnoticed. 29
Formerly common illnesses in the United States are common abroad, with measles, varicella-zoster virus infection, and rubella occurring in child and adult travelers. 3 Measles is considered one of the most contagious infectious diseases. More than one-third of child travelers from the United States have not completed the recommended course of measles, mumps, and rubella vaccines at the time of travel due to immunization scheduling. One-half of all measles importations into the United States comes from these international travelers. 30 Measles should always be considered in the differential because of the low or incomplete vaccination rates in travelers and high levels of exposure in some areas abroad. eTable E lists the most common infectious causes of dermatologic concern in the returning traveler.
Data Sources: A PubMed search was completed using the key words prevention, diagnosis, treatment, travel related illness, surveillance, travel medicine, chemoprophylaxis, and returning traveler treatment. The search was limited to English-language studies published since 2000. Secondary references from the key articles identified by the search were used as well. Also searched were the Centers for Disease Control and Prevention and Cochrane databases. Search dates: September 2022 to November 2022, March 2023, and August 2023.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army, the U.S. Department of Defense, or the U.S. government.
The World Tourism Organization. International tourists to hit 1.8 billion by 2030. October 11, 2011. Accessed March 2023. https://www.unwto.org/archive/global/press-release/2011-10-11/international-tourists-hit-18-billion-2030
- Angelo KM, Kozarsky PE, Ryan ET, et al. What proportion of international travellers acquire a travel-related illness? A review of the literature. J Travel Med. 2017;24(5):10.1093/jtm/tax046.
Centers for Disease Control and Prevention. CDC Yellow Book: Health Information for International Travel . Oxford University Press; 2023. Accessed August 26, 2023. https://wwwnc.cdc.gov/travel/yellowbook/2024/table-of-contents
Wu HM. Evaluation of the sick returned traveler. Semin Diagn Pathol. 2019;36(3):197-202.
Scaggs Huang FA, Schlaudecker E. Fever in the returning traveler. Infect Dis Clin North Am. 2018;32(1):163-188.
Feder HM, Mansilla-Rivera K. Fever in returning travelers: a case-based approach. Am Fam Physician. 2013;88(8):524-530.
Giddings SL, Stevens AM, Leung DT. Traveler's diarrhea. Med Clin North Am. 2016;100(2):317-330.
Harvey K, Esposito DH, Han P, et al.; Centers for Disease Control and Prevention. Surveillance for travel-related disease–GeoSentinel Surveillance System, United States, 1997–2011. MMWR Surveill Summ. 2013;62:1-23.
Sridhar S, Turbett SE, Harris JB, et al. Antimicrobial-resistant bacteria in international travelers. Curr Opin Infect Dis. 2021;34(5):423-431.
Matteelli A, Carvalho AC, Bigoni S. Visiting relatives and friends (VFR), pregnant, and other vulnerable travelers. Infect Dis Clin North Am. 2012;26(3):625-635.
Ladhani S, Aibara RJ, Riordan FA, et al. Imported malaria in children: a review of clinical studies. Lancet Infect Dis. 2007;7(5):349-357.
Sanford C, McConnell A, Osborn J. The pretravel consultation. Am Fam Physician. 2016;94(8):620-627.
Shahbodaghi SD, Rathjen NA. Malaria. Am Fam Physician. 2022;106(3):270-278.
Freedman DO, Chen LH, Kozarsky PE. Medical considerations before international travel. N Engl J Med. 2016;375(3):247-260.
- Marti F, Steffen R, Mutsch M. Influenza vaccine: a travelers' vaccine? Expert Rev Vaccines. 2008;7(5):679-687.
Vivancos R, Abubakar I, Hunter PR. Foreign travel, casual sex, and sexually transmitted infections: systematic review and meta-analysis. Int J Infect Dis. 2010;14(10):e842-e851.
Paquet D, Jung L, Trawinski H, et al. Fever in the returning traveler. Dtsch Arztebl Int. 2022;119(22):400-407.
Cantey PT, Montgomery SP, Straily A. Neglected parasitic infections: what family physicians need to know—a CDC update. Am Fam Physician. 2021;104(3):277-287.
Rathjen NA, Shahbodaghi SD. Bioterrorism. Am Fam Physician. 2021;104(4):376-385.
