Drug combinations
WARNING! For educational purposes: We do not endorse any of these combinations. This page will always be 'work in progress'. It is extremely important to be safe at all times! See below the graphic for important information regarding specific combinations.
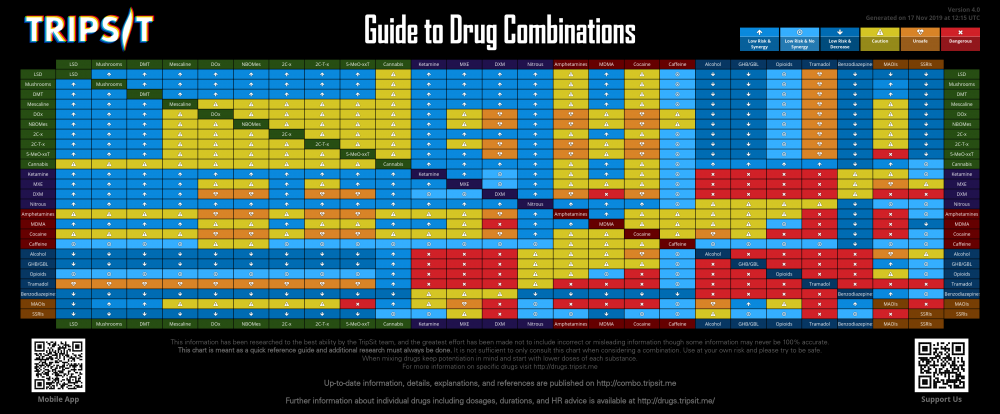
- 2 Categorisations
- 3 Chart versions
- 4 Use & Attribution
- 5.1 cannabis & lsd
- 5.2 amphetamines & lsd
- 5.3 cocaine & lsd
- 5.4 tramadol & lsd
- 5.5 cannabis & mushrooms
- 5.6 amphetamines & mushrooms
- 5.7 cocaine & mushrooms
- 5.8 tramadol & mushrooms
- 5.9 cannabis & dmt
- 5.10 amphetamines & dmt
- 5.11 cocaine & dmt
- 5.12 tramadol & dmt
- 5.13 5-meo-xxt & mescaline
- 5.14 cannabis & mescaline
- 5.15 amphetamines & mescaline
- 5.16 cocaine & mescaline
- 5.17 caffeine & mescaline
- 5.18 tramadol & mescaline
- 5.19 5-meo-xxt & dox
- 5.20 cannabis & dox
- 5.21 ketamine & dox
- 5.22 mxe & dox
- 5.23 dxm & dox
- 5.24 pcp & dox
- 5.25 amphetamines & dox
- 5.26 mdma & dox
- 5.27 cocaine & dox
- 5.28 caffeine & dox
- 5.29 alcohol & dox
- 5.30 opioids & dox
- 5.31 tramadol & dox
- 5.32 maois & dox
- 5.33 5-meo-xxt & nbomes
- 5.34 cannabis & nbomes
- 5.35 mxe & nbomes
- 5.36 amphetamines & nbomes
- 5.37 cocaine & nbomes
- 5.38 caffeine & nbomes
- 5.39 tramadol & nbomes
- 5.40 maois & nbomes
- 5.41 5-meo-xxt & 2c-x
- 5.42 cannabis & 2c-x
- 5.43 amphetamines & 2c-x
- 5.44 cocaine & 2c-x
- 5.45 caffeine & 2c-x
- 5.46 tramadol & 2c-x
- 5.47 maois & 2c-x
- 5.48 5-meo-xxt & 2c-t-x
- 5.49 cannabis & 2c-t-x
- 5.50 amphetamines & 2c-t-x
- 5.51 cocaine & 2c-t-x
- 5.52 caffeine & 2c-t-x
- 5.53 alcohol & 2c-t-x
- 5.54 opioids & 2c-t-x
- 5.55 maois & 2c-t-x
- 5.56 cannabis & amt
- 5.57 caffeine & amt
- 5.58 alcohol & amt
- 5.59 opioids & amt
- 5.60 maois & amt
- 5.61 mxe & 5-meo-xxt
- 5.62 dxm & 5-meo-xxt
- 5.63 cannabis & 5-meo-xxt
- 5.64 amphetamines & 5-meo-xxt
- 5.65 mdma & 5-meo-xxt
- 5.66 cocaine & 5-meo-xxt
- 5.67 caffeine & 5-meo-xxt
- 5.68 amphetamines & cannabis
- 5.69 mdma & cannabis
- 5.70 cocaine & cannabis
- 5.71 alcohol & cannabis
- 5.72 amphetamines & ketamine
- 5.73 mdma & ketamine
- 5.74 cocaine & ketamine
- 5.75 caffeine & ketamine
- 5.76 alcohol & ketamine
- 5.77 ghb/gbl & ketamine
- 5.78 opioids & ketamine
- 5.79 benzodiazepines & ketamine
- 5.80 maois & ketamine
- 5.81 pcp & mxe
- 5.82 amphetamines & mxe
- 5.83 mdma & mxe
- 5.84 cocaine & mxe
- 5.85 caffeine & mxe
- 5.86 alcohol & mxe
- 5.87 ghb/gbl & mxe
- 5.88 opioids & mxe
- 5.89 benzodiazepines & mxe
- 5.90 maois & mxe
- 5.91 ssris & mxe
- 5.92 amphetamines & dxm
- 5.93 cocaine & dxm
- 5.94 caffeine & dxm
- 5.95 alcohol & dxm
- 5.96 ghb/gbl & dxm
- 5.97 opioids & dxm
- 5.98 benzodiazepines & dxm
- 5.99 maois & dxm
- 5.100 ssris & dxm
- 5.101 amphetamines & pcp
- 5.102 mdma & pcp
- 5.103 cocaine & pcp
- 5.104 caffeine & pcp
- 5.105 alcohol & pcp
- 5.106 ghb/gbl & pcp
- 5.107 opioids & pcp
- 5.108 benzodiazepines & pcp
- 5.109 maois & pcp
- 5.110 ssris & pcp
- 5.111 alcohol & nitrous
- 5.112 ghb/gbl & nitrous
- 5.113 opioids & nitrous
- 5.114 tramadol & nitrous
- 5.115 mdma & amphetamines
- 5.116 cocaine & amphetamines
- 5.117 caffeine & amphetamines
- 5.118 alcohol & amphetamines
- 5.119 ghb/gbl & amphetamines
- 5.120 opioids & amphetamines
- 5.121 tramadol & amphetamines
- 5.122 benzodiazepines & amphetamines
- 5.123 maois & amphetamines
- 5.124 cocaine & mdma
- 5.125 caffeine & mdma
- 5.126 alcohol & mdma
- 5.127 ghb/gbl & mdma
- 5.128 tramadol & mdma
- 5.129 maois & mdma
- 5.130 caffeine & cocaine
- 5.131 alcohol & cocaine
- 5.132 ghb/gbl & cocaine
- 5.133 opioids & cocaine
- 5.134 tramadol & cocaine
- 5.135 maois & cocaine
- 5.136 ssris & cocaine
- 5.137 ghb/gbl & alcohol
- 5.138 opioids & alcohol
- 5.139 tramadol & alcohol
- 5.140 benzodiazepines & alcohol
- 5.141 maois & alcohol
- 5.142 ssris & alcohol
- 5.143 opioids & ghb/gbl
- 5.144 tramadol & ghb/gbl
- 5.145 benzodiazepines & ghb/gbl
- 5.146 tramadol & opioids
- 5.147 benzodiazepines & opioids
- 5.148 maois & opioids
- 5.149 ssris & opioids
- 5.150 benzodiazepines & tramadol
- 5.151 LSD & Mushrooms
- 5.152 LSD & DMT
- 5.153 LSD & Mescaline
- 5.154 LSD & DOx
- 5.155 LSD & NBOMes
- 5.156 LSD & 2C-x
- 5.157 LSD & 2C-T-x
- 5.158 LSD & αMT
- 5.159 LSD & 5-MeO-xxT
- 5.160 LSD & Cannabis
- 5.161 LSD & Ketamine
- 5.162 LSD & MXE
- 5.163 LSD & DXM
- 5.164 LSD & Nitrous
- 5.165 LSD & Amphetamines
- 5.166 LSD & MDMA
- 5.167 LSD & Cocaine
- 5.168 LSD & Caffeine
- 5.169 LSD & Alcohol
- 5.170 LSD & GHB\GBL
- 5.171 LSD & Opioids
- 5.172 LSD & Tramadol
- 5.173 LSD & Benzodiazepines
- 5.174 LSD & MAOIs
- 5.175 LSD & SSRIs
- 5.176 Mushrooms & DMT
- 5.177 Mushrooms & Mescaline
- 5.178 Mushrooms & DOx
- 5.179 Mushrooms & NBOMes
- 5.180 Mushrooms & 2C-x
- 5.181 Mushrooms & 2C-T-x
- 5.182 Mushrooms & αMT
- 5.183 Mushrooms & 5-MeO-xxT
- 5.184 Mushrooms & Cannabis
- 5.185 Mushrooms & Ketamine
- 5.186 Mushrooms & MXE
- 5.187 Mushrooms & DXM
- 5.188 Mushrooms & Nitrous
- 5.189 Mushrooms & Amphetamines
- 5.190 Mushrooms & MDMA
- 5.191 Mushrooms & Cocaine
- 5.192 Mushrooms & Caffeine
- 5.193 Mushrooms & Alcohol
- 5.194 Mushrooms & GHB\GBL
- 5.195 Mushrooms & Opioids
- 5.196 Mushrooms & Tramadol
- 5.197 Mushrooms & Benzodiazepines
- 5.198 Mushrooms & MAOIs
- 5.199 Mushrooms & SSRIs
- 5.200 DMT & Mescaline
- 5.201 DMT & DOx
- 5.202 DMT & NBOMes
- 5.203 DMT & 2C-x
- 5.204 DMT & 2C-T-x
- 5.205 DMT & αMT
- 5.206 DMT & 5-MeO-xxT
- 5.207 DMT & Cannabis
- 5.208 DMT & Ketamine
- 5.209 DMT & MXE
- 5.210 DMT & DXM
- 5.211 DMT & Nitrous
- 5.212 DMT & Amphetamines
- 5.213 DMT & MDMA
- 5.214 DMT & Cocaine
- 5.215 DMT & Caffeine
- 5.216 DMT & Alcohol
- 5.217 DMT & GHB\GBL
- 5.218 DMT & Opioids
- 5.219 DMT & Tramadol
- 5.220 DMT & Benzodiazepines
- 5.221 DMT & MAOIs
- 5.222 DMT & SSRIs
- 5.223 Mescaline & DOx
- 5.224 Mescaline & NBOMes
- 5.225 Mescaline & 2C-x
- 5.226 Mescaline & 2C-T-x
- 5.227 Mescaline & αMT
- 5.228 Mescaline & 5-MeO-xxT
- 5.229 Mescaline & Cannabis
- 5.230 Mescaline & Ketamine
- 5.231 Mescaline & MXE
- 5.232 Mescaline & DXM
- 5.233 Mescaline & Nitrous
- 5.234 Mescaline & Amphetamines
- 5.235 Mescaline & MDMA
- 5.236 Mescaline & Cocaine
- 5.237 Mescaline & Caffeine
- 5.238 Mescaline & Alcohol
- 5.239 Mescaline & GHB\GBL
- 5.240 Mescaline & Opioids
- 5.241 Mescaline & Tramadol
- 5.242 Mescaline & Benzodiazepines
- 5.243 Mescaline & MAOIs
- 5.244 Mescaline & SSRIs
- 5.245 DOx & NBOMes
- 5.246 DOx & 2C-x
- 5.247 DOx & 2C-T-x
- 5.248 DOx & αMT
- 5.249 DOx & 5-MeO-xxT
- 5.250 DOx & Cannabis
- 5.251 DOx & Ketamine
- 5.252 DOx & MXE
- 5.253 DOx & DXM
- 5.254 DOx & Nitrous
- 5.255 DOx & Amphetamines
- 5.256 DOx & MDMA
- 5.257 DOx & Cocaine
- 5.258 DOx & Caffeine
- 5.259 DOx & Alcohol
- 5.260 DOx & GHB\GBL
- 5.261 DOx & Opioids
- 5.262 DOx & Tramadol
- 5.263 DOx & Benzodiazepines
- 5.264 DOx & MAOIs
- 5.265 DOx & SSRIs
- 5.266 NBOMes & 2C-x
- 5.267 NBOMes & 2C-T-x
- 5.268 NBOMes & αMT
- 5.269 NBOMes & 5-MeO-xxT
- 5.270 NBOMes & Cannabis
- 5.271 NBOMes & Ketamine
- 5.272 NBOMes & MXE
- 5.273 NBOMes & DXM
- 5.274 NBOMes & Nitrous
- 5.275 NBOMes & Amphetamines
- 5.276 NBOMes & MDMA
- 5.277 NBOMes & Cocaine
- 5.278 NBOMes & Caffeine
- 5.279 NBOMes & Alcohol
- 5.280 NBOMes & GHB\GBL
- 5.281 NBOMes & Opioids
- 5.282 NBOMes & Tramadol
- 5.283 NBOMes & Benzodiazepines
- 5.284 NBOMes & MAOIs
- 5.285 NBOMes & SSRIs
- 5.286 2C-x & 2C-T-x
- 5.287 2C-x & αMT
- 5.288 2C-x & 5-MeO-xxT
- 5.289 2C-x & Cannabis
- 5.290 2C-x & Ketamine
- 5.291 2C-x & MXE
- 5.292 2C-x & DXM
- 5.293 2C-x & Nitrous
- 5.294 2C-x & Amphetamines
- 5.295 2C-x & MDMA
- 5.296 2C-x & Cocaine
- 5.297 2C-x & Caffeine
- 5.298 2C-x & Alcohol
- 5.299 2C-x & GHB\GBL
- 5.300 2C-x & Opioids
- 5.301 2C-x & Tramadol
- 5.302 2C-x & Benzodiazepines
- 5.303 2C-x & MAOIs
- 5.304 2C-x & SSRIs
- 5.305 2C-T-x & αMT
- 5.306 2C-T-x & 5-MeO-xxT
- 5.307 2C-T-x & Cannabis
- 5.308 2C-T-x & Ketamine
- 5.309 2C-T-x & MXE
- 5.310 2C-T-x & DXM
- 5.311 2C-T-x & Nitrous
- 5.312 2C-T-x & Amphetamines
- 5.313 2C-T-x & MDMA
- 5.314 2C-T-x & Cocaine
- 5.315 2C-T-x & Caffeine
- 5.316 2C-T-x & Alcohol
- 5.317 2C-T-x & GHB\GBL
- 5.318 2C-T-x & Opioids
- 5.319 2C-T-x & Tramadol
- 5.320 2C-T-x & Benzodiazepines
- 5.321 2C-T-x & MAOIs
- 5.322 2C-T-x & SSRIs
- 5.323 αMT & 5-MeO-xxT
- 5.324 αMT & Cannabis
- 5.325 αMT & Ketamine
- 5.326 αMT & MXE
- 5.327 αMT & DXM
- 5.328 αMT & Nitrous
- 5.329 αMT & Amphetamines
- 5.330 αMT & MDMA
- 5.331 αMT & Cocaine
- 5.332 αMT & Caffeine
- 5.333 αMT & Alcohol
- 5.334 αMT & GHB\GBL
- 5.335 αMT & Opioids
- 5.336 αMT & Tramadol
- 5.337 αMT & Benzodiazepines
- 5.338 αMT & MAOIs
- 5.339 αMT & SSRIs
- 5.340 5-MeO-xxT & Cannabis
- 5.341 5-MeO-xxT & Ketamine
- 5.342 5-MeO-xxT & MXE
- 5.343 5-MeO-xxT & DXM
- 5.344 5-MeO-xxT & Nitrous
- 5.345 5-MeO-xxT & Amphetamines
- 5.346 5-MeO-xxT & MDMA
- 5.347 5-MeO-xxT & Cocaine
- 5.348 5-MeO-xxT & Caffeine
- 5.349 5-MeO-xxT & Alcohol
- 5.350 5-MeO-xxT & GHB\GBL
- 5.351 5-MeO-xxT & Opioids
- 5.352 5-MeO-xxT & Tramadol
- 5.353 5-MeO-xxT & Benzodiazepines
- 5.354 5-MeO-xxT & MAOIs
- 5.355 5-MeO-xxT & SSRIs
- 5.356 Cannabis & Ketamine
- 5.357 Cannabis & MXE
- 5.358 Cannabis & DXM
- 5.359 Cannabis & Nitrous
- 5.360 Cannabis & Amphetamines
- 5.361 Cannabis & MDMA
- 5.362 Cannabis & Cocaine
- 5.363 Cannabis & Caffeine
- 5.364 Cannabis & Alcohol
- 5.365 Cannabis & GHB\GBL
- 5.366 Cannabis & Opioids
- 5.367 Cannabis & Tramadol
- 5.368 Cannabis & Benzodiazepines
- 5.369 Cannabis & MAOIs
- 5.370 Cannabis & SSRIs
- 5.371 Ketamine & MXE
- 5.372 Ketamine & DXM
- 5.373 Ketamine & Nitrous
- 5.374 Ketamine & Amphetamines
- 5.375 Ketamine & MDMA
- 5.376 Ketamine & Cocaine
- 5.377 Ketamine & Caffeine
- 5.378 Ketamine & Alcohol
- 5.379 Ketamine & GHB\GBL
- 5.380 Ketamine & Opioids
- 5.381 Ketamine & Tramadol
- 5.382 Ketamine & Benzodiazepines
- 5.383 Ketamine & MAOIs
- 5.384 Ketamine & SSRIs
- 5.385 MXE & DXM
- 5.386 MXE & Nitrous
- 5.387 MXE & Amphetamines
- 5.388 MXE & MDMA
- 5.389 MXE & Cocaine
- 5.390 MXE & Caffeine
- 5.391 MXE & Alcohol
- 5.392 MXE & GHB\GBL
- 5.393 MXE & Opioids
- 5.394 MXE & Tramadol
- 5.395 MXE & Benzodiazepines
- 5.396 MXE & MAOIs
- 5.397 MXE & SSRIs
- 5.398 DXM & Nitrous
- 5.399 DXM & Amphetamines
- 5.400 DXM & MDMA
- 5.401 DXM & Cocaine
- 5.402 DXM & Caffeine
- 5.403 DXM & Alcohol
- 5.404 DXM & GHB\GBL
- 5.405 DXM & Opioids
- 5.406 DXM & Tramadol
- 5.407 DXM & Benzodiazepines
- 5.408 DXM & MAOIs
- 5.409 DXM & SSRIs
- 5.410 Nitrous & Amphetamines
- 5.411 Nitrous & MDMA
- 5.412 Nitrous & Cocaine
- 5.413 Nitrous & Caffeine
- 5.414 Nitrous & Alcohol
- 5.415 Nitrous & GHB\GBL
- 5.416 Nitrous & Opioids
- 5.417 Nitrous & Tramadol
- 5.418 Nitrous & Benzodiazepines
- 5.419 Nitrous & MAOIs
- 5.420 Nitrous & SSRIs
- 5.421 Amphetamines & MDMA
- 5.422 Amphetamines & Cocaine
- 5.423 Amphetamines & Caffeine
- 5.424 Amphetamines & Alcohol
- 5.425 Amphetamines & GHB\GBL
- 5.426 Amphetamines & Opioids
- 5.427 Amphetamines & Tramadol
- 5.428 Amphetamines & Benzodiazepines
- 5.429 Amphetamines & MAOIs
- 5.430 Amphetamines & SSRIs
- 5.431 MDMA & Cocaine
- 5.432 MDMA & Caffeine
- 5.433 MDMA & Alcohol
- 5.434 MDMA & GHB\GBL
- 5.435 MDMA & Opioids
- 5.436 MDMA & Tramadol
- 5.437 MDMA & Benzodiazepines
- 5.438 MDMA & MAOIs
- 5.439 MDMA & SSRIs
- 5.440 Cocaine & Caffeine
- 5.441 Cocaine & Alcohol
- 5.442 Cocaine & GHB\GBL
- 5.443 Cocaine & Opioids
- 5.444 Cocaine & Tramadol
- 5.445 Cocaine & Benzodiazepines
- 5.446 Cocaine & MAOIs
- 5.447 Cocaine & SSRIs
- 5.448 Caffeine & Alcohol
- 5.449 Caffeine & GHB\GBL
- 5.450 Caffeine & Opioids
- 5.451 Caffeine & Tramadol
- 5.452 Caffeine & Benzodiazepines
- 5.453 Caffeine & MAOIs
- 5.454 Caffeine & SSRIs
- 5.455 Alcohol & GHB\GBL
- 5.456 Alcohol & Opioids
- 5.457 Alcohol & Tramadol
- 5.458 Alcohol & Benzodiazepines
- 5.459 Alcohol & MAOIs
- 5.460 Alcohol & SSRIs
- 5.461 GHB\GBL & Opioids
- 5.462 GHB\GBL & Tramadol
- 5.463 GHB\GBL & Benzodiazepines
- 5.464 GHB\GBL & MAOIs
- 5.465 GHB\GBL & SSRIs
- 5.466 Opioids & Tramadol
- 5.467 Opioids & Benzodiazepines
- 5.468 Opioids & MAOIs
- 5.469 Opioids & SSRIs
- 5.470 Tramadol & Benzodiazepines
- 5.471 Tramadol & MAOIs
- 5.472 Tramadol & SSRIs
- 5.473 Benzodiazepines & MAOIs
- 5.474 Benzodiazepines & SSRIs
- 5.475 MAOIs & SSRIs
This chart is meant as a quick reference guide and additional research MUST always be done. If you use this chart or information on your site you must link to the full summaries and display this message.
If you want to give us some feedback/recommendation/comment on the chart, you can contact us:
Join #content channel on IRC
We have a printed combo chart available here. We also offer a tool to generate a custom sized version of the chart that fits your need via a Github application which you can then take to your local printing place. If you chose to print your own we request that you please donate to help us cover running cost and develop new useful tools. Do note if you wish to edit the chart to your fitting please get in contact with us first via the email below. Printing and reselling the posters is not permitted without explicit written permission via email.