Jensenius M, Davis X, von Sonnenburg F, et al.; Geo-Sentinel Surveillance Network. Multicenter GeoSentinel analysis of rickettsial diseases in international travelers, 1996–2008. Emerg Infect Dis. 2009;15(11):1791-1798.
Tolle MA. Evaluating a sick child after travel to developing countries. J Am Board Fam Med. 2010;23(6):704-713.
Centers for Disease Control and Prevention. About malaria. February 2, 2022. Accessed August 21, 2022. https://www.cdc.gov/malaria/about/index.html
Wilder-Smith A, Schwartz E. Dengue in travelers. N Engl J Med. 2005;353(9):924-932.
Summer A, Stauffer WM. Evaluation of the sick child following travel to the tropics. Pediatr Ann. 2008;37(12):821-826.
Swaminathan A, Torresi J, Schlagenhauf P, et al.; GeoSentinel Network. A global study of pathogens and host risk factors associated with infectious gastrointestinal disease in returned international travellers. J Infect. 2009;59(1):19-27.
Shah N, DuPont HL, Ramsey DJ. Global etiology of travelers' diarrhea: systematic review from 1973 to the present. Am J Trop Med Hyg. 2009;80(4):609-614.
Michal Stevens A, Esposito DH, Stoney RJ, et al.; GeoSentinel Surveillance Network. Clostridium difficile infection in returning travellers. J Travel Med. 2017;24(3):1-6.
Mayer CA, Neilson AA. Hepatitis A - prevention in travellers. Aust Fam Physician. 2010;39(12):924-928.
Herness J, Snyder MJ, Newman RS. Arthropod bites and stings. Am Fam Physician. 2022;106(2):137-147.
Bangs AC, Gastañaduy P, Neilan AM, et al. The clinical and economic impact of measles-mumps-rubella vaccinations to prevent measles importations from U.S. pediatric travelers returning from abroad. J Pediatric Infect Dis Soc. 2022;11(6):257-266.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2023 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 10 - Vietnam
- Section 11 - Rapid Diagnostic Tests for Infectious Diseases
General Approach to the Returned Traveler
Cdc yellow book 2024.
Author(s): Jessica Fairley
The Posttravel Evaluation
Common syndromes, general management.
As many as 43%–79% of travelers to low- and middle-income countries become ill with a travel-associated health problem. Although most of these illnesses are mild, some travelers become sick enough to seek care from a health care provider. Most posttravel infections become apparent soon after returning from abroad, but incubation periods vary, and some syndromes can present months to years after initial infection or after travel.
When evaluating a patient with a probable travel-associated illness, approach the differential diagnosis by incorporating both the patient presentation and risk factors related to travel (e.g., destination, duration of travel, and exposures; see Table 11-01 ). Salient points of the history of present illness and the travel and medical history, descriptions of common nonfebrile syndromes, and initial management steps are outlined below. The differential diagnosis and management for a traveler with fever (or febrile syndrome) is discussed in detail in Sec. 11, Ch. 4, Fever in the Returned Traveler .
Table 11-01 Elements of a complete travel history in an ill returned traveler
HISTORY OF THE PRESENT ILLNESS
Symptoms: primary & associated
Date of symptom or illness onset
Geographic location at time of symptom onset (e.g., while away, in transit, after return)
Healthcare received while abroad and after return (e.g., medications, hospitalizations)
TRAVEL DETAILS
Destinations visited and itineraries
Duration of travel (date of departure and date of return)
Reason for travel
- Business (include details about possible exposures and type of work done)
- Immigration
- Missionary, volunteer, humanitarian aid work
- Providing or receiving medical care
- Research or education
- Visiting friends & relatives
Accommodations and sleeping arrangements
- Hotel with or without air conditioning, window screens, or mosquito nets
- Safari, including camping outdoors, in a lodge, in a luxury tent
- Someone’s home
Transportation used
RECREATIONAL ACTIVITIES
Camping and hiking
Sightseeing
Water exposures
- Boating or rafting
- Fresh water (lake, river, stream) bathing, boating, swimming, wading
- Hot springs
- Hot tubs, swimming pools
- Ocean (diving, snorkeling, surfing; consider marine life exposure)
Other activities
Animal or arthropod bites, stings, scratches
Drinking water (bottled, purified, tap, use of ice)
- Raw fruits, vegetables
- Undercooked meat
- Unpasteurized dairy products
Insect bites (mosquito, tick, sand fly, tsetse fly)
Medical or dental care (planned or unplanned)