Email: [email protected] .

Categorisations
Low Risk & Synergy - These drugs work together to cause an effect greater than the sum of its parts, and they aren't likely to cause an adverse or undesirable reaction when used carefully. Additional research should always be done before combining drugs.
Low Risk & No Synergy - Effects are just additive. The combination is unlikely to cause any adverse or undesirable reaction beyond those that might ordinarily be expected from these drugs.
Caution - These combinations are not usually physically harmful, but may produce undesirable effects, such as physical discomfort or overstimulation. Extreme use may cause physical health issues. Synergistic effects may be unpredictable. Care should be taken when choosing to use this combination.
Unsafe - There is considerable risk of physical harm when taking these combinations, they should be avoided where possible.
Dangerous - These combinations are considered extremely harmful and should always be avoided. Reactions to these drugs taken in combination are highly unpredictable and have a potential to cause death.
Chart versions
Portuguese (Needs Translation)
Polish (Needs Translation)
Use & Attribution
Use of the data the combination chart and app are built upon is free-of-charge for non-commercial purposes. Distribution and display of the combination chart is also free for non-commercial purposes. In both cases, we only require that you link back to either this page, or [1] . This should be accompanied with a note citing TripSit as the source for the information wherever it appears. The presentation should also include a note that the information is only intended for a quick overview and reference, and that it is necessary for users to perform more individual research before making a decision.
Specific Combinations
Cannabis & lsd.
Status: Caution
Note: Cannabis has an unexpectedly strong and somewhat unpredictable synergy with psychedelics.
amphetamines & lsd
Note: Stimulants increase anxiety levels and the risk of thought loops which can lead to negative experiences
cocaine & lsd
Tramadol & lsd.
Status: Unsafe
Note: Tramadol is well known to lower seizure threshold and psychedelics also cause occasional seizures.
cannabis & mushrooms
Amphetamines & mushrooms, cocaine & mushrooms, tramadol & mushrooms, cannabis & dmt, amphetamines & dmt, cocaine & dmt, tramadol & dmt, 5-meo-xxt & mescaline.
Note: The 5-MeO class of tryptamines can be unpredictable in their interactions
cannabis & mescaline
Amphetamines & mescaline.
Note: The focus and anxiety caused by stimulants is magnified by psychedelics and results in an increased risk of thought loops
cocaine & mescaline
Caffeine & mescaline.
Status: Low Risk & No Synergy
Note: High doses of caffeine are uncomfortable and this will be magnified by psychedelics
tramadol & mescaline
Note: This combination can cause seizures due to the lowering of the threshold by tramadol and the potential of mescaline to cause seziures.
5-meo-xxt & dox
Note: The 5-MeO class of tryptamines can be unpredictable in their interactions, particularly increasing the risk of unpleasant physical side effects.
cannabis & dox
Ketamine & dox.
Status: Low Risk & Synergy
Note: Ketamine and psychedelics tend to potentiate each other - go slowly.
mxe & dox
Note: As an NMDA antagonist MXE potentiates DOx which can be unpleasantly intense
dxm & dox
Note: The DOx class as psychedelic stimulants have the potential to mask the effects of DXM and could lead to redosing to an unsafe level. DXM can also potentiate DOx resulting in an unpleasantly intense experience.
pcp & dox
Note: Details of this combination are not well understood but PCP generally interacts in an unpredictable manner.
amphetamines & dox
Note: The combined stimulating effects of the two can lead to an uncomfortable body-load, while the focusing effects of amphetamine can easily lead to thought loops. Coming down from amphetamines while the DOx is still active can be quite anxiogenic.
mdma & dox
Note: The combined stimulating effects of the two can be uncomfortable. Coming down on the MDMA while the DOx is still active can be quite anxiogenic.
cocaine & dox
Note: The combined stimulating effects of the two can lead to an uncomfortable body-load, while the focusing effects of cocaine can easily lead to thought loops. Coming down from cocaine while the DOx is still active can be quite anxiogenic
caffeine & dox
Note: High doses of caffeine may cause anxiety which is less manageable when tripping, and since both are stimulating it may cause some physical discomfort.
alcohol & dox
Status: Low Risk & Decrease
Note: Drinking on stimulants is risky because the sedative effects of the alcohol are reduced, and these are what the body uses to gauge drunkenness. This typically leads to excessive drinking with greatly reduced inhibitions, high risk of liver damage and increased dehydration. They will also allow you to drink past a point where you might normally pass out, increasing the risk.
opioids & dox
Note: No unexpected interactions.
tramadol & dox
Maois & dox.
Note: MAO-B inhibitors can increase the potency and duration of phenethylamines unpredictably
5-meo-xxt & nbomes
Note: The 5-MeO class of tryptamines can be unpredictable in their interactions and the NBOMes are known to be unpredictable even alone. This combination is best avoided
cannabis & nbomes
Mxe & nbomes.
Note: As an NMDA antagonist MXE potentiates NBOMes which can be unpleasantly intense
amphetamines & nbomes
Note: Amphetamines and NBOMes both provide considerable stimulation. When combined they can result in tachycardia, hypertension, vasoconstriction and in extreme cases heart failure. The anxiogenic and focusing effects of stimulants are also not good in combination with psychedelics as they can lead to unpleasant thought loops. NBOMes are known to cause seizures and stimulants can increase this risk.
cocaine & nbomes
Note: Cocaine and NBOMes both provide considerable stimulation. When combined they can result in severe vasoconstriction, tachycardia, hypertension, and in extreme cases heart failure.
caffeine & nbomes
Note: Caffiene can bring out the natural stimulation from psychedelic drugs to make it uncomfortable. High doses can cause anxiety which is hard to handle while tripping
tramadol & nbomes
Note: Tramadol is well known to lower seizure threshold and NBOMes have also shown a tendency to cause severe seizures
maois & nbomes
5-meo-xxt & 2c-x.
Note: The 5-MeO psychedelics can interact unpredictably to potentiate other psychedelics
cannabis & 2c-x
Amphetamines & 2c-x.
Note: The anxiogenic and focusing effects of stimulants increase the chance of unpleasant thought loops. The combination is generally uneccessary because of the stimulating effects of psychedelics. Combination of the stimulating effects may be uncomfortable.
cocaine & 2c-x
Note: The anxiogenic and focusing effects of stimulants increase the chance of unpleasant thought loops. The combination is generally unnecessary because of the stimulating effects of psychedelics. Combination of the stimulating effects may be uncomfortable.
caffeine & 2c-x
Note: High doses of caffeine may cause anxiety which is less manageable when tripping, and since both are stimulating the combination may cause some physical discomfort.
tramadol & 2c-x
Note: Tramadol is well known to lower seizure threshold and psychedelics raise the risk of seizures.
maois & 2c-x
5-meo-xxt & 2c-t-x.
Note: Both classes of compounds can be unpredictable alone
cannabis & 2c-t-x
Amphetamines & 2c-t-x.
Note: Stimulants increase anxiety levels and the risk of thought loops which can lead to negative experiences. In extreme cases, they can result in severe vasoconstriction, tachycardia, hypertension, and in extreme cases heart failure.
cocaine & 2c-t-x
Note: Cocaine and 2c-t-x both provide considerable stimulation. When combined they can result in severe vasoconstriction, tachycardia, hypertension, and in extreme cases heart failure.
caffeine & 2c-t-x
Alcohol & 2c-t-x.
Note: Both these classes of compound can interact unpredictably. Caution should be exercised.
opioids & 2c-t-x
Note: No expected interactions, some opioids have serotonin action, and could lead to Serotonin Syndrome or a seizure. These are pretty much only to Pentazocine, Methadone, Tramadol, Tapenatdol.
maois & 2c-t-x
Note: MAO-B inhibitors can increase the potency and duration of phenethylamines unpredictably, which could be dangerous given the unpredictability of the 2C-T-x series
cannabis & amt
Note: Cannabis has an unexpectedly strong and somewhat unpredictable synergy with psychedelics. Small amounts can reduce nausea with aMT but take care.
caffeine & amt
Alcohol & amt.
Note: aMT has a broad mechanism of action in the brain and so does alcohol so the combination can be unpredictable
opioids & amt
Note: No unexpected interactions
maois & amt
Status: Dangerous
Note: aMT is an MAOI on its own. Using enzyme inhibitors can greatly reduce predictability of effects.
mxe & 5-meo-xxt
Note: Little information exists about this combination.
dxm & 5-meo-xxt
Cannabis & 5-meo-xxt, amphetamines & 5-meo-xxt.
Note: The anxiogenic and focusing effects of stimulants increase the chance of unpleasant thought loops. The combination is generally unnecessary because of the stimulating effects of psychedelics.
mdma & 5-meo-xxt
Note: Some of the 5-MeO tryptamines are a bit unpredictable and should be mixed with MDMA with care
cocaine & 5-meo-xxt
Caffeine & 5-meo-xxt, amphetamines & cannabis, mdma & cannabis.
Note: Large amounts of either or both may cause strong and somewhat unpredictable experiences, which can be as intense as psychedelics. Consider rather Set and Setting are good, before you combine these. Cannabis should be saved for towards the end of the MDMA experience if possible, where the psychedelic alike effect won't come to play.
cocaine & cannabis
Alcohol & cannabis.
Note: In excess, this combination can cause nausea.
amphetamines & ketamine
Note: No unexpected interactions, though likely to increase blood pressure but not an issue with sensible doses. Moving around on high doses of this combination may be ill advised due to risk of physical injury.
mdma & ketamine
Cocaine & ketamine, caffeine & ketamine, alcohol & ketamine.
Note: Both substances cause ataxia and bring a very high risk of vomiting and unconsciousness. If the user falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position.
ghb/gbl & ketamine
Note: Both substances cause ataxia and bring a risk of vomiting and unconsciousness. If the user falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position.
opioids & ketamine
Note: Both substances bring a risk of vomiting and unconsciousness. If the user falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position.
benzodiazepines & ketamine
Note: Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. While unconscious, vomit aspiration is a risk if not placed in the recovery position.
maois & ketamine
Note: MAO-B inhibitors appear to increase the potency of Ketamine. MAO-A inhbitors have some negative reports associated with the combination but there isn't much information available
pcp & mxe
Note: There are no reports available about this combination
amphetamines & mxe
Note: Risk of tachycardia, hypertension, and manic states
mdma & mxe
Note: There have been reports of risky serotonergic interactions when the two are taken at the same time, but MXE taken to the end of an MDMA experience does not appear to cause the same issues.
cocaine & mxe
Note: Stimulants taken with MXE can lead to hypermanic states much more easily, especially if sleep is avoided.
caffeine & mxe
Note: No likely interactions
alcohol & mxe
Note: There is a high risk of memory loss, vomiting and severe ataxia from this combination.
ghb/gbl & mxe
Note: Both substances cause ataxia and bring a risk of vomiting and unconsciousness. If the patient falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position.
opioids & mxe
Note: This combination can potentiate the effects of the opioid
benzodiazepines & mxe
Note: Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. Place affected patients in the recovery position to prevent vomit aspiration from excess.
maois & mxe
Note: MAO-B inhibitors appear to increase the potency of MXE. MAO-A inhbitors have some negative reports associated with the combination but there isn't much information available
ssris & mxe
Note: Depending on the SSRI this combination can be unpredictable
amphetamines & dxm
Note: Both substances raise heart rate, in extreme cases, panic attacks caused by these drugs have led to more serious heart issues.
cocaine & dxm
Note: Both substances raise heart rate, in extreme cases, panic attacks caused by these drugs have led to more serious heart issues
caffeine & dxm
Alcohol & dxm.