Disease outbreaks in visited destinations
Sexual activity during travel (document condom use, new partner[s])
Tattoos or piercings while traveling
VECTORBORNE DISEASE PRECAUTIONS
Adherence to malaria prophylaxis
Insect repellent use (25%–40% DEET or other Environmental Protection Agency–registered product)
Mosquito nets
VACCINES RECEIVED
Coronavirus disease 2019 (COVID-19)
Hepatitis A
Hepatitis B
Japanese encephalitis
Measles-mumps-rubella (MMR)
Meningococcal disease
Tetanus-diphtheria-acellular pertussis (Tdap)
Yellow fever
MEDICATIONS TAKEN
Malaria prophylaxis
All medicines taken (whether routinely or for symptomatic treatment), including antibiotics
- Herbal, complementary, alternative
- Over the counter
- Prescription
PAST MEDICAL HISTORY
Chronic medical conditions
- Autoimmune disease
- Heart disease
- Immunosuppressive conditions
Recent illnesses or surgeries
ADDITIONAL INFORMATION
Alcohol, tobacco, illicit drug use
Family history
Recent travel, domestic or international, especially ≤6 months
History of the Present Illness
As with any medical evaluation, the history of the present illness and associated clinical factors are the first considerations when approaching an ill returned traveler. Information about the timing of illness, immunization and prophylaxis history, itinerary, exposures, and comorbidities can help refine the diagnosis.
Timing of Illness in Relation to Travel
Because most common travel-associated infections have short incubation periods, most ill travelers will seek medical attention ≤1 month of returning from their destinations. Dengue and other arboviral infections, influenza, and travelers’ diarrhea are examples of infections with shorter incubation periods (<2 weeks). Diseases with slightly longer incubation periods, ≤4–6 weeks, include viral hepatitis, acute HIV, leishmaniasis, malaria, and typhoid fever, among others. Occasionally, some infections (e.g., leishmaniasis, malaria, schistosomiasis, tuberculosis) might become manifest months or even years after a traveler returns. Consider malaria in the differential diagnosis of any traveler who traveled to a malaria-endemic area ≤1 year of presentation. A detailed travel history that extends beyond a few months before presentation is important. The most common travel-associated infections by incubation period are listed in Table 11-02 , Table 11-03 , and Table 11-04 .
Table 11-02 Common travel-associated infections by incubation period: <14 days
Table 11-03 common travel-associated infections by incubation period: 14 days–6 weeks, table 11-04 common travel-associated infections by incubation period: >6 weeks, immunization & prophylaxis history.
When evaluating an ill returned traveler, review the traveler’s vaccination history and malaria prophylaxis used. Fewer than half of US travelers who visit low- and middle-income countries seek pretravel medical advice, increasing the likelihood that they did not receive pretravel vaccines and did not receive or take antimalarial drugs. Although adherence to malaria prophylaxis does not rule out the possibility of malaria, it substantially reduces the risk and increases the possibility of an alternative diagnosis.
Likewise, history of vaccination against hepatitis A and yellow fever would make these diseases unlikely causes of hepatitis or jaundice in a returning traveler. Remember to ask about routine vaccinations like measles-mumps-rubella (MMR) and tetanus-diphtheria-pertussis (Tdap). The most common vaccine-preventable diseases among returned travelers seeking care at GeoSentinel clinics during 1997–2010 included hepatitis A, hepatitis B, influenza, and typhoid fever. More than half of these patients with vaccine-preventable diseases were hospitalized.
Itinerary & Travel Duration
A traveler’s itinerary is crucial to formulating a differential diagnosis because exposures differ depending on the region of travel and the specific areas (e.g., rural vs. urban). A febrile illness with nonspecific symptoms could be dengue, malaria, rickettsial disease, or typhoid fever, among others, depending on the itinerary and endemicity of these infections. Being able to exclude certain infections based on the travel itinerary can help avoid unnecessary testing.
A 2013 study from the GeoSentinel Surveillance Network found that the frequency of certain diseases varied depending on the region of the world visited; among travelers with fevers, for example, dengue was diagnosed most frequently among travelers coming from Asia, while malaria was diagnosed most frequently among travelers returning from Africa.
Travel duration is also a factor because the risk for a travel-associated illness increases with the length of the trip. A tropical medicine specialist can assist with the differential diagnosis and might be aware of outbreaks or the current prevalence of an infectious disease in an area. The 2014–2015 Ebola virus epidemic in West Africa highlighted the importance of epidemiologic factors and travel itineraries in managing patients and protecting staff and the community.
Knowing a patient’s exposures during travel (e.g., consumption of contaminated food or water, insect bites, freshwater swimming) also can assist with the differential diagnosis. In addition to malarial parasites, mosquitoes transmit viruses (e.g., chikungunya, dengue, yellow fever, Zika) and filarial parasites (e.g., Wuchereria bancrofti ). Depending on the clinical syndrome, a history of a tick bite could suggest a diagnosis of tick-borne encephalitis, African tick-bite fever, or other rickettsial infections. Tsetse flies are the vector for transmission of Trypanosoma brucei , a protozoan that causes African sleeping sickness. Tsetse flies are large, and their bites are painful; patients often recall being bitten. Freshwater bathing, swimming, wading, or other contact can put travelers at risk for leptospirosis, schistosomiasis, and other diseases.
Accommodations and activities also can influence the risk of acquiring certain diseases while abroad. Travelers who visit friends and relatives are at greater risk for malaria, typhoid fever, and other diseases, often because they stay longer, travel to more remote destinations, have more contact with local water sources, and typically do not seek pretravel advice (see Sec. 9, Ch. 9, Visiting Friends & Relatives: VFR Travel ). Travelers backpacking and camping in rural areas have a greater risk for certain diseases than those staying in luxury, air-conditioned hotels.
Comorbidities
Underlying illnesses can affect a traveler’s susceptibility to infection as well as the clinical manifestations and severity of disease. An increasing number of international travelers are immunosuppressed, whether due to HIV infection, treatment with immune-modulating medications, being an organ transplant recipient, or other primary or acquired immunodeficiencies (see Sec. 3, Ch. 1, Immunocompromised Travelers ). In addition, several factors associated with travel can exacerbate underlying conditions (e.g., chronic lung disease, inflammatory bowel disease, ischemic heart disease).
Symptoms & Illness Severity
Although the symptoms of many infectious and travel-associated syndromes overlap, the initial symptoms and presentation should ultimately guide the differential diagnosis: gastrointestinal symptoms and febrile illnesses are the most common syndromes in returning travelers. Remember that conditions such as appendicitis, urinary tract infections, and domestically acquired viral infections also can present in returning travelers.
Severity of illness is not only important for patient triage but also can help clinicians distinguish certain infections. Is the traveler hemodynamically stable? Is the infection potentially life-threatening (e.g., malaria)? Does the traveler have a severe respiratory syndrome or signs of hemorrhagic fever? Some suspected illnesses might necessitate prompt involvement of public health authorities. For more details, see General Management, later in this chapter.
The 3 most common clinical syndromes after travel to low- and middle-income countries are dermatologic conditions, diarrheal diseases, and systemic febrile illnesses, each of which is described in more detail elsewhere in this section (see Dermatologic Conditions , Persistent Diarrhea in Returned Travelers , and Fever in the Returned Traveler ). Evaluate febrile travelers returning from malaria-endemic destinations immediately. Other common clinical presentations and findings include animal bites and scratches, asymptomatic eosinophilia, and respiratory illnesses.
Animal Bites & Scratches
Promptly evaluate any traveler who reports animal exposures during travel (see Sec. 4, Ch. 7, Zoonotic Exposures: Bites, Stings, Scratches & Other Hazards ). Consider travelers with animal bites and scratches as high-risk for rabies exposure, and provide rabies postexposure prophylaxis, as indicated (see Sec. 5, Part 2, Ch. 18, Rabies ). If the traveler was exposed to a macaque, herpes B postexposure prophylaxis might be indicated (see Sec. 5, Part 2, Ch. 1, B Virus ).
Asymptomatic Eosinophilia
Eosinophilia in a returning traveler suggests possible helminth infection. Allergic diseases, hematologic disorders, and a few other viral, fungal, and protozoan infections also can cause eosinophilia. Eosinophilia can be present during pulmonary migration of parasites (e.g., Ascaris , hookworm, schistosomiasis, Strongyloides ).