Note: Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. Place affected patients in the recovery position to prevent vomit aspiration from excess. Additionally CNS depression can lead to difficulty breathing. Avoid on anything higher than 1st plateau.
ghb/gbl & dxm
Note: Both substances cause ataxia and bring a risk of vomiting and unconsciousness. If the patient falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position. This combination is hard to predict
opioids & dxm
Note: CNS depression, difficult breathing, heart issues, hepatoxic, just very unsafe combination all around. Additionally if one takes dxm, their tolerance of opiates goes down slightly, thus causing additional synergistic effects.
benzodiazepines & dxm
Note: Small doses of benzos can end a bad trip, but both substances potentiate the ataxia and sedation caused by the other and this can lead to unexpected loss of consciousness at high doses. While unconscious, vomit aspiration is a risk if not placed in the recovery position.
maois & dxm
Note: High risk of serotonin syndrome
ssris & dxm
Note: High risk of serotonin syndrome.
amphetamines & pcp
Note: This combination can easily lead to hypermanic states
mdma & pcp
Cocaine & pcp, caffeine & pcp, alcohol & pcp, ghb/gbl & pcp, opioids & pcp.
Note: PCP can reduce opioid tolerance, increasing the risk of overdose
benzodiazepines & pcp
Note: Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. While unconscious, vomit aspiration is a risk if not placed in the recovery position. Memory blackouts are likely
maois & pcp
Note: This combination is very poorly explored
ssris & pcp
Alcohol & nitrous.
Note: Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. While unconscious, vomit aspiration is a risk if not placed in the recovery position. Memory blackouts are likely.
ghb/gbl & nitrous
Opioids & nitrous, tramadol & nitrous, mdma & amphetamines.
Note: Amphetamines increase the neurotoxic effects of MDMA
cocaine & amphetamines
Note: This combination of stimulants will increase strain on the heart. It is not generally worth it as cocaine has a mild blocking effect on dopamine releasers like amphetamine
caffeine & amphetamines
Note: This combination of stimulants is not generally necessary and may increase strain on the heart, as well as potentially causing anxiety and greater physical discomfort.
alcohol & amphetamines
Note: Drinking on stimulants is risky because the sedative effects of the alcohol are reduced, and these are what the body uses to gauge drunkenness. This typically leads to excessive drinking with greatly reduced inhibitions, high risk of liver damage and increased dehydration. They will also allow you to drink past a point where you might normally pass out, increasing the risk. If you do decide to do this then you should set a limit of how much you will drink each hour and stick to it, bearing in mind that you will feel the alcohol and the stimulant less. Extended release formulations may severely impede sleep, further worsening the hangover.
ghb/gbl & amphetamines
Note: Stimulants increase respiration rate allowing a higher dose of sedatives. If the stimulant wears off first then the opiate may overcome the patient and cause respiratory arrest.
opioids & amphetamines
Note: Stimulants increase respiration rate allowing a higher dose of opiates. If the stimulant wears off first then the opiate may overcome the patient and cause respiratory arrest.
tramadol & amphetamines
Note: Tramadol and stimulants both increase the risk of seizures.
benzodiazepines & amphetamines
Note: Both can dull each other's effects, so if one wears off before the other it's possible to overdose due to the lack of counteraction
maois & amphetamines
Note: MAO-B inhibitors can increase the potency and duration of phenethylamines unpredictably. MAO-A inhibitors with amphetamine can lead to hypertensive crises.
cocaine & mdma
Note: Cocaine blocks some of the desirable effects of MDMA while increasing the risk of heart attack.
caffeine & mdma
Note: Caffiene is not really necessary with MDMA and increases any neurotoxic effects from MDMA
alcohol & mdma
Note: Both MDMA and alcohol cause dehydration. Approach this combination with caution, moderation and sufficient hydration. More than a small amount of alcohol will dull the euphoria of MDMA
ghb/gbl & mdma
Note: Large amounts of GHB/GBL may overwhelm the effects of MDMA on the comedown.
tramadol & mdma
Maois & mdma.
Note: MAO-B inhibitors can increase the potency and duration of phenethylamines unpredictably. MAO-A inhibitors with MDMA will lead to hypertensive crises.
caffeine & cocaine
Note: Both stimulants, risk of tachycardia, hypertension, and in extreme cases heart failure.
alcohol & cocaine
Note: Drinking on stimulants is risky because the sedative effects of the alcohol are reduced, and these are what the body uses to gauge drunkenness. This typically leads to excessive drinking with greatly reduced inhibitions, high risk of liver damage and increased dehydration. They will also allow you to drink past a point where you might normally pass out, increasing the risk. If you do decide to do this then you should set a limit of how much you will drink each hour and stick to it, bearing in mind that you will feel the alcohol less. Cocaine is potentiated somewhat by alcohol because of the formation of cocaethylene.
ghb/gbl & cocaine
Note: Stimulants increase respiration rate allowing a higher dose of sedatives. If the stimulant wears off first then the opiate may overcome the patient and cause respiratory arrest. Likewise the G can wear off and leave a dangerous concentration of cocaine behind
opioids & cocaine
Tramadol & cocaine, maois & cocaine.
Note: This combination is poorly explored
ssris & cocaine
Note: May reduce each others' effectiveness. Cocaine can reduce mental stability and therefore exacerbate conditions which SSRIs are used to treat.
ghb/gbl & alcohol
Note: Even in very low doses this combination rapidly leads to memory loss, severe ataxia and unconsciousness. There is a high risk of vomit aspiration while unconscious.
opioids & alcohol
Note: Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. Place affected patients in the recovery position to prevent vomit aspiration from excess. Memory blackouts are likely
tramadol & alcohol
Note: Heavy CNS depressants, risk of seizures. Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. Place affected patients in the recovery position to prevent vomit aspiration from excess. Memory blackouts are likely.
benzodiazepines & alcohol
Note: Ethanol ingestion may potentiate the CNS effects of many benzodiazepines. The two substances potentiate each other strongly and unpredictably, very rapidly leading to unconsciousness. While unconscious, vomit aspiration is a risk if not placed in the recovery position. Blacking out and memory loss is almost certain.
maois & alcohol
Note: Tyramine found in many alcoholic beverages can have dangerous reactions with MAOIs, causing an increase in blood pressure.
ssris & alcohol
Note: Alcohol may potentiate some of the pharmacologic effects of CNS-active agents. Use in combination may result in additive central nervous system depression and/or impairment of judgment, thinking, and psychomotor skills.
opioids & ghb/gbl
Note: The two substances potentiate each other strongly and unpredictably, very rapidly leading to unconsciousness. While unconscious, vomit aspiration is a risk if not placed in the recovery position
tramadol & ghb/gbl
Note: The sedative effects of this combination can lead to dangerous respiratory depression.
benzodiazepines & ghb/gbl
Note: The two substances potentiate each other strongly and unpredictably, very rapidly leading to unconsciousness. While unconscious, vomit aspiration is a risk if not placed in the recovery position.
tramadol & opioids
Note: Concomitant use of tramadol increases the seizure risk in patients taking other opioids. These agents are often individually epileptogenic and may have additive effects on seizure threshold during coadministration. Central nervous system- and/or respiratory-depressant effects may be additively or synergistically present
benzodiazepines & opioids
Note: Central nervous system and/or respiratory-depressant effects may be additively or synergistically present. The two substances potentiate each other strongly and unpredictably, very rapidly leading to unconsciousness. While unconscious, vomit aspiration is a risk if not placed in the recovery position Blackouts/memory loss likely
maois & opioids
Note: Coadministration of monoamine oxidase inhibitors (MAOIs) with certain opioids has been associated with rare reports of severe and fatal adverse reactions. There appear to be two types of interaction, an excitatory and a depressive one. Symptoms of the excitatory reaction may include agitation, headache, diaphoresis, hyperpyrexia, flushing, shivering, myoclonus, rigidity, tremor, diarrhea, hypertension, tachycardia, seizures, and coma. Death has occurred in some cases.
ssris & opioids
Note: There have been very infrequent reports of a risk of serotonin syndrome with this combination, though this should not be a practical concern.
benzodiazepines & tramadol
Note: Central nervous system- and/or respiratory-depressant effects may be additively or synergistically present. Vomit aspiration a risk when passed out, lay down in recovery position if ingested.
LSD & Mushrooms
Lsd & dmt.
- http://www.ncbi.nlm.nih.gov/pubmed/3006089
- http://deepblue.lib.umich.edu/bitstream/handle/2027.42/26285/0000370.pdf
LSD & Mescaline
Lsd & dox, lsd & nbomes, lsd & 2c-x, lsd & 2c-t-x, lsd & αmt, lsd & 5-meo-xxt, lsd & cannabis, lsd & ketamine, lsd & mxe, lsd & dxm, lsd & nitrous, lsd & amphetamines, lsd & mdma, lsd & cocaine, lsd & caffeine, lsd & alcohol, lsd & ghb\gbl.
- http://www.ncbi.nlm.nih.gov/pubmed/16483730
LSD & Opioids
- http://www.ncbi.nlm.nih.gov/pubmed/547279
- "Low doses antagonized the effects of both hallucinogens, whereas larger doses enhanced their effects."
LSD & Tramadol
Lsd & benzodiazepines, lsd & maois.
- http://www.ncbi.nlm.nih.gov/pubmed/8788508
- http://www.ncbi.nlm.nih.gov/pubmed/108709
- https://www.erowid.org/references/refs_view.php?A=ShowDocPartFrame&ID=2439&DocPartID=2199
LSD & SSRIs
- http://www.nature.com/npp/journal/v14/n6/full/1380431a.html
- http://www.ncbi.nlm.nih.gov/pubmed/8726753
Mushrooms & DMT
Mushrooms & mescaline, mushrooms & dox, mushrooms & nbomes, mushrooms & 2c-x, mushrooms & 2c-t-x, mushrooms & αmt, mushrooms & 5-meo-xxt, mushrooms & cannabis, mushrooms & ketamine, mushrooms & mxe, mushrooms & dxm, mushrooms & nitrous, mushrooms & amphetamines, mushrooms & mdma, mushrooms & cocaine, mushrooms & caffeine, mushrooms & alcohol, mushrooms & ghb\gbl, mushrooms & opioids, mushrooms & tramadol, mushrooms & benzodiazepines, mushrooms & maois, mushrooms & ssris, dmt & mescaline, dmt & dox, dmt & nbomes, dmt & 2c-x, dmt & 2c-t-x, dmt & αmt, dmt & 5-meo-xxt, dmt & cannabis, dmt & ketamine, dmt & mxe, dmt & dxm, dmt & nitrous, dmt & amphetamines, dmt & mdma, dmt & cocaine, dmt & caffeine, dmt & alcohol, dmt & ghb\gbl, dmt & opioids, dmt & tramadol, dmt & benzodiazepines, dmt & maois, dmt & ssris, mescaline & dox, mescaline & nbomes, mescaline & 2c-x, mescaline & 2c-t-x, mescaline & αmt, mescaline & 5-meo-xxt.
- The 5-MeO class of tryptamines can be unpredictable in their interactions.
Mescaline & Cannabis
Mescaline & ketamine, mescaline & mxe, mescaline & dxm, mescaline & nitrous, mescaline & amphetamines.
- The focus and anxiety caused by stimulants is magnified by psychedelics and results in an increased risk of thought loops.
Mescaline & MDMA
Mescaline & cocaine, mescaline & caffeine.
- High doses of caffeine are uncomfortable and this will be magnified by psychedelics.
Mescaline & Alcohol
Mescaline & ghb\gbl, mescaline & opioids, mescaline & tramadol.
- This combination can cause seizures due to the lowering of the threshold by tramadol and the potential of mescaline to cause seziures.
Mescaline & Benzodiazepines
Mescaline & maois, mescaline & ssris, dox & nbomes, dox & 2c-x, dox & 2c-t-x, dox & αmt, dox & 5-meo-xxt.
- The 5-MeO class of tryptamines can be unpredictable in their interactions, particularly increasing the risk of unpleasant physical side effects.
DOx & Cannabis
Dox & ketamine.
- Ketamine and psychedelics tend to potentiate each other - go slowly.
DOx & MXE
- As an NMDA antagonist MXE potentiates DOx which can be unpleasantly intense.
DOx & DXM
- The DOx class as psychedelic stimulants have the potential to mask the effects of DXM and could lead to redosing to an unsafe level. DXM can also potentiate DOx resulting in an unpleasantly intense experience.
DOx & Nitrous
Dox & amphetamines.
- The combined stimulating effects of the two can lead to an uncomfortable body-load, while the focusing effects of amphetamine can easily lead to thought loops. Coming down from amphetamines while the DOx is still active can be quite anxiogenic.
- http://www.ncbi.nlm.nih.gov/pubmed/1208759
DOx & MDMA
- The combined stimulating effects of the two can be uncomfortable. Coming down on the MDMA while the DOx is still active can be quite anxiogenic.
DOx & Cocaine
- The combined stimulating effects of the two can lead to an uncomfortable body-load, while the focusing effects of cocaine can easily lead to thought loops. Coming down from cocaine while the DOx is still active can be quite anxiogenic.
DOx & Caffeine
- High doses of caffeine may cause anxiety which is less manageable when tripping, and since both are stimulating it may cause some physical discomfort.
DOx & Alcohol
- Drinking on stimulants is risky because the sedative effects of the alcohol are reduced, and these are what the body uses to gauge drunkenness. This typically leads to excessive drinking with greatly reduced inhibitions, high risk of liver damage and increased dehydration. They will also allow you to drink past a point where you might normally pass out, increasing the risk.
DOx & GHB\GBL
Dox & opioids.
- No unexpected interactions.
DOx & Tramadol
- Tramadol is well known to lower seizure threshold and psychedelics also cause occasional seizures.
DOx & Benzodiazepines
Dox & maois, dox & ssris, nbomes & 2c-x, nbomes & 2c-t-x, nbomes & αmt, nbomes & 5-meo-xxt.
- The 5-MeO class of tryptamines can be unpredictable in their interactions and the NBOMes are known to be unpredictable even alone. This combination is best avoided.
NBOMes & Cannabis
Nbomes & ketamine, nbomes & mxe, nbomes & dxm, nbomes & nitrous, nbomes & amphetamines.
- Amphetamines and NBOMes both provide considerable stimulation. When combined they can result in tachycardia, hypertension, vasoconstriction and in extreme cases heart failure. The anxiogenic and focusing effects of stimulants are also not good in combination with psychedelics as they can lead to unpleasant thought loops. NBOMes are known to cause seizures and stimulants can increase this risk.
NBOMes & MDMA
Nbomes & cocaine.
- Cocaine and NBOMes both provide considerable stimulation. When combined they can result in severe vasoconstriction, tachycardia, hypertension, and in extreme cases heart failure.
NBOMes & Caffeine
- Caffiene can bring out the natural stimulation from psychedelic drugs to make it uncomfortable. High doses can cause anxiety which is hard to handle while tripping.
NBOMes & Alcohol
Nbomes & ghb\gbl, nbomes & opioids, nbomes & tramadol.
- Tramadol is well known to lower seizure threshold and NBOMes have also shown a tendency to cause severe seizures.
NBOMes & Benzodiazepines
Nbomes & maois, nbomes & ssris, 2c-x & 2c-t-x, 2c-x & αmt, 2c-x & 5-meo-xxt.
- The 5-MeO psychedelics can interact unpredictably to potentiate other psychedelics.
2C-x & Cannabis
2c-x & ketamine, 2c-x & mxe, 2c-x & dxm, 2c-x & nitrous, 2c-x & amphetamines.
- The anxiogenic and focusing effects of stimulants increase the chance of unpleasant thought loops. The combination is generally uneccessary because of the stimulating effects of psychedelics. Combination of the stimulating effects may be uncomfortable.