Other parasitic infections associated with eosinophilia include lymphatic filariasis, chronic strongyloidiasis, acute trichinellosis, and visceral larva migrans. These infections might be asymptomatic, but also could have associated symptoms (e.g., rash, swelling). In an outbreak of sarcocystosis among travelers returning from Tioman Island, Malaysia, those affected presented with eosinophilia and myalgias and had eosinophilic myositis on muscle biopsy (see Sec. 5, Part 3, Ch. 18, Sarcocystosis ).
Parasitic infections are rare in most travelers, so consider other etiologies for eosinophilia; for instance, eosinophilia can be a sign of a hematologic malignancy. See Section 5 for more information on specific diseases.
Respiratory Illnesses
Respiratory illnesses are frequent among returned travelers and are typically associated with common respiratory viruses, including influenza and now, severe acute respiratory syndrome coronavirus 2, the cause of coronavirus disease 2019 (COVID-19). Since the pandemic began in early 2020, coronavirus disease (COVID-19) has overtaken influenza in overall global incidence. And although historically influenza has been the most common vaccine-preventable disease associated with international travel, COVID-19 could surpass it in that regard. To make that determination, however, a better understanding of the epidemiology of travel-associated COVID-19 transmission is needed (see Sec. 5, Part 2, Ch. 3, COVID-19 ).
If the travel history is appropriate and respiratory symptoms do not have a clear alternative diagnosis, include other emerging respiratory infections (e.g., avian influenza, Middle East respiratory syndrome [MERS]) in the differential diagnosis. In suspected cases of an emerging respiratory infection, alert local public health authorities and the Centers for Disease Control and Prevention (CDC) immediately. See relevant chapters in Section 5 for more information on these emerging infections; for a list of febrile respiratory illnesses that can occur after exposures in tropical destinations, see Table 11-10 in the chapter, Fever in the Returned Traveler .
Delayed illness onset and chronic cough after travel could be tuberculosis, especially in a long-term traveler or health care worker. Helminths and helminth infections associated with pulmonary symptoms include Ascaris , hookworms ( Ancylostoma or Necator ), paragonimiasis, schistosomiasis, and strongyloidiasis.
Most posttravel illnesses can be managed on an outpatient basis, but some patients, especially those with systemic febrile illnesses, might need to be hospitalized. Furthermore, potentially severe, transmissible infections (e.g., COVID-19, Ebola, MERS) require enhanced infection control measures and often, higher levels of care. Severe clinical presentations (e.g., acute respiratory distress, hemodynamic instability, mental status changes) require inpatient care. Have a low threshold for admitting a febrile patient if malaria is suspected; complications can occur rapidly. Management in an inpatient setting is especially vital for patients unlikely to follow up reliably or who have no one at home to assist if symptoms quickly worsen.
Initial Evaluation
After conducting a thorough physical exam, paying particular attention to skin manifestations or evidence of prior insect bites, order tests based on chief complaint and exposure history. Frequently useful tests include complete blood count with differential (to look for anemia, eosinophilia, leukocytosis, leukopenia, thrombocytopenia); blood cultures and malaria rapid diagnostic tests (depending on the presence of fever and travel itinerary); a complete metabolic profile (to identify electrolyte, renal, or liver dysfunction); serologic or PCR tests for arboviral infections (as needed); and stool cultures and ova and parasite exams. These tests often can help narrow the differential diagnosis and determine disease severity.
Antimicrobial Resistance
Be aware of the risk to international travelers for acquiring antimicrobial resistant organisms. Carefully consider travel history when caring for patients, both to identify effective treatments for infections and to ensure infection control interventions are in place to prevent spread of antimicrobial resistance (see Sec. 11, Ch. 5, Antimicrobial Resistance ).
Consultation
Consult an infectious disease specialist when managing complicated or severe travel-associated infections, or when the diagnosis remains unclear. A tropical medicine or infectious disease specialist should be involved in cases that require specialized treatment (e.g., leishmaniasis, severe malaria, and neurocysticercosis).
Involve local, state, and federal public health authorities whenever managing transmissible, high-consequence infections. CDC provides on-call assistance with the diagnosis and management of parasitic infections at 404-718-4745 (for parasitic infections other than malaria) or 770-488-7788 (toll-free at 855-856-4713) for malaria, during business hours. After business hours or for other conditions, call the CDC Emergency Operations Center at 770-488-7100.
The following authors contributed to the previous version of this chapter: Jessica K. Fairley
Bibliography
Angelo KM, Kozarsky PE, Ryan ET, Chen LH, Sotir MJ. What proportion of international travellers acquire a travel-related illness? A review of the literature. J Travel Med. 2017;24(5):tax046.
Boggild AK, Castelli F, Gautret P, Torresi J, von Sonnenburg F, Barnett ED, et al. Vaccine preventable diseases in returned international travelers: results from the GeoSentinel Surveillance Network. Vaccine. 2010;28(46):7389–95.
Centers for Disease Control and Prevention. Notes from the field: acute muscular sarcocystosis among returning travelers—Tioman Island, Malaysia, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(2):37–8.
Chen LH, Wilson ME, Davis X, Loutan L, Schwartz E, Keystone J, et al. Illness in long-term travelers visiting GeoSentinel clinics. Emerg Infect Dis. 2009;15(11):1773–82.
Fairley JK, Kozarsky PE, Kraft CS, Guarner J, Steinberg JP, Anderson E, et al. Ebola or not? Evaluating the ill traveler from Ebola-affected countries in West Africa. Open Forum Infect Dis. 2016;3(1):ofw005.
Hamer DH, Connor BA. Travel health knowledge, attitudes and practices among United States travelers. J Travel Med. 2004;11(1):23–6.
Hendel-Paterson B, Swanson SJ. Pediatric travelers visiting friends and relatives (VFR) abroad: illnesses, barriers and pre-travel recommendations. Travel Med Infect Dis. 2011;9(4):192–203.
Leder K, Torresi J, Libman MD, Cramer JP, Castelli F, Schlagenhauf P, et al. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med. 2013;158(6):456–68.
Ryan ET, Wilson ME, Kain KC. Illness after international travel. N Engl J Med. 2002;347(7):505–16.
Schulte C, Krebs B, Jelinek T, Nothdurft HD, von Sonnenburg F, Loscher T. Diagnostic significance of blood eosinophilia in returning travelers. Clin Infect Dis. 2002;34(3):407–11.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Medications for Motion Sickness
Other names: Sea Sickness
A disturbance of the inner ear that is caused by repeated motion
Drugs used to treat Motion Sickness
The medications listed below are related to or used in the treatment of this condition.
Frequently asked questions
- What is the Benadryl hat man?
- How long does Benadryl take to work?
- Does Benadryl help with or cause anxiety?
- Does Benadryl make you sleepy?
- Diphenhydramine Hydrochloride vs Citrate: What's the difference?
- Does Ginger interact with any drugs?
- Can you take Benadryl while pregnant?
View more FAQ
Alternative treatments for Motion Sickness
The following products are considered to be alternative treatments or natural remedies for Motion Sickness. Their efficacy may not have been scientifically tested to the same degree as the drugs listed in the table above. However, there may be historical, cultural or anecdotal evidence linking their use to the treatment of Motion Sickness.
- Dramamine Non Drowsy
Learn more about Motion Sickness
Care guides.
- Motion Sickness
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Medical Disclaimer

IMAGES
COMMENTS
Scopolamine - the most commonly prescribed medication for motion sickness. It must be taken before symptoms start. It is available as a patch that is placed behind the ear 6-8 hours before ...
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant. When you visit a place where the climate or sanitary practices are ...
Motion Sickness. Motion sickness happens when the movement you see is different from what your inner ear senses. This can cause dizziness, nausea, and vomiting. You can get motion sick in a car, or on a train, airplane, boat, or amusement park ride. Motion sickness can make traveling unpleasant, but there are strategies to prevent and treat it.
Avian Flu (Bird Flu) COVID-19. Chagas Disease (American Trypanosomiasis) Chikungunya. Cholera. Crimean-Congo Hemorrhagic fever. Dengue. Diphtheria. Ebola and Marburg.
Motion sickness is a common condition that happens when you're in motion, like riding in a vehicle, while sitting still. It happens when your eyes, inner ear and body send conflicting messages to your brain. ... Motion sickness can make travel a miserable experience and take the fun out of playing a video game or an immersive virtual reality ...