2C-x & MDMA
2c-x & cocaine.
- The anxiogenic and focusing effects of stimulants increase the chance of unpleasant thought loops. The combination is generally unnecessary because of the stimulating effects of psychedelics. Combination of the stimulating effects may be uncomfortable.
2C-x & Caffeine
- High doses of caffeine may cause anxiety which is less manageable when tripping, and since both are stimulating the combination may cause some physical discomfort.
2C-x & Alcohol
2c-x & ghb\gbl, 2c-x & opioids, 2c-x & tramadol.
- Tramadol is well known to lower seizure threshold and psychedelics raise the risk of seizures.
2C-x & Benzodiazepines
2c-x & maois, 2c-x & ssris, 2c-t-x & αmt, 2c-t-x & 5-meo-xxt, 2c-t-x & cannabis, 2c-t-x & ketamine, 2c-t-x & mxe, 2c-t-x & dxm, 2c-t-x & nitrous, 2c-t-x & amphetamines, 2c-t-x & mdma, 2c-t-x & cocaine, 2c-t-x & caffeine, 2c-t-x & alcohol.
- Both these classes of compound can interact unpredictably. Caution should be exercised.
2C-T-x & GHB\GBL
2c-t-x & opioids.
- No expected interactions, some Opioids have Serotonin action, and could lead to Serotonin Syndrome or a seizure. These are pretty much only to Pentazocine, Methadone, Tramadol, Tapenatdol.
2C-T-x & Tramadol
2c-t-x & benzodiazepines, 2c-t-x & maois, 2c-t-x & ssris, αmt & 5-meo-xxt, αmt & cannabis, αmt & ketamine, αmt & mxe, αmt & dxm, αmt & nitrous, αmt & amphetamines, αmt & mdma, αmt & cocaine, αmt & caffeine, αmt & alcohol.
- αMT has a broad mechanism of action in the brain and so does alcohol so the combination can be unpredictable.
αMT & GHB\GBL
Αmt & opioids.
- No unexpected interactions
αMT & Tramadol
Αmt & benzodiazepines, αmt & maois, αmt & ssris, 5-meo-xxt & cannabis, 5-meo-xxt & ketamine, 5-meo-xxt & mxe, 5-meo-xxt & dxm, 5-meo-xxt & nitrous, 5-meo-xxt & amphetamines.
- The anxiogenic and focusing effects of stimulants increase the chance of unpleasant thought loops. The combination is generally unnecessary because of the stimulating effects of psychedelics.
5-MeO-xxT & MDMA
- Some of the 5-MeO tryptamines are a bit unpredictable and should be mixed with MDMA with care.
5-MeO-xxT & Cocaine
5-meo-xxt & caffeine, 5-meo-xxt & alcohol, 5-meo-xxt & ghb\gbl, 5-meo-xxt & opioids, 5-meo-xxt & tramadol, 5-meo-xxt & benzodiazepines, 5-meo-xxt & maois, 5-meo-xxt & ssris, cannabis & ketamine, cannabis & mxe, cannabis & dxm, cannabis & nitrous, cannabis & amphetamines, cannabis & mdma, cannabis & cocaine, cannabis & caffeine, cannabis & alcohol, cannabis & ghb\gbl, cannabis & opioids, cannabis & tramadol, cannabis & benzodiazepines, cannabis & maois, cannabis & ssris, ketamine & mxe, ketamine & dxm, ketamine & nitrous, ketamine & amphetamines.
- Amphetamine worsens Ketamines ataxia.
- http://www.ncbi.nlm.nih.gov/pubmed/23660488
Ketamine & MDMA
Ketamine & cocaine, ketamine & caffeine.
- http://onlinelibrary.wiley.com/doi/10.1111/j.1742-7843.2009.00382.x/full
Ketamine & Alcohol
- Both substances cause ataxia and bring a very high risk of vomiting and unconsciousness. If the user falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position.
- http://onlinelibrary.wiley.com/doi/10.1002/jemt.22045/abstract
Ketamine & GHB\GBL
- Both substances cause ataxia and bring a risk of vomiting and unconsciousness. If the user falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position.
Ketamine & Opioids
- Both substances bring a risk of vomiting and unconsciousness. If the user falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position.
- http://www.ncbi.nlm.nih.gov/pubmed/21224020
Ketamine & Tramadol
Ketamine & benzodiazepines.
- Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. While unconscious, vomit aspiration is a risk if not placed in the recovery position.
Ketamine & MAOIs
Ketamine & ssris, mxe & dxm.
- http://i.imgur.com/zmqaw.jpg
- http://www.sciencedirect.com/science/article/pii/S0014488607002543
MXE & Nitrous
Mxe & amphetamines.
- Risk of tachycardia, hypertension, and manic states.
- http://www.ncbi.nlm.nih.gov/pubmed/25060403
MXE & MDMA
- There have been reports of risky serotonergic interactions when the two are taken at the same time, but MXE taken to the end of an MDMA experience does not appear to cause the same issues.
MXE & Cocaine
- Stimulants taken with MXE can lead to hypermanic states much more easily, especially if sleep is avoided.
MXE & Caffeine
- No likely interactions.
MXE & Alcohol
- There is a high risk of memory loss, vomiting and severe ataxia from this combination.
MXE & GHB\GBL
- Both substances cause ataxia and bring a risk of vomiting and unconsciousness. If the patient falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position.
MXE & Opioids
- This combination can potentiate the effects of the opioid.
MXE & Tramadol
Mxe & benzodiazepines.
- Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. Place affected patients in the recovery position to prevent vomit aspiration from excess.
MXE & MAOIs
Mxe & ssris.
- Depending on the SSRI this combination can be unpredictable.
DXM & Nitrous
Dxm & amphetamines.
- Both substances raise heart rate, in extreme cases, panic attacks caused by these drugs have led to more serious heart issues.
DXM & MDMA
Dxm & cocaine, dxm & caffeine, dxm & alcohol.
- Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. Place affected patients in the recovery position to prevent vomit aspiration from excess. Additionally CNS depression can lead to difficulty breathing. Avoid on anything higher than 1st plateau.
DXM & GHB\GBL
- Both substances cause ataxia and bring a risk of vomiting and unconsciousness. If the patient falls unconscious while under the influence there is a severe risk of vomit aspiration if they are not placed in the recovery position. This combination is hard to predict.
DXM & Opioids
- CNS depression, difficult breathing, heart issues, hepatoxic, just very unsafe combination all around. Additionally, there is a reverse cross tolerance between opiates/dxm. I.E. if one takes dxm, their tolerance of opiates goes down slightly, thus causing additional synergistic effects.
DXM & Tramadol
Dxm & benzodiazepines.
- Small doses of benzos can end a bad trip, but both substances potentiate the ataxia and sedation caused by the other and this can lead to unexpected loss of consciousness at high doses. While unconscious, vomit aspiration is a risk if not placed in the recovery position.
DXM & MAOIs
- High risk of serotonin syndrome.
DXM & SSRIs
Nitrous & amphetamines, nitrous & mdma, nitrous & cocaine, nitrous & caffeine, nitrous & alcohol.
- This combination can lead to vomiting.
Nitrous & GHB\GBL
Nitrous & opioids, nitrous & tramadol, nitrous & benzodiazepines, nitrous & maois, nitrous & ssris, amphetamines & mdma.
- Amphetamines increase the neurotoxic effects of MDMA.
Amphetamines & Cocaine
- This combination of stimulants will increase strain on the heart. It is not generally worth it as cocaine has a mild blocking effect on dopamine releasers like amphetamine.
Amphetamines & Caffeine
- This combination of stimulants is not generally necessary and may increase strain on the heart, as well as potentially causing anxiety and greater physical discomfort.
Amphetamines & Alcohol
- Drinking on stimulants is risky because the sedative effects of the alcohol are reduced, and these are what the body uses to gauge drunkenness. This typically leads to excessive drinking with greatly reduced inhibitions, high risk of liver damage and increased dehydration. They will also allow you to drink past a point where you might normally pass out, increasing the risk. If you do decide to do this then you should set a limit of how much you will drink each hour and stick to it, bearing in mind that you will feel the alcohol and the stimulant less. Extended release formulations may severely impede sleep, further worsening the hangover.
Amphetamines & GHB\GBL
- Stimulants increase respiration rate allowing a higher dose of sedatives. If the stimulant wears off first then the opiate may overcome the patient and cause respiratory arrest.
Amphetamines & Opioids
- Stimulants increase respiration rate allowing a higher dose of opiates. If the stimulant wears off first then the opiate may overcome the patient and cause respiratory arrest.
Amphetamines & Tramadol
- Tramadol and stimulants both increase the risk of seizures.
Amphetamines & Benzodiazepines
- http://www.ncbi.nlm.nih.gov/pubmed/17320309
Amphetamines & MAOIs
Amphetamines & ssris, mdma & cocaine.
- Cocaine blocks some of the desirable effects of MDMA while increasing the risk of heart attack.
MDMA & Caffeine
- Caffiene is not really necessary with MDMA and increases any neurotoxic effects from MDMA.
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3492978/
- http://link.springer.com/article/10.1007/s00213-010-1864-1
- http://www.sciencedirect.com/science/article/pii/S0028390805003114
- http://www.ncbi.nlm.nih.gov/pubmed/24211539
MDMA & Alcohol
- Both MDMA and alcohol cause severe dehydration. Approach this combination with caution, moderation and sufficient hydration.
- http://www.ncbi.nlm.nih.gov/pubmed/21040238
- http://www.ncbi.nlm.nih.gov/pubmed/21756931
MDMA & GHB\GBL
- http://www.ncbi.nlm.nih.gov/pubmed/16234132
- http://www.ncbi.nlm.nih.gov/pubmed/22554869
- http://www.ncbi.nlm.nih.gov/pubmed/20730418
MDMA & Opioids
Mdma & tramadol, mdma & benzodiazepines, mdma & maois, mdma & ssris, cocaine & caffeine.
- Both stimulants, risk of tachycardia, hypertension, and in extreme cases heart failure.
Cocaine & Alcohol
- Drinking on stimulants is risky because the sedative effects of the alcohol are reduced, and these are what the body uses to gauge drunkenness. This typically leads to excessive drinking with greatly reduced inhibitions, high risk of liver damage and increased dehydration. They will also allow you to drink past a point where you might normally pass out, increasing the risk. If you do decide to do this then you should set a limit of how much you will drink each hour and stick to it, bearing in mind that you will feel he alcohol less. Cocaine is potentiated somewhat by alcohol by reduction of cocaine breakdown which results in increased risk to the heart.
Cocaine & GHB\GBL
- Stimulants increase respiration rate allowing a higher dose of sedatives. If the stimulant wears off first then the opiate may overcome the patient and cause respiratory arrest. Likewise the G can wear off and leave a dangerous concentration of cocaine behind.
Cocaine & Opioids
Cocaine & tramadol, cocaine & benzodiazepines, cocaine & maois, cocaine & ssris.
- Risk of serotonin syndrome, Likely to make the SSRI's innefective with regular cocaine use. The SSRIs may also make the cocaine less effective. Mental stability and cocaine don't go together.
- http://www.ncbi.nlm.nih.gov/pubmed/23761390
- http://www.ncbi.nlm.nih.gov/pubmed/20195220
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3377381
Caffeine & Alcohol
- http://www.ncbi.nlm.nih.gov/pubmed/20001110
Caffeine & GHB\GBL
Caffeine & opioids, caffeine & tramadol.
- http://www.ncbi.nlm.nih.gov/pubmed/20837047
Caffeine & Benzodiazepines
Caffeine & maois, caffeine & ssris.
- http://journals.lww.com/jpharmacogenetics/abstract/1996/06000/a_fluvoxamine_caffeine_interaction_study.3.aspx
Alcohol & GHB\GBL
- Even in very low doses this combination rapidly leads to memory loss, severe ataxia and unconsciousness. There is a high risk of vomit aspiration while unconscious.
- http://www.ncbi.nlm.nih.gov/pubmed/15274975
Alcohol & Opioids
- Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. Place affected patients in the recovery position to prevent vomit aspiration from excess. Memory blackouts are likely.
Alcohol & Tramadol
- Heavy CNS depressants, risk of seizures. Both substances potentiate the ataxia and sedation caused by the other and can lead to unexpected loss of consciousness at high doses. Place affected patients in the recovery position to prevent vomit aspiration from excess. Memory blackouts are likely.
Alcohol & Benzodiazepines
- Ethanol ingestion may potentiate the CNS effects of many benzodiazepines. The two substances potentiate each other strongly and unpredictably, very rapidly leading to unconsciousness. While unconscious, vomit aspiration is a risk if not placed in the recovery position. Blacking out and memory loss is almost certain.
Alcohol & MAOIs
- The chemical tyramine in alcoholic beverages can have dangerous reactions with MAOIs, causing an increase in blood pressure.
Alcohol & SSRIs
- Alcohol may potentiate some of the pharmacologic effects of CNS-active agents. Use in combination may result in additive central nervous system depression and/or impairment of judgment, thinking, and psychomotor skills.
- http://www.ncbi.nlm.nih.gov/pubmed/15739105
GHB\GBL & Opioids
- The two substances potentiate each other strongly and unpredictably, very rapidly leading to unconsciousness. While unconscious, vomit aspiration is a risk if not placed in the recovery position.
- http://www.ncbi.nlm.nih.gov/pubmed/7782758
GHB\GBL & Tramadol
- The sedative effects of this combination can lead to dangerous respiratory depression.
GHB\GBL & Benzodiazepines
Ghb\gbl & maois.
- No study, but MAO B inhibitors should enhance the effects, no interaction with MAO A.
GHB\GBL & SSRIs
Opioids & tramadol.
- Concomitant use of tramadol increases the seizure risk in patients taking other opioids. These agents are often individually epileptogenic and may have additive effects on seizure threshold during coadministration. Central nervous system- and/or respiratory-depressant effects may be additively or synergistically present.
Opioids & Benzodiazepines
- Central nervous system and/or respiratory-depressant effects may be additively or synergistically present. The two substances potentiate each other strongly and unpredictably, very rapidly leading to unconsciousness. While unconscious, vomit aspiration is a risk if not placed in the recovery position Blackouts/memory loss likely.
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3454351/
Opioids & MAOIs
- Coadministration of monoamine oxidase inhibitors (MAOIs) with certain opioids has been associated with rare reports of severe and fatal adverse reactions. There appear to be two types of interaction, an excitatory and a depressive one. Symptoms of the excitatory reaction may include agitation, headache, diaphoresis, hyperpyrexia, flushing, shivering, myoclonus, rigidity, tremor, diarrhea, hypertension, tachycardia, seizures, and coma. Death has occurred in some cases.
- http://www.ncbi.nlm.nih.gov/pubmed/17157368 (?)
- http://www.ncbi.nlm.nih.gov/pubmed/2891392
- http://www.if-pan.krakow.pl/pjp/pdf/2013/3_593.pdf
Opioids & SSRIs
- http://www.ncbi.nlm.nih.gov/pubmed/23391344
- http://www.ncbi.nlm.nih.gov/pubmed/20513454
- http://www.ncbi.nlm.nih.gov/pubmed/16005413
- http://www.ncbi.nlm.nih.gov/pubmed/18676387
- http://www.ncbi.nlm.nih.gov/pubmed/17381671
Tramadol & Benzodiazepines
- Central nervous system- and/or respiratory-depressant effects may be additively or synergistically present. Vomit aspiration a risk when passed out, lay down in recovery position if ingested.
- http://www.ncbi.nlm.nih.gov/pubmed/12842359
Tramadol & MAOIs
- http://www.ncbi.nlm.nih.gov/pubmed/16051647
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2750095/
Tramadol & SSRIs
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714818/
Benzodiazepines & MAOIs
Benzodiazepines & ssris.
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2446479/
- http://www.ncbi.nlm.nih.gov/pubmed/9435993
MAOIs & SSRIs
- http://www.ncbi.nlm.nih.gov/pubmed/24577320
Contributors: Anonymous , Bjorn , Borax , GrimReaper , Reality , Robustrepresent , Roi , Sleep , TripMate
Navigation menu
Click to download our Free Psilocybin Sourcing Guide
The Psilocybin-Blunting Effects of SSRIs and Antidepressants
- Erika Perez
Serotonergic medications like SSRIs have been on the market for treatment of mental health conditions like depression and anxiety for several decades now, and they’ve maintained a steady public backing since their conception.
More recently though, the cultural discussion surrounding these regimens has addressed a wide-reaching dissatisfaction with their often intolerable side effects.
It’s this longing for more deep-rooted and durable antidepressant and integrative mental health treatments that have given our psychedelic renaissance such impassioned communal reinforcement.
To the best of our knowledge, this may be the most comprehensive analysis and review to date on the chemico-biological interactions of these medicines in each of their respective drug classes.
We explore the mechanisms by which antidepressants can reduce or amplify the potency of a psychedelic trip and the safety-first steps you can take to reduce negative interactions.
Whether you’re looking to replace a current medication with psilocybin therapy or seeking to combine traditional talk therapy with psychedelic therapy , this discussion on the psychedelic drug interactions will undoubtedly inform your next steps.
Key Takeaways
- Tapering off antidepressants prior to a psychedelic experience mitigates the blunting effects, allowing for the psychedelic medicine to work uninhibited.
- When tapering off of a prescribed medication, doing so 2 weeks in advance and under the care of a facilitator provides a supportive and safe container for this delicate process.
- Microdosing may be an effective alternative to prescription antidepressants.
- Psychedelic Passage : Your Psychedelic Concierge — The easy, legal way to find trustworthy psilocybin guides, facilitators and psychedelic assisted therapy near you in the United States.
Download Our Free Psilocybin Sourcing Guide
For harm-reduction purposes, we provide links to online psilocybin vendors, local stores, delivery services, and spore vendors for growing your own medicine at home.
Antidepressants That Interact With Psychedelic Medicine
Selective serotonin reuptake inhibitors (ssris).
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Fluvoxamine (Luvox)
- Fluvoxamine CR (Luvox CR)
- Paroxetine (Paxil)
- Paroxetine CR (Paxil CR)
- Sertraline (Zoloft)
Serotonin-norepinephrine reuptake inhibitors (SNRIs)
- Desvenlafaxine (Pristiq)
- Duloxetine (Cymbalta)
- Venlafaxine (Effexor)
- Venlafaxine XR (Effexor XR)
- Milnacipran (Savella)
- Levomilnacipran (Fetzima)
Serotonin partial agonist/reuptake inhibitor (SPARIs)
- Vilazodone (Viibryd)
- Vortioxetine (Trintellix)
Tricyclic antidepressants (TCAs)
- Amitriptyline (Elavil)
- Desipramine (Norpramin)
- Doxepin (Sinequan)
- Imipramine (Tofranil)
- Nortriptyline (Pamelor)
- Clomipramine (Anafranil)
- Maprotiline (Ludiomil)
- Trimipramine (Surmontil)
- Protriptyline (Vivactil)
Monoamine oxidase inhibitors (MAOIs)
- Phenelzine (Nardil)
- Selegiline (Emsam)
- Tranylcypromine (Marplan)
- Isocarboxazid (Parnate)
- Moclobemide
Norepinephrine-dopamine reuptake inhibitors (NDRIs)
- Bupropion (Wellbutrin, Aplenzin)
Atypical agents
- Mirtazapine (Remeron)
- Nefazodone (Serzone)
- Trazodone (Desyrel, Oleptro)
- Buspirone (Buspar)
Expectation Management for the Psychedelic Trip
Assuming well informed expectations for psilocybin therapy is key for having an experience that’s tailored to your body’s metabolic needs and to your present mental health conditions.
While some studies on the matter have yielded contradicting findings, a substantial number of anecdotal reports draw a significant, negative correlation between prolonged use of serotonergic medications and the degree to which a psychedelic trip can be inwardly experienced.
“I am on 200mg of Sertraline and took 3.5gs of shrooms last night. It basically felt the same as the first time I smoked pot. Got the munchies, but no hallucinations unless I closed my eyes, and even then there was hardly anything.” – Reddit User
“I take Zoloft and can NOT trip on shrooms. I’ve tried a few times. I think the Zoloft blocks the trip” – Reddit User
In other words, people who are prescribed these pharmaceutical drugs and take them routinely, have reported experiencing little to no hallucinogenic effects on a standard dose of tryptamines, like psilocybin mushrooms and LSD.
Though this phenomena seems to expand its presence into a plethora of other psychedelic drugs , like Phenethylamines (MDMA, mescaline), today we’ll be settling our attention on the trip-suppressing effects of antidepressant pharmaceuticals.
Let’s begin by discussing the mechanisms that scientists believe are encouraging this mind-body discord.
Please note that the infancy of the psychedelic medicine industry unfortunately limits the range of controlled research studies and clinical trials that have investigated less-discussed, sometimes case-specific nuances of our highly variant body of psychedelics.
Though that’s caused most of our current research to rely largely on anecdotal reports, it’s important to recognize the high and widespread frequency of these discouraging interactions.
For the purpose of offering a comprehensive analysis, we’ll be piecing together the findings of several observational studies, to paint a more conclusive scientific explanation for this absorption-related dysfunction.
Current Research Studies on Antidepressants and Psychedelics
In a 1999 study , researchers deduced that the perceptual distortions experienced from hallucinogenic drugs are mainly hosted by 5-HT2A (serotonin) receptors through glutamatergic transmissions occurring in the cerebral cortex (Aghajanian & Malek).
Substances like LSD and psilocybin are bicyclicly structured into an indole-shaped ring. This form allows them to perfectly attach themselves to our brain’s 5-HT2A (serotonin) receptors.
Picture this as the communion of a particular key with its corresponding lock, like the perfect piece to a complex puzzle.
Now that we understand a small part of psilocybin’s cerebral route , let’s take a look at the mechanisms of antidepressants.
A 2004 study led by Pau Celada and colleagues in 2004, investigated the biological mechanisms of antidepressants. Their findings concluded that antidepressants act as antagonists at the 5-HT2A receptors. (Amargos-Bosch et al.).
What does this mean? Well, first and foremost, it tells us that compounds like LSD and psilocybin target the same receptors as antidepressants .
It also suggests a conflict of chemical interest, where two drugs are attempting to act on serotonin receptors to alter brain function.
While psilocybin is trying to bind to and activate 5-HT2A receptors (in order to elicit hallucinogenic effects), antidepressants are attaching themselves to these same receptors, then blocking the sites to prevent further 5-HTR binding .
This obstructs our body’s biological response to psychedelic drugs that act on 5-HT2AR, since their serotonin chemicals cannot be freely absorbed by the clogged receptor.
Essentially, antidepressants increase extracellular serotonin levels in order to inhibit nerve cells from reabsorbing serotonin that was previously produced by it.
By hindering reabsorption, our brains are given a larger supply of unoccupied serotonin to amplify transmission between its neurons.
A large number of studies hypothesize that down-regulation is the culprit of our brain’s inability to metabolize serotonin, after prolonged antidepressant use. One 2013 study produced findings that supported this notion (Gray et al.).
The study recruited 19 unmedicated subjects with major depressive disorder and compared the binding function of their 5-HT receptors before and after a 5-9 week period of self medication with SSRIs.
Results showed an 18% downregulation of binding functions to 5-HT autoreceptors, congruous with previously conducted animal studies.
This initial reduction is thought to increase the firing rate of serotonergic neurons in later stages of treatment, magnifying this communication by releasing more serotonin.
However, post-treatment results indicate that this surge is not durably maintained without the antidepressant, and instead it causes our brains to have more trouble producing serotonin than it did pre-treatment.
So the big question–how does these findings communicate the brain’s inability to experience normal levels of psychedelic hallucinations, during and after antidepressant use?
Very simply, while on an antidepressant and in the weeks to months after discontinuation, our brains don’t allow psilocybin’s main chemical (serotonin) to attach itself to our serotonin receptors.
Since 5HT receptors are thought to be the main cause of psychedelic effects, an inability to permeate the serotonin reuptake pump means an inability to feel this fungus’ psychoactive properties.
Also, someone who’s only recently stopped prolonged use of antidepressants, may not feel a standard psychedelic dose as potently as someone who’s never been on a serotonergic medication.
Of the very few observational studies directly investigating this phenomenon, a 1996 study recruited 32 volunteers to report on the intensity of their psychedelic experiences while on heavy use of antidepressants (fluoxetine, paroxetine, sertraline, trazodone) (Bronson et al.).
88% experienced a significant reduction of LSD effects after more than 3 weeks of antidepressant dosing.
A 2017 study agreed with these findings, coming to the conclusion that antidepressants evoke 5HT2AR downregulation, consequently blunting the effects of psychedelic drugs (Carhart-Harris & Nutt).
One of their earlier studies examined the effects of tricyclic antidepressants on the LSD experience. After seeking out 10 subjects who had been on TCAs or MAOIs for at least 3 weeks, they gathered their reports on the LSD experience.
A standardized questionnaire revealed a significant correlation between chronic use of TCAs and amplified hallucinatory distortions on LSD. Conversely, participants on MAOIs experienced a significant reduction of subjective LSD effects.
However, another 2017 study came to a much different conclusion. This study found that MAOIs increased the accumulation of 5-MeO-DMT in the central nervous system and enhanced its interaction with 5-HT2A receptors (Halberstadt).
This suggests that MAOIs may increase the effects of 5-MeO-DMT and other tryptamine hallucinogens, rather than decreasing their effects .
We should note though, the study primarily focused on the alteration of the pharmacodynamics of 5-MeO-DMT by MAOIs and did not directly investigate the subjective effects of the combination of MAOIs and tryptamine hallucinogens in humans.
A 2016 literary review by PK Gillman also concluded that MAOIs should not be taken with drugs intended to release serotonin as their interaction could potentially cause serotonin syndrome— a bodily reaction caused by an excessive amount of amassed serotonin, which could be fatal.
He also agreed that this combination could reduce the effects of psychedelics like MDMA and ecstasy.
Anecdotally, we’re seeing that c hronic use of irreversible and non-selective MAOIs can diminish responses to serotonegric psychedelics. Acute use of reversible MAOIS (e.g. harmala alkaloids) can potentiate responses.
To be clear, combining psychedelics with any drug that inhibits serotonin reuptake will increase the chances of serotonin syndrome, also known as serotonin toxicity.
If serotonin is not able to be metabolized, it can overaccumulation in the brain, leading to potentially fatal outcomes.
Buspirone’s blunting effects on psychedelics are not caused by inhibition of reuptake, but by their partial agonist properties that may compete with the psychedelic attempts to enter those same serotonin receptors.
A 2016 study by Pokorny and colleagues used a double blind, within-subject design to analyze the effects of Buspirone on psilocybin hallucinations.
The placebo group was given a small dose of ergotamine, an anti-migraine medication, to compare interactions against larger, regular doses of Buspirone.
The Altered State of Consciousness rating scale was used to detail the subjects’ experiences which produced very strong evidence (p<0.001) for a significant decrease in visual hallucinations and a significant decrease in derealisation and depersonalisation (p=0.062), compared to main scale scores.
Ergotamine did not produce any suppressing effects. These results conclude that Buspirone inhibits hallucinatory effects of psychedelic drugs.
To those who’ve found themselves in this colorless situation, unable to experience the therapeutic effects of psychedelic medicine for many different conditions–never fear.
There are steps we can take to ensure our bodies metabolize psilocybin as they can.

Restoring The Serotonin System After Antidepressant Use
A 2019 study by Kathryn G. Commons and colleagues suggests that autoreceptor desensitization isn’t an effect of antidepressants.
They argue against the hypothesis that long term use of antidepressant medications overstimulates serotonin receptors and permanently reduces their ability to continue emitting this autoinhibitory feedback.
Their research suggests that although desensitization may occur, the unaffected receptors do continue inhibiting reuptake, returning our brain to baseline levels of serotonin production using the compensatory feedback inhibitors that remain.
These findings illustrate a positive outcome that seems in line with many of our client’s experiences: After tapering off antidepressants, the brain’s serotonin system returns close-enough to baseline for journeyers to feel the effects of psychedelic medicine.
What Have We Seen Anecdotally With Our Clients?
As a company who facilitates psychedelic journeys professionally, we’ve worked with both clients who are on antidepressants and those who are not.
Our take is that antidepressants don’t pose a safety concern when combined with psilocybin treatment, but they do tend to interfere with client expectations.
Chances are if you’re exploring an intentional psychedelic experience, you’re seeking some sort of change.
The challenge is this—what happens if you put all the time, energy, and money towards preparing for a psychedelic experience only to have nothing happen?
For most people, the answer is disappointment. This is why we typically discourage combining serotonergic medications with psilocybin.
The interesting thing is that we’ve had clients send us this study from 2021 which shows the SSRI’s don’t interfere with the psychedelic experience—but we’ve found that doesn’t hold true–at least not with all medications.
While the study is a great data point, it’s also important to consider the results we’ve seen anecdotally working with clients first-hand over the last several years.
We’ve sat with some clients who are taking SSRIs and are able to have psychedelic experiences—they typically just need a higher dose of psilocybin.
Alternatively, we’ve sat with clients who are taking SSRIs who eat 10+ grams of mushrooms and experience no effects at all.
So, it’s not that this study is ‘wrong’—just that it doesn’t paint the full picture.
At this point in time, we don’t have enough information to accurately predict whether a client will have a significant psychedelic experience while taking SSRIs—some will and some won’t.
The question is, is that a risk you’re willing to take as a journeyer? Only you know the answer to that question.
How Long Do I Need to Discontinue Use?
Understanding what should be naturally expected from our body’s present conditions is step number one. Conscious and safe preparation for the psychedelic experience in step number two for ensuring you preserve your physical and mental health.
Before diving into some relevant and effective options for getting the most out of your magic mushrooms, please be advised that cessation of any medical treatment like antidepressants, should always be discussed with your psychiatrist beforehand.
Antidepressant dosage reduction or termination should always be done under the supervised care and direction of a medical professional and should never be abruptly withdrawn.
Abrupt discontinuation of antidepressant medications can worsen mental health conditions and cause emotional instability and volatility.
Having said that, we understand it can be intimidating to approach your doctor with psychedelic-related concerns. If you need some guidance, check out our article on how to speak with your doctor about psilocybin therapy.
Now, let’s review what can be done to promote better absorption of psilocybin to hopefully yield more adequately-weighted therapeutic psychedelic effects:
- If you’re taking any of the SSRIs or SNRIs referenced in the first chart, including SPARI drugs like Vibryyd (Vilazodone) or Trintellix (Vortioxetine), with the exception of fluoxetine, consider tapering off of your meds no less than 2 weeks before your psychedelic journey.
If you’re on fluoxetine , discontinuation of medication should occur at least 6 weeks prior to your journey. By the time you’re ready to embark on the trip, you should have ceased consumption of any SSRI drug.
- Fortunately, there are no reports of reduced psychedelic effects on Wellbutrin , but some would advise tapering medication as a precaution, correlating the length of premeditated discontinuation to the potency of desired effects.
- On a Mirtazapine medication, tapering should also allow for a 2 week period of discontinued use, prior to your trip. Mirtazapine could dull psychedelic experiences, similar to SSRIs and SNRIs, but its blunting mechanisms lie in a blockage of the 5HT2A receptor, rather than blocking the 5HT reuptake pump.
- This same 2 week tapering regimen should be applied for those on Tricyclic antidepressants . Discontinuation before a psychedelic trip is advised due to the potential for experiencing intensified psychedelic effects and serotonin syndrome.
- If on Trazodone , tapering and discontinuation should be in effect a minimum of 5 days before a trip to prevent blunting effects.
- Buspirone consumers should also follow the 5-day minimum to avoid the same events.
- MAOIs should be discontinued through tapering 2 weeks before a trip for these same reasons.
The combination of Lithium and psilocybin appears to pose potential risks, as it may lead to toxicity and increase the likelihood of adverse outcomes such as seizures, serotonin toxicity, or negative experiences.
How Microdosing & Psychotropic Medication Can Help
Microdosing psilocybin mushrooms can potentially be helpful for those looking to taper off of psychotropic medications such as antidepressants, anti-anxiety medications, stimulants, antipsychotics, and mood stabilizers.
This is because psilocybin binds to the 5-HT receptors which are linked to mood, social behavior, sexual desire, memory, sleep, appetite and digestion among many other things.
In other words, the benefit to including microdoses of psilocybin while tapering off of pharmaceuticals is that it provides a natural supplement to the systems influenced by psychotropic medications.
This effect lessens or even eliminates the pharmaceutical withdrawal side effects altogether (things like brain zaps, fatigue, irritability, etc.).
Many people report feeling lighter and more alive while taking microdoses with their psychotropic medications, even while tapering.