Motion sickness (travel sickness) is common, especially in children. It is caused by repeated unusual movements during travelling, which send strong (sometimes confusing) signals to the balance and position sensors in the brain.
There are different types of travel-associated infections that cause fever, along with other symptoms to include diarrhea, vomiting, rashes, and muscle aches. The most common of these include malaria, dengue, typhoid fever, and chikungunya. Malaria. Malaria is a parasitic disease spread by mosquitoes in tropical and subtropical climates.
Fewer vaccinated people, making infectious diseases more common; Poor infrastructure, leading to contaminated food and water; Warmer weather, which allows bacteria, parasites and mosquitos to thrive; The Most Common Travel-Related Illnesses. Some of the most common illnesses that people contract while traveling are: Colds
Common travel-related diseases and their symptoms include: Malaria — Though the disease can lay dormant for as long as a year, symptoms include those of the flu, such as chills and high fever. Tuberculosis — Chest pain, weight loss, chills or fever, loss of appetite, night sweats, or a cough that lasts three or more weeks and produces blood ...
To identify travel-related diseases and facilitate rapid communication between clinicians and public health professionals globally, a surveillance system (e.g., GeoSentinel) is needed. ... of global travel-related disease surveillance so that clinicians and public health professionals are aware of the most common travel-related illnesses and ...
Most people see a healthcare provider for motion sickness ahead of planned travel, in order to seek preventive treatment, but other situations do arise. The most common complications of motion sickness include vomiting that leads to dehydration and electrolyte imbalances, which can be treated easily.
Motion sickness; Other names: Kinetosis, travel sickness, seasickness, airsickness, carsickness, simulation sickness, space motion sickness, ... A specific form of terrestrial motion sickness, being carsick is quite common and evidenced by disorientation while reading a map, a book, or a small screen during travel. Carsickness results from the ...
The main infectious diseases to which travellers may be exposed, and precautions for each, are detailed in the Chapter 5 of the International travel and health situation publication.The most common infectious illness to affect travellers, namely travellers' diarrhoea, is covered in Chapter 3 of the International travel and health situation publication.
Motion sickness is caused by repeated movements when travelling, like going over bumps in a car or moving up and down in a boat, plane or train. The inner ear sends different signals to your brain from those your eyes are seeing. These confusing messages cause you to feel unwell. Find out more about motion sickness, an unpleasant combination of ...
Dengue. Dengue is another common travel disease spread through mosquito bites. It is common in tropical and subtropical regions, including the Caribbean, Central and South America, Western Pacific Islands, Australia, Southeast Asia, and Africa. Symptoms include fever, headache, nausea, vomiting, rash, pain in the eyes, joints, and muscles, and ...
Reading while travelling is among the most common causes of car sickness. 10 most common causes of travel sickness. Reading (39%) Travelling backwards (38%) Sitting in the back seat (31%)
What is Motion Sickness? Kinetosis — commonly known as motion sickness — is any disorder caused by motion, such as seasickness, airsickness or carsickness, as defined by Taber's Cyclopedic Medical Dictionary. It is a common complaint of travelers on boats or planes, in motor vehicles, and even while riding animals such as horses.
Table 3 lists common tropical diseases and associated vectors. 3, 6, 18 Physicians should ... with travelers diarrhea being the most common travel-related illness. 7 Diarrhea linked to travel in ...
Common Syndromes. General Management. As many as 43%-79% of travelers to low- and middle-income countries become ill with a travel-associated health problem. Although most of these illnesses are mild, some travelers become sick enough to seek care from a health care provider. Most posttravel infections become apparent soon after returning ...
Other common diseases include fevers, like yellow fever or dengue fever, which often spread through mosquitos or other insect bites. If you get any of these conditions, controlling the fever is vital to preventing serious complications. Recognizing the Symptoms of Travel-Related Sicknesses . You're likely familiar with cold and flu symptoms ...
Diarrheal diseases are the most common travel-related illness. They are acquired from eating contaminated food or water. Pepto-Bismol prophylaxis might be something to consider, or taking it at ...
The following products are considered to be alternative treatments or natural remedies for Motion Sickness. Their efficacy may not have been scientifically tested to the same degree as the drugs listed in the table above. However, there may be historical, cultural or anecdotal evidence linking their use to the treatment of Motion Sickness.