The other benefit to microdosing during the tapering process is that it increases neuroplasticity in the brain (Ly et al., 2018 ). Although microdosing effects are sub-perceptual, they allow for the brain to form and reorganize synaptic connections.
In other words, a microdosing protocol allows the brain to be re-wired in a way such that it is not dependent on pharmaceutical medications.
In summary, microdosing psilocybin potentially allows one to taper off of their psychotropic medications faster and with far fewer withdrawal side effects.
Important Note: Because many psychotropic medications also work through the serotonin pathways, it will likely require a higher dose of psilocybin for the effects to be felt. This is normal, simply adjust your dosage as necessary.
How to Determine Your Psychedelic Dose
Until recently, assessing the potency of psychedelic substances required sending samples to a lab, a costly and time-consuming process. However, recent advancements have led to the availability of at-home testing kits, including ones for mushroom material.
These at-home kits, like QTests by Miraculix , not only confirm substance presence but also provide precise measurements of potency, either in milligrams or as a percentage. This enables users to accurately dose and tailor their experiences, crucial for avoiding overwhelming or underwhelming effects.
Understanding potency is essential for therapeutic use, as different doses can result in vastly different experiences. For microdosing, it ensures consistent daily doses.
Qtests offers:
- MDMA test kit
- LSD test kit
- Psilocybin mushroom test kit
- Cannabis test kit .
QTests provide a scientifically validated method for determining the concentration of unregulated substances, granting both journeyers greater control over treatment processes and safeguarding the potential benefits of psychedelic therapies.
Explore Harm Reduction Products:
- The Best Purity Test Kits for Psychedelic Therapy
- How to Test The Potency of Psychedelics At Home: Mushrooms, LSD, MDMA
- The Best Mushroom Grow Kits for Psychedelic Therapy
- The Best Spore Vendors for Psychedelic Therapy
Helpful Tips For Tapering Off of Antidepressants
The best way to taper off, adjust, or eliminate any medication is with the supervision and guidance of your prescribing doctor or psychiatrist .
However, we also recognize that many doctors are better at prescribing medications than they are at helping people taper.
This often results in them recommending tapering regimens that are far too aggressive and lead to significant withdrawal symptoms.
For most people, these withdrawal symptoms are so disruptive and debilitating that it seems easier to continue to use a particular pharmaceutical drug in order to avoid the return of depressive symptoms.
In an effort to provide you with some general guidelines, we’ve outlined a tapering protocol established by Adele Framer, the founder of survivingantidepressants.org :
Since 2011, Surviving Antidepressants has advocated a conservative 10% reduction per month of the most recent dose – an exponential taper, the size of each reduction becoming progressively smaller, approximating the hyperbolic method endorsed by recent research (Framer, 2021 ).
These gradual tapers to minimize withdrawal symptoms typically require the creation of customized dosages and take many months to several years, depending on individual tolerance for dosage reduction.
Why reductions at monthly intervals? Although diagnostic criteria require withdrawal to appear within a week of dosage reduction, our members report it can take several weeks (or more) for them to appear.
People may not recognize incipient symptoms themselves or it may take some time for symptoms to culminate. Pharmacokinetically, enough residual drug may be active to forestall withdrawal symptoms through the washout period.
If the taper proceeds without significant problems, for most drugs, people generally reduce to less than 2.5% of the original dosage before stopping completely.
Given the potential lag time in emergence of withdrawal side effects, the person should be monitored for at least 3 months after discontinuation, with low-dose reinstatement at the ready should subsequent withdrawal symptoms appear.
To reiterate, taper slowly and listen to your body at all times. It is common for withdrawal side effects to have a delayed onset up to 2 weeks.
Oftentimes a more conservative tapering process will be faster in the long run than forcing things and ending up in the start/stop cycle.
What About Medications Other Than Antidepressants?
Stimulant medications like Adderall and Vyvanse have a much shorter half life. Prescription stimulants may not affect the psychedelic experience noticeably. For more information, check out “ Can You Mix Psychedelic Mushrooms With Adderall and Stimulants? “.
The procedure for using psychedelics if you’re on opioids may be dependent on the specific medication you’re on. However, a medication like Wellbutrin ( Bupropion ) is a non-issue in combination with serotonergic psychedelics.
Bupropion primarily affects the norepinephrine and dopamine systems, with minimal direct impact on serotonin. Psilocin, on the other hand, primarily affects serotonin receptors. This suggests that the two drugs have different primary mechanisms of action and do not directly interact at the receptor level.
Additionally, Bupropion is metabolized in the liver, primarily by CYP2B6, to its active metabolites. Psilocin is metabolized from psilocybin through a different pathway. Therefore, there is no known direct interaction between these metabolic pathways.
Atypical antipsychotics (e.g. chlorpromazine, risperidone, ketanserin) appear non-toxic but diminish responses to serotonergic psychedelics.
Typical antipsychotics (e.g. haloperidol) appear to increase risks of anxious ego-dissolution and dysphoric experience.
Buspirone appears non-toxic but may compete with psilocin or downregulate serotonin receptors to diminish responses.
When it comes to other psychotropic medications, we suggest speaking with our team of psychedelic concierges to ensure that all potential contraindications are accounted for.
Drugs like benzodiazepines should never be tapered off of without consulting a medical professional. The withdrawal symptoms of benzodiazepines can be life threatening and should not be taken lightly.
Helpful Resources
- Should I Stop Using Antidepressants for Psychedelic Therapy?
- Top 5 Ways to Consume Psychedelic Mushrooms for Therapy
- How Often Should You Take Psilocybin Mushrooms?
- How Long Should You Microdose Psychedelic Mushrooms For?
- The Psychedelic Therapy Process: A Step-by-Step Guide
Our Services & How We Support Your Psychedelic Journey
Psychedelic Passage is dedicated to supporting your psychedelic journey through providing access to safety resources and psychedelic facilitation services.
We believe in the transformative potential of psychedelics when approached with the right knowledge, guidance, and preparation. Our commitment is centered on providing access to accurate and comprehensive information about these medicines.
We offer you access to a network of pre-vetted professional psychedelic facilitators who are experienced and well-trained, specializing in guiding individuals through their psychedelic experiences in a safe and supportive manner.
They play a crucial role in ensuring a positive and enriching journey by providing guidance on contraindications, proper dosing, and general preparation.
On the day of your psychedelic journey, our facilitators are there to offer continuous support, creating a nurturing and comfortable environment for your experience.
Overall, our organization strives to empower and support individuals on their psychedelic journey, offering a holistic approach that includes education, guidance, preparation, day-of support, and integration assistance.
Get Matched with a Trusted Psychedelic Therapy Provider Near You
Hi there! We sincerely hope that you’ve found valuable takeaways that resonate with your current intentions. To explore research-based education, stay updated with psychedelic news, and benefit from practical how-to articles, we encourage you to head over to our resources page .
If you’re seeking personalized advice and are prepared to take the first step toward a therapeutic psychedelic experience, we invite you to book a consultation with our team of experienced psychedelic concierges.
This consultation is more than just a conversation; it’s an opportunity to be matched with a trustworthy local facilitator. You’ll be seamlessly connected to our rigorously vetted network of psychedelic guides, ensuring potential matches align with your needs.
Psychedelic Passage offers confidence and peace of mind by alleviating the burden of having to guess who’s right for you. If you want to discover how Psychedelic Passage can help you, we empower you to learn more about our services and check out client testimonials from those who’ve gone before you.
Your healing path is uniquely yours, and our commitment is to serve you at every juncture. Psychedelic Passage: Your Psychedelic Concierge — The easy, legal way to find trustworthy psilocybin guides, facilitators and psychedelic assisted therapy near you in the United States.
Learn More About Our Network
- Meet Our Referral Network
- Explore Frequently Asked Questions
- Watch Client Testimonials
- Book a Consultation Call
- Is Psychedelic Passage Safe & Legit?
Frequently Asked Questions: Antidepressants & Psychedelics
Q: can i take antidepressants and psychedelics together.
It’s generally advised to avoid combining antidepressants with psychedelics due to potential interactions. Antidepressants, especially SSRIs, can diminish or alter the effects of psychedelics, making the experience unpredictable and potentially less effective.
Aside from psychedelics being blunted by antidepressants, combining the two could potentially increase the risk for serotonin syndrome, so it’s best to taper off prior to ingesting psychedelics.
Q: Can psychedelics be used as an alternative to traditional antidepressant medications?
Psychedelics — specifically psilocybin—have been shown in recent studies to be an effective antidepressant and even treatment method for treatment-resistant depression.
However, they are not currently approved as a standard alternative to traditional antidepressants given the complex legality around these substances.
Q: How might psychedelics affect my mental health if I have a history of depression?
Because depression is a complex condition, there is no guarantee that taking a psychedelic will have a reliable effect (but then again, even prescribed medications have the same issue).
Overall, many studies suggest potential therapeutic benefits for depression, but in cases of extreme mental health issues, consulting a professional and having a great deal of support is pertinent if experimenting with these medicines.
Connect With Psychedelic Passage
- Listen to our podcast on Spotify , Apple Podcasts , and iHeartRadio
- Subscribe to our Youtube Channel
- Follow us on Instagram , Reddit , Twitter , and Linked in for bite-sized updates and content.
Looking for a professionally supported in-person psychedelic experience?
Take the first step and book a consultation call with us today. We'll walk you through every step of the process after getting to know you and your unique situation.
Related posts
How can psychedelics benefit someone who is happy.
With all the emphasis on how psychedelics are helpful in treating mental health conditions, many people who aren’t dealing with a diagnosis have been left
How To Use Psychedelics for Transcendental Healing? 7 Tips
Psychedelics have been used as sacramental tools for transcendental healing for thousands of years. For many in the Western world, the idea of psychedelics as
At Psychedelic Passage, we offer professional 1-on-1 guidance and companionship on your journey of healing. We simply can't sit back and let Americans continue to sit in silent suffering trying to battle mental health issues within a broken health care system, all while knowing that effective alternatives exist. We stand for the sacred, at-home, ceremonial use of psychedelics for consciousness exploration, which we believe to be a fundamental human right.
Everything you need to know about how our service works
See the questions most of our clients ask
All you need for proper preparation, integration and ceremony
Sign up for our newsletter and get our free psilocybin sourcing guide
We only send you what you need to know to use psychedelics for your healing journey.
- Website by SQ
- Privacy policy
- Terms of use
- © Psychedelic Passage. All rights reserved
DISCLAIMER: Psychedelic Passage does not provide psychoactive or controlled substances. Many controlled substances are illegal. The illegal use of a controlled substance may result in criminal consequences. Using controlled substances outside of the lawful supervision of a medical professional may also result in serious health complications including death. We are not licensed therapists, counselors, or medical professionals. We are not spiritual guides or scientists. We are a harm reduction company. Please use your discretion and consult a medical professional to ensure our services meet your needs. Any referrals to third parties that we may provide are informational, for your convenience only, and based on the criteria you provide to us. You are solely responsible for making a selection of a practitioner or other service and determining whether he/she/they are appropriate for you. No referral is an endorsement or recommendation of the practitioner or their services. Please conduct your due diligence on any practitioner you use. We do not provide referrals to “underground” (illegal) psychedelic services. Any information received through our services should be considered for educational purposes and not be misconstrued as medical or legal advice. Please use your discretion and consult with a medical professional to ensure our services meet your needs.
13918 E. Mississippi Ave. #68175 Aurora, CO 80012
Search for anything like: microdosing, dosage, integration
Get Your Free Psilocybin Sourcing Guide!
Just tell us where to send it…
Download Our Free Psilocybin Sourcing Guide!
Congratulations we've sent the sourcing guide to your inbox. .
You can now close this window.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- VA Author Manuscripts

Drug-drug interactions between psychiatric medications and MDMA or psilocybin: a systematic review
Aryan sarparast.
1 Department of Psychiatry, Oregon Health & Science University, Portland, OR 97239, USA
Kelan Thomas
2 College of Pharmacy, Touro University California, Vallejo, CA 94592, USA
Benjamin Malcolm
3 Awake Movement LLC, Chino Hills, CA, USA
Christopher S. Stauffer
4 Department of Mental Health, VA Portland Health Care System, Portland, OR 97239, USA
Associated Data
Rationale & objectives.
±3,4-Methylenedioxymethamphetamine (MDMA) and psilocybin are currently moving through the US Food and Drug Administration’s phased drug development process for psychiatric treatment indications: posttraumatic stress disorder and depression, respectively. The current standard of care for these disorders involves treatment with psychiatric medications (e.g., selective serotonin reuptake inhibitors), so it will be important to understand drug-drug interactions between MDMA or psilocybin and psychiatric medications.
In accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we queried the MEDLINE database via PubMed for publications of human studies in English spanning between the first synthesis of psilocybin (1958) and December 2020. We used 163 search terms containing 22 psychiatric medication classes, 135 specific psychiatric medications, and 6 terms describing MDMA or psilocybin.
Forty publications were included in our systematic review: 26 reporting outcomes from randomized controlled studies with healthy adults, 3 epidemiologic studies, and 11 case reports. Publications of studies describe interactions between MDMA ( N = 24) or psilocybin ( N = 5) and medications from several psychiatric drug classes: adrenergic agents, antipsychotics, anxiolytics, mood stabilizers, NMDA antagonists, psychostimulants, and several classes of antidepressants. We focus our results on pharmacodynamic, physiological, and subjective outcomes of drug-drug interactions.
Conclusions
As MDMA and psilocybin continue to move through the FDA drug development process, this systematic review offers a compilation of existing research on psychiatric drug-drug interactions with MDMA or psilocybin.
Introduction
Preliminary evidence for the use of ± 3,4-methylenedioxymethamphetamine (MDMA) ( Jerome et al. 2020 ; Mitchell et al. 2021 ) and psilocybin ( Carhart-Harris et al. 2021 ; Castro Santos and Gama Marques 2021 ; Davis et al. 2021 ) in the treatment of psychiatric disorders has been promising. Both drugs have been studied as augmentation to psychotherapy and are typically only administered one to three times during a treatment course ( Mithoefer et al. 2016 ). This represents a departure from traditional pharmacological treatment in psychiatry. MDMA and psilocybin were researched as clinical interventions beginning in the 1970s and 1960s, respectively. However, the field of psychiatry has a limited understanding of their therapeutic use due to their Schedule I categorization (i.e., drugs determined to lack safety even under medical supervision, have no currently accepted medical use, and are deemed to have a high potential for abuse). Despite MDMA and psilocybin’s categorization as Schedule I substances, the US Food and Drug Administration (FDA) has more recently granted Breakthrough Therapy designation to MDMA-assisted psychotherapy (MAP) for Posttraumatic Stress Disorder (PTSD) as well as psilocybin-assisted psychotherapy (PAP) for both Major Depressive Disorder (MDD) and Treatment-Resistant Depression (TRD). Breakthrough Therapy designation is a process designed to expedite the development and review of drugs intended to treat a serious or life-threatening condition for which preliminary clinical evidence suggests substantial improvement over available options. MAP and PAP are currently being studied in Phase III and Phase II manufacturer-sponsored clinical trials, respectively. Upon successful completion of Phase III trials, a manufacturer may submit a New Drug Application asking the FDA to consider a drug for marketing approval.
MAP and PAP have shown transdiagnostic therapeutic potential beyond PTSD and depression, including as treatments for anxiety disorders ( Danforth et al. 2018 ; Moreno et al. 2006 ; Vargas et al. 2020 ) and substance use disorders ( Bogenschutz et al. 2015 ; Johnson et al. 2014 ; Sessa et al. 2021 ). All of the above-mentioned indications are frequently treated with psychiatric medications, such as: adrenergic agents, antipsychotics, anxiolytics, mood stabilizers, psychostimulants, and antidepressants. In fact, a combination of multiple psychiatric medications (i.e., polypharmacy) is common in the clinical management of MDD ( Blier et al. 2010 ; Carpenter et al. 2002 ) and PTSD ( Khachatryan et al. 2016 ; Krystal et al. 2011 ). With the number of clinical trials of MAP and PAP increasing exponentially, and potential FDA approval in the pipeline, it is important to compile what we know about the potential drug-drug interactions between psychiatric medications and MDMA or psilocybin.
MDMA is a phenethylamine compound with psychostimulant effects. It promotes social engagement ( Kirkpatrick and de Wit 2015 ), openness ( Wagner et al. 2017 ), receptiveness to positive affect ( Hysek et al. 2012b ), heightened empathy ( Hysek et al. 2014a ), and increased disclosure of emotional content in dialogue ( Baggott et al. 2015 ), leading to its characterization as an “entactogen-empathogen.” These effects distinguish MDMA from “classic psychedelics.” The active dose range of MDMA in studies is 75–225 mg administered orally ( Multidisciplinary Association for Psychedelic Studies 2021 ). The onset of pharmacological effects usually occurs 30–60 min after ingestion, with peak effects appearing 75–120 min after ingestion and a total duration of 3–6 h ( Multidisciplinary Association for Psychedelic Studies 2021 ). The elimination half-life is 8–9 h.
MDMA reverses the action of monoamine transporters, which include the serotonin transporter (SERT), norepinephrine transporter (NET), and dopamine transporter (DAT) ( Rudnick and Wall 1992 ). MDMA also competes with monoamines for sites on the vesicular monoamine transporter-2 (VMAT-2) ( Partilla et al. 2006 ), suggesting that MDMA leads to the displacement of monoamines from presynaptic vesicular stores as well. Together, transporter reversal and emptying of vesicular stores results in increased concentrations of intrasynaptic monoamines: predominantly serotonin (5-HT), to a lesser degree norepinephrine (NE), and to the least degree dopamine (DA) ( Bogen et al. 2003 ; Oeri 2021 ). Additionally, MDMA displays some binding affinity as an agonist at 5-HT 1A , 5-HT 2A , 5-HT 2B and 5-HT 2C serotonin receptors; α 1 -, α 2A - and β-adrenergic receptors; D 1 - and D 2 -dopamine receptors; M 1 - and M 2 -muscarinic receptors; H 1 -histamine receptor; and minimally at the human trace amine-associated receptor 1 (TAAR1) ( Battaglia et al. 1988 ; Oeri 2021 ). The S( +)-MDMA enantiomer has a stronger binding affinity to radiolabeled brain serotonin and dopamine binding sites than R(−)-MDMA ( Lyon et al. 1986 ; Shulgin 1986 ). Recent MAP clinical trials have used a racemic mixture of MDMA. MDMA’s downstream effects include increased secretion of arginine vasopressin ( Simmler et al. 2011 ), adrenocorticotropic hormone (ACTH) ( Grob et al. 1995 ), cortisol, prolactin, and oxytocin ( Hysek et al. 2014a ). MDMA is metabolized by cytochrome P450 enzymes ( Table 1 ), primarily CYP2D6 followed by catechol-O-methyltransferase to its main inactive metabolite 4-hydroxy-3-methoxymethamphetamine (HMMA) ( Abraham et al. 2009 ). MDMA also has a minor metabolism pathway via CYP3A4, CYP1A2, CYP2B6, and CYP2C19 to its only active metabolite 3,4-methylenedioxyamphetamine (MDA) ( Vizeli et al. 2017 ). MDMA is also thought to lead to auto-inhibition of CYP2D6, resulting in nonlinear pharmacokinetics ( Kolbrich et al. 2008 ). MDMA and its metabolites are primarily excreted as conjugates, such as sulfates and glucuronides ( Vizeli et al. 2017 ).
Main enzymes involved in MDMA & psilocybin metabolism
Bold = primary metabolic enzyme(s)
Common physiological effects of MDMA include increased heart rate, blood pressure, temperature, pupil size, as well as adverse acute transient physical effects such as nausea, vomiting, bruxism, muscle aches, headache, sweating, fatigue, dizziness, and dry mouth ( Multidisciplinary Association for Psychedelic Studies 2021 ). MDMA increases plasma epinephrine and NE ( Hysek and Liechti 2012 ; Pacifici et al. 2004 ). Common psychological effects of MDMA include euphoria, anxiolysis, enhanced fear-extinction learning, feelings of closeness or connectedness, an expanded emotional range ( Carhart-Harris et al. 2014 ; Sessa 2017 ), as well as adverse subjective effects such as fearfulness, dysphoria, confusion, sleeplessness, and decreased appetite ( Baylen and Rosenberg 2006 ). MDMA’s properties as an ‘empathogen-entactogen’ may have specific advantages in the treatment of PTSD including promoting increases in the personality feature of openness ( Wagner et al. 2017 ), large magnitudes of posttraumatic growth (i.e. positive changes in self-perception, interpersonal relationships, or philosophy of life) ( Gorman et al. 2020 ), fear extinction ( Feduccia and Mithoefer 2018 ), widened window of tolerance ( Mithoefer et al. 2011 ), and reopening of the critical period for social reward learning possibly mediated by oxytocin release (in mice, Nardou et al. 2019 ).
In recreational settings, MDMA is colloquially known as “ecstasy” or “molly.” Past year illicit use among US persons aged 12 or older was approximately 1.0% of the population between 2015 and 2019 ( Center for Behavioral Health Statistics and Quality 2020 ). Unverified recreational ecstasy pills often consist of variable doses ranging from no detectable MDMA to 280 mg or more ( Morefield et al. 2011 ; Wood et al. 2011 ). Ecstasy is frequently adulterated with other substances prior to sale ( Saleemi et al. 2017 ; Togni et al. 2015 ). Additionally, ecstasy use is often intentionally co-ingested with other substances ( Rigg and Sharp 2018 ), and involves situational risk factors such as heavy physical exertion, excessive heat, low water intake or water intoxication, and lack of screening for medical risk factors. In these settings, several types of short and longer-term adverse effects have been reported, including seizures, rhabdomyolysis, cardiovascular events, neurocognitive dysfunction, psychiatric crisis, habituation and addiction, and death ( Grob and Grigsby 2021 ). Case reports and epidemiologic analyses of drug interactions from these recreational settings are much less reliable and present major limitations. In contrast to recreational use, clinical trials to date have involved carefully screened participants ingesting laboratory-grade MDMA at precise dosages. There has only been one reported serious adverse reaction to MDMA within a clinical trial setting: one participant experienced exacerbated ventricular extrasystoles after 125 mg of MDMA, which resulted in overnight hospital monitoring and full recovery within one day ( Multidisciplinary Association for Psychedelic Studies 2021 ). Moderate doses utilized in MAP clinical trials, administered only two or three times during a course of treatment, have not resulted in persistently detectable deficits in neurocognitive function ( Grob and Grigsby 2021 ).
Psilocybin (4-phosphoryloxy-N,N-dimethyltryptamine) is a psychoactive tryptamine that naturally occurs in over 200 species of mushrooms, most notably from the genus Psilocybe ( Nichols 2020 ). It is often referred to as a “classic psychedelic,” since the drug-induced alterations of perception, emotion, and cognition are primarily related to 5-HT 2A receptor agonism ( Johnson et al. 2019 ), though it also binds to other 5-HT receptor subtypes ( Nichols 2020 ). Pooled data from 579 oral psilocybin doses administered across completed clinical trials involved a broad range of dosing for psilocybin from “very low dose” (0.014 mg/kg) to “high dose” (0.6 mg/kg), corresponding to 3.15–42 mg in a 70-kg human ( Usona Institute 2021 ). The subjective effects of psilocybin usually begin 20–40 min after ingestion, peak after 60–90 min, and have a total duration of 6 h ( Hasler et al. 2004 ).
Psilocybin is a prodrug, rapidly dephosphorylated upon ingestion by alkaline phosphatase or non-specific esterases, to its active metabolite, psilocin ( Thomas et al. 2017 ). Psilocybin and psilocin lack clinically significant inhibitor activity at monoamine reuptake pumps, such as SERT or VMAT-2, thus do not result in substantially increased intrasynaptic serotonin ( Rickli et al. 2016 ). Due to minimal intrasynaptic serotonin release, psilocybin’s mechanism of action is unlikely, even in high doses, to result in serotonin toxicity ( Malcolm and Thomas 2021 ). Psilocin metabolism primarily occurs via UDP-glucuronyltransferase enzymes, UGT1A9 and UGT1A10 ( Table 1 ) ( Dinis-Oliveira 2017 ; Manevski et al. 2010 ). Psilocin also undergoes deamination and demethylation to form the inactive metabolite 4-hydroxy-indole-3-acetic acid (4HIAA) ( Manevski et al. 2010 ).
Physiologically, psilocybin is known to cause mild increases in blood pressure and heart rate ( Thomas et al. 2017 ). Common physical adverse effects include headache, nausea, dizziness, and fatigue ( Usona Institute 2021 ). Psilocybin can elicit subjective experiences with mystical-type qualities, such as an increased sense of unity, transcendence of time and space, loss of self, and euphoria ( Griffiths et al. 2006 ; Studerus et al. 2010 ). Mystical-type experiences are correlated in the laboratory with diminished activity of functionally connected brain circuits collectively termed the default mode network (DMN) as well as long-term improvements in wellbeing, psychosocial function, symptoms of clinical illness, and mindfulness-related capacities ( Barrett and Griffiths 2018 ; Griffiths et al. 2008 ). Psilocybin lacks dopamine-mediated reinforcement, and there is no evidence supporting potential for habituation or addiction despite development of rapid tolerance with repeated administration ( Johnson et al. 2018 ). Common adverse psychological effects include transient anxiety, dysphoria, impaired sleep, paranoia, grief, and preoccupation with death ( Barrett et al. 2016 , Usona Institute 2021 ).
While laboratory-made synthetic psilocybin is typically used in clinical trials, psilocybin is often ingested for personal use as “magic mushrooms.” Pooled data from the 2015–2018 National Survey on Drug Use and Health shows that approximately 9.68% of US adults have ever used psilocybin in their lifetime ( Yockey and King 2021 ). Psilocybin is known to have a wide margin of safety, with lethal doses of psilocybin estimated to be more than 1000-fold higher than therapeutic doses ( Gable 2004 ; Johnson et al. 2018 ). There have been no serious adverse events related to psilocybin in clinical trials ( Thomas et al. 2017 ). Compared to personal use of other psychedelics, psilocybin appears to have the lowest rates of adverse events reported to poison control centers and very few reports of cardiovascular events ( Borowiak et al. 1998 ; Leonard et al. 2018 ).
Drug interaction potential
Given that both MDMA and psilocybin modulate serotonin neurotransmission, there is a potential for drug-drug interactions with medications that also modulate the serotonin system, including Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), Tricyclic Antidepressants (TCAs), Monoamine Oxidase Inhibitors (MAOIs), mirtazapine, trazodone, lithium, buspirone, atypical antipsychotics, and others. Some of these interactions may increase the risk of toxidromes such as serotonin syndrome ( Malcolm and Thomas 2021 ). Another pharmacodynamic interaction that may occur is the attenuation of MDMA’s subjective effects or reduced efficacy of MAP for PTSD in participants with recent exposure to antidepressant drugs that inhibit reuptake transporters ( Hysek et al. 2012d ; Feduccia et al. 2020 ). While a history of SSRI usage ever in one’s lifetime does not seem to be associated with reduced MAP efficacy ( Mitchell et al. 2021 ), the adequate washout period between SSRI use and MAP has not yet been delineated. Due to MDMA also acting on the NE and DA neurotransmitter systems, there are potential interactions with drugs that target these neurotransmitters as well, such as SNRIs, bupropion, and psychostimulants. There may also be relevant drug-drug interactions between psychiatric medications and MDMA or psilocybin through more indirect mechanisms. For example, GABAergic agents such as benzodiazepines have been advocated as an intervention to mitigate acute psychological or physiological adverse effects related to psychedelics ( Johnson et al. 2008 ). From a pharmacokinetic perspective, other medications may be substrates, inhibitors (e.g., CYP2D6, which could result in competitive interactions with MDMA), or inducers of drug-metabolizing enzymes. While interactions with UGTs are not as common, there are some medications that inhibit or induce UGT enzymes, which may theoretically affect the metabolism of psilocybin ( English et al. 2012 ).
Objective of systematic review
Although reviews of drug-drug interactions (DDI) with MDMA have been published ( Papaseit et al. 2020 ), none have been systematic, and there have been no reviews of DDIs with psilocybin. Therefore, the objective of this systematic review is to summarize all existing data related to pharmacokinetic, physiological, and subjective effects of drug-drug interactions between medications prescribed in psychiatry and MDMA or psilocybin.
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. PROSPERO 2021 registration ID: CRD42021233519. The PICOS (Participants-Intervention/Exposure-Comparison-Outcomes-Study) framework was used to guide the methods of this review. Participants are people of any age who were exposed to, or ingested, MDMA or psilocybin in combination with a psychiatric medication. For clinical trials, comparison is made between MDMA or psilocybin in combination with a psychiatric drug versus MDMA or psilocybin alone. Outcomes include measures of pharmacokinetics (e.g., plasma drug and metabolite levels), physiology (e.g., vital signs, circulating catecholamines), and subjective outcomes (e.g., psychological effects, list of complaints). Study type was defined broadly to include meta-analyses, systematic reviews, randomized controlled trials (RCTs), retrospective studies, cross-sectional studies, case–control studies, cohort studies, and case reports.
A list of psychiatric medications (see Table 2 ) was compiled using the APA Textbook of Psychopharmacology, 5 th Edition , Appendix for the psychiatric pharmacopoeia in the United States ( Schatzberg and Nemeroff 2017 ). Given that clinical research investigating MDMA and psilocybin is also being conducted outside of the United States (e.g., {"type":"clinical-trial","attrs":{"text":"NCT01689740","term_id":"NCT01689740"}} NCT01689740 , {"type":"clinical-trial","attrs":{"text":"NCT04670081","term_id":"NCT04670081"}} NCT04670081 ), we referenced Martindale: The Complete Drug Reference ( Scriba 2011 ) and included any internationally-approved pharmacotherapy for the treatment of PTSD and MDD that we had not already included. Lastly, we referred to the Department of Veterans Affairs and Department of Defense practice guidelines for PTSD and MDD to include additional medications that are not typically categorized as psychiatric drugs, but are used in the treatment of these disorders (e.g., prazosin, liothyronine) ( VA/DOD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder 2017 ).
Psychiatric medication and medication class search terms
Search strategy
We searched the MEDLINE database via PubMed for publications in English between 1958 and 2020. This date range was chosen to capture relevant scientific literature beginning with the synthesis and formal research use of psilocybin ( Hofmann et al. 1958 ) as well as the early use of MDMA’s therapeutic properties in psychotherapy starting in the 1970’s ( Passie 2018 ). We utilized the PubMed Advanced Search Builder to conduct a query comprising 163 terms included in the Title or Abstract. A total of 22 search terms reflecting psychopharmacology classes and 135 search terms reflecting psychiatric medications (e.g., Tricyclic antidepressant OR Desipramine OR Nortriptyline) were combined using the logical operator AND with 6 search terms aimed to capture MDMA OR psilocybin (“psilocybin” OR “mdma” OR “ecstasy” OR “psychedelic” OR “entheogen” OR “3 4 methylenedioxymethamphetamine”). See Tables 2 and and3 3 for the full list of search terms. A total of 21 filters were applied: case reports, classical article, clinical conference, clinical study, clinical trial, clinical trial protocol, phase 1 clinical trial, phase 2 clinical trial, phase 3 clinical trial, phase 4 clinical trial, comparative study, controlled clinical trial, historical article, meta-analysis, multicenter study, observational study, practice guideline, pragmatic clinical trial, randomized controlled trial, systematic review, humans. This resulted in a total of 455 abstracts at the time of query (December 21 st , 2020).
Psychedelic-related search terms
Study selection
Each abstract was screened for inclusion by two independent reviewers. Abstracts were excluded if they were an editorial, a duplicate, not available in the English language, or otherwise did not address the objective of this systematic review. Any discrepancies between independent reviewers were discussed among the authors of this systematic review, leading to a final decision to include or exclude a specific article based on unanimous consensus. We assessed the remaining full-text articles in detail, during which 12 additional hand-selected articles arose that had not been captured by our database query. Hand-selected articles were reviewed and met all study selection criteria.
Ultimately, 40 articles were included in our systematic review. See Fig. 1 for a PRISMA flow diagram. 26 RCTs and 3 epidemiologic studies were captured. We corresponded with any researchers who published more than one of the resulting RCT articles to seek unpublished or uncaptured data; no additional data were obtained this way. We included the 3 epidemiologic studies in this review due to their large sample sizes and implications for future hypothesis generation, despite their methodological limitations. In addition, 11 case studies were reviewed and placed in the Supplemental Materials .

PRISMA study selection flow diagram
Percent change calculation
The following formula was utilized to standardize comparison of outcome measures (e.g., Epinephrine nmol/l) when ingestion of MDMA or psilocybin was preceded by ingestion of another drug (e.g., carvedilol) versus preceded by placebo, resulting in a percentage change (e.g., ↑204.3%) in the outcome of interest. V PBO-MDMA refers to the value of the outcome of interest for the MDMA (or psilocybin) pretreatment with placebo condition, and V med-MDMA refers to the value of the outcome of interest for MDMA (or psilocybin) pretreatment with the psychiatric medication.
This review includes 26 publications of RCTs and 3 epidemiologic studies (1 post-marketing surveillance association study, 1 cross-sectional survey, and 1 quantitative analysis). RCTs ( Table 4 ) include combinations of MDMA with SSRIs ( Farré et al. 2007 ; Liechti and Vollenweider 2000a ; Tancer and Johanson 2006 ), SNRIs ( Hysek et al. 2011 ; Hysek et al. 2012d ), bupropion ( Schmid et al. 2015 ), methylphenidate ( Hysek et al. 2014b ), haloperidol ( Liechti and Vollenweider 2000b ), memantine ( de Sousa Fernandes Perna et al. 2014 ), and adrenergic agents ( Hasler et al. 2009 ; Hysek et al. 2010 , 2013 ; Hysek et al. 2012a , b , c ); and combinations of psilocybin with ergotamine or buspirone ( Pokorny et al. 2016 ), haloperidol or risperidone ( Vollenweider et al. 1998 ), chlorpromazine ( Keeler 1967 ), and escitalopram ( Becker et al. 2021 ). Our results include primary outcome publications for 17 original RCTs along with 9 additional analyses of secondary or exploratory outcome measures using the same sample from a previously-published RCT. Exploratory analyses were on drug-drug interactions with MDMA and their effects on: immune response ( Bigler et al. 2015 ; Pacifici et al. 2004 ), drug metabolism ( Pacifici et al. 2004 ; Steuer et al. 2016 ), plasma copeptin ( Simmler et al. 2011 ), pupillary response ( Hysek and Liechti 2012 ), psychological effects ( Liechti 2000 ), and habituation of startle response ( Liechti et al. 2001 ).
Summary of drug-drug interaction randomized controlled trials
MAOI monoamine oxidase inhibitor, NDRI norepinephrine-dopamine reuptake inhibitor, NMDAR N-methyl-D-aspartate receptor, RCT randomized controlled trial, SNRI serotonin-norepinephrine reuptake inhibitor, SSRI selective serotonin reuptake inhibitor
Not included: MDMA/ecstasy co-ingestion from cross-sectional studies ( Copeland et al. 2006 ; Cohen et al. 2021 ) or epidemiologic data from online “trip reports” ( Nayak et al. 2021 )
All of the RCTs enrolled only “healthy” adults, often recruited from a university campus, and had limited sample sizes (range of 8–23 participants). Several trials also investigated pharmacogenetic biomarkers, such as CYP2D6 genotype, and categorized participants as extensive, intermediate, or poor metabolizers. Common exclusion criteria across clinical trials were pregnancy or nursing, age < 18 or > 45, BMI < 18.5 or > 25 kg/m 2 , presence of psychiatric illness in self or first-degree relatives, and active substance use. Many studies required female participants to be in the follicular phase of their menstrual cycle (day 2–14) during drug dosing due the potential for cyclic change in subjective reactivity to amphetamines ( White et al. 2002 ). Refer to Table 5 for additional details on study designs and study participants and to Tables 6 and and7 7 for pharmacokinetic, physiological, and subjective outcomes of the RCTs included in our systematic review.
Randomized controlled trial designs and participants
Randomized controlled trial outcomes—MDMA
Percent change reported for [psych med] + MDMA vs. placebo + MDMA
↔ no change in response, ∼ = estimated percentage change approximated from graphical representation of outcome data
AUC area under the curve, AUEC area under the effect-time curve, C max peak plasma concentration, DAT dopamine transporter, DBP diastolic blood pressure (mmHg), E max peak effects, HMMA 4-hydroxy-3-methoxymethamphetamine, MAP mean arterial pressure, MDA 3,4-methylenedioxyamphetamine, MDMA 3,4-Methylenedioxymethamphetamine, NET norepinephrine transporter, SBP systolic blood pressure (mmHg), SERT sertraline transporter, Temp temperature (C°), t 1/2 half-life, t max time to maximum plasma concentration, Δ change from baseline
Randomized controlled trial outcomes—psilocybin
Percent change reported for [psych med] + psilocybin vs. placebo + psilocybin
Adrenergic agents & MDMA
RCTs were conducted combining MDMA with four different adrenergic agents: carvedilol, pindolol, clonidine, and doxazosin. These studies were among those hand-selected for inclusion as these medications, or medications from the same class, are occasionally used in clinical psychiatric practice as augmentation treatment (e.g., α 1 -adrenergic receptor blockers for the treatment of PTSD) and may be relevant clinically in the management of common transient effects of MDMA such as elevated blood pressure ( De Jong et al. 2010 ; Kinzie and Leung 1989 ; Scherrer et al. 2019 ).
Hasler et al. (2009) hypothesized that pindolol (20 mg p.o.), a mixed β-adrenergic and 5HT 1A receptor antagonist, administered one hour prior to MDMA (1.6 mg/kg p.o.) would affect MDMA-induced affective, cognitive, and cardiovascular responses ( Hasler et al. 2009 ; Hysek et al. 2010 ). It was found that pindolol pretreatment on average affected experience for only a few subscales of the affective measures (i.e., reduction in MDMA-induced “positive basic mood,” “mania-like experience,” and “dreaminess”) and had no significant effect on MDMA-induced impairments when performing neurocognitive tasks ( Hasler et al. 2009 ). Pindolol pretreatment reduced MDMA-induced increases in peak heart rate, but had no effect on MDMA-induced change in mean arterial pressure, body temperature, or adverse effects ( Hysek et al. 2010 ).
Hysek et al. (2012c) examined the combination of carvedilol (50 mg p.o.), an α 1 - and β-adrenoreceptor antagonist, with MDMA (125 mg p.o.) and found a large reduction in MDMA’s cardiostimulant and hyperthermic effects without significantly affecting MDMA’s subjective effects. Self-reported acute and subacute complaints from MDMA were not significantly affected by carvedilol. Despite the attenuation of MDMA’s physiological effects, there was a significant rise in circulating epinephrine and NE. Carvedilol and MDMA are both CYP2D6 substrates, while MDMA is also an autoinhibitor ( O’Mathúna et al. 2008 ); however, MDMA and MDA plasma levels were unchanged when co-administered with carvedilol compared to MDMA alone.
Hysek et al. (2012a) hypothesized that the α 2 -adrenergic receptor agonist clonidine (150 μg p.o.), when administered one hour prior to MDMA (125 mg p.o.), would modulate the exocytotic release of NE and thus reduce MDMA’s effects. It was found that clonidine did indeed reduce MDMA-induced elevation in circulating NE and blood pressure, but decreased by the same magnitude as clonidine alone. Body temperature, mydriasis, self-reported mood effects and adverse effects from MDMA were not significantly affected by clonidine pretreatment ( Hysek and Liechti 2012 ).
Hysek et al. (2013) hypothesized that pretreatment with the α 1 -adrenergic receptor antagonist doxazosin (8 mg p.o. ~ 16 h prior) would reduce MDMA-induced (125 mg p.o.) increases in blood pressure and positive mood. Indeed, doxazosin pretreatment, on average, reduced MDMA-induced increases in mean arterial pressure (MAP), despite enhancing circulating NE and tachycardia. Doxazosin pretreatment also attenuated MDMA-induced heightened mood ratings as predicted, and moderately attenuated increased body temperature. Self-reported adverse effects and mydriasis from MDMA were not significantly affected by doxazosin pretreatment ( Hysek and Liechti 2012 ).
Antipsychotics & MDMA
One RCT was identified that combined MDMA with an antipsychotic ( Liechti and Vollenweider 2000b ). Researchers hypothesized that the D 2 antagonism effects of haloperidol (1.4 mg i.v.) would attenuate some of the stimulant-like effects of MDMA (1.5 mg/kg p.o.). No changes were observed in MDMA-induced cardiovascular or thermogenic effects, nor responsiveness to startle ( Liechti et al. 2001 ). In contrast to their hypothesis, this drug combination resulted in reduced well-being, reduced “oceanic boundlessness”, and a higher rate of state anxiety. Overall, researchers noted an alteration in the psychological profile of MDMA’s usually pleasurable state to a dysphoric one.
Bupropion & MDMA
Schmid et al. (2015) studied the combination of bupropion XR (titrated to 300 mg p.o. over 7 days) with MDMA (125 mg p.o. administered concurrently with bupropion XR 300 mg on day 7). The researchers hypothesized that DAT and NET blockade by bupropion pretreatment would attenuate the mood and cardiostimulant effects of MDMA. There was a moderate reduction in NE as well as an attenuation in heart rate elevation. No other significant cardiovascular, mydriatic, or hormonal changes occurred compared to MDMA alone. Bupropion did affect self-reported subjective complaints from MDMA, although bupropion significantly prolonged the positive mood effects of MDMA. There was an increase in MDMA levels and reduction in the primary metabolites, DHMA and HMMA, suggesting inhibition of CYP2D6 by bupropion ( Steuer et al. 2016 ). There was also reduction in MDA levels, suggesting inhibition of CYP2B6 by bupropion ( Steuer et al. 2016 ). MDMA increased bupropion levels when co-administered due to MDMA’s autoinhibition of CYP2D6.
Memantine & MDMA
de Sousa Fernandes Perna et al. (2014) studied pretreatment with the NMDA-antagonist memantine (20 mg p.o. 2 h prior) to determine if this would alter MDMA’s (75 mg p.o.) effects on memory and mood. The researchers hypothesized that memantine pretreatment may potentially reverse MDMA-induced memory impairment since this had been demonstrated in animal models. The study determined that memantine pretreatment had no effect on MDMA-induced acute memory impairment or effects on mood.
Psychostimulants & MDMA
Hysek et al. (2014b) conducted an RCT combining MDMA with methylphenidate. Researchers hypothesized that MDMA and methylphenidate may have pharmacodynamic interactions given that they both act on NET and DAT. MDMA and methylphenidate levels and half-lives were unaffected by co-administration; however, researchers found that methylphenidate delayed the time it took for MDMA to reach maximum concentration. The researchers remark this may be due to methylphenidate reducing the absorption of MDMA. There was an increase in circulating epinephrine, heart rate, and rate pressure product. Subjectively, methylphenidate attenuated MDMA’s effect on “happy” affect recognition and increased mental concentration. The co-administration of methylphenidate and MDMA increased acute and subacute subjective complaints. This suggested to researchers that “the combined use of methylphenidate and MDMA would not result in additional psychoactive effects compared with MDMA alone, but such a combination would enhance cardiovascular and adverse effects”.
Serotonin reuptake inhibitors & MDMA
Given that MDMA increases intrasynaptic 5HT, partially by inhibiting SERT, researchers hypothesized that the SERT-blocking effects of SSRIs carry the potential for pharmacodynamic interactions when co-administered with MDMA. In addition, several SSRIs are also substrates or inhibitors of cytochrome P450 enzymes, which may result in pharmacokinetic interactions with MDMA. Three primary RCTs, and four additional analyses of exploratory outcomes from the primary RCTs, have been published looking at the combination of MDMA with citalopram ( Liechti 2000 ; Liechti and Vollenweider 2000a ; Liechti et al. 2001 ) fluoxetine ( Tancer and Johanson 2006 ) and paroxetine ( Farré et al. 2007 ; Pacifici et al. 2004 ; Segura et al. 2005 ). All three SSRIs attenuated the subjective effects of MDMA by ~ 30– ~ 80%, while physiological effects were attenuated by ~ 6– ~ 14% (with the exception of paroxetine, which was on the order of ~ 40– ~ 60%). Both fluoxetine and paroxetine are strong inhibitors of CYP2D6, and plasma concentrations of MDMA were increased despite the effects of MDMA being attenuated. Exploratory studies demonstrated that paroxetine both blunted MDMA-induced immunosuppression, especially cytokine release ( Pacifici et al. 2004 ), and may interact with multiple cytochrome P450 enzymes involved in MDMA metabolism ( Segura et al. 2005 ).
Hysek et al. (2012d) studied the effect of duloxetine, an SNRI, on MDMA because of its potent inhibition of both SERT and NET, without substantial activity at DAT. Compared to MDMA alone, the addition of duloxetine reduced circulating NE and attenuated MDMA-induced increases in heart rate and blood pressure. There was a near complete elimination of MDMA’s effects on the pupillary light reflex ( Hysek and Liechti 2012 ). Exploratory hormone measures with female participants found that MDMA-induced elevations in copeptin were reduced by duloxetine, while there was no significant change in males ( Simmler et al. 2011 ). Subjectively, many of MDMA’s effects, including those on mood—such as well-being, extroversion, closeness, openness, as well as alterations in consciousness—were significantly reduced by duloxetine. Participants given MDMA alone had 5.56 more acute complaints than baseline, while duloxetine co-administered with MDMA resulted in having less acute and subacute complaints than their pre-drug baseline. These reductions of MDMA’s pharmacodynamic, physiological, and subjective effects occurred despite increased MDMA plasma levels due to CYP2D6 inhibition by duloxetine, suggesting that pharmacokinetics are not responsible for these attenuating effects.
Reboxetine & MDMA
Hysek et al. (2011) were interested in studying the effects of a NE specific reuptake inhibitor, reboxetine (8 mg p.o.), on MDMA (125 p.o.). Researchers hypothesized that reboxetine inhibition of NET would outcompete MDMA’s effects on NET, resulting in attenuation of MDMA’s effects. Confirming their hypothesis, they found reductions in circulating NE and attenuation of the cardiovascular stimulant effects of MDMA. Subjectively, the addition of reboxetine attenuated MDMA’s psychostimulant properties, such as emotional excitation, feeling “stimulated,” state anxiety, and blissful feelings such as closeness and boundlessness. There were no significant effects on other psychological parameters such as drug “liking” or “good drug effect.” Reboxetine reduced MDMA-induced acute and subacute complaints, such as tremor and restlessness. These attenuations in MDMA’s effects occurred despite increased plasma MDMA, likely due to reboxetine’s CYP2D6 inhibition. E x vivo plasma examination showed that reboxetine co-administered with MDMA reduced NET binding and had no effect on SERT or DAT binding.
Antipsychotics & psilocybin
RCTs were conducted combining psilocybin with three antipsychotics: chlorpromazine, haloperidol, and risperidone. An early study co-administered the typical antipsychotic chlorpromazine (50 mg p.o), which antagonizes both D 2 and 5HT 2A receptors, with psilocybin (0.2 mg/kg p.o.), resulting in attenuation in psilocybin-induced mydriasis and visual perceptual changes ( Keeler 1967 ). Vollenweider et al. (1998) examined the role of the D 2 antagonist haloperidol (0.021 mg/kg i.v.) and the mixed 5 HT 2A /D 2 antagonist risperidone (0.5 mg p.o., 1 mg p.o.) when separately combined with psilocybin (0.25 mg/kg p.o.). In contrast to risperidone, haloperidol had no effects on psilocybin-induced perceptual changes but did increase the “dread of ego dissolution” parameter of the Altered States of Consciousness (APZ-OAV) scale. Risperidone reduced all the parameters of the APZ-OAV, demonstrating attenuation in psilocybin-induced alterations in consciousness, including a reduction in dread of ego dissolution. Working memory was tested using the delayed-response task, where a brief visual stimulus is presented then withdrawn, and after a several second delay, the participant is asked to identify the location of the visual stimulus. Psilocybin alone delayed reaction time during its peak effects, though co-administration with risperidone attenuated the delay in reaction time.
Serotonin agonists & psilocybin
We found only one RCT combining psilocybin with serotonin agonists ( Pokorny et al. 2016 ). Due to psilocybin’s binding affinity for 5-HT 1A and 5-HT 2A , the researchers independently examined the effects of combining psilocybin (170 μg/kg p.o.) with buspirone (20 mg p.o.) or ergotamine (3 mg p.o.), both of which have 5-HT 1A and 5-HT 2A affinity. It was found that buspirone reduced visionary restructuralization, a subscale of the 5-Dimensions of Altered States of Consciousness Rating Scale (5D-ASC). This suggests that buspirone attenuated psilocybin-induced visual perceptual changes. Ergotamine had no effect on psilocybin-induced subjective effects, perhaps due to different functional selectivity profiles at these receptors.
Serotonin reuptake inhibitors & psilocybin
To date, there has been only one RCT combining psilocybin with an SSRI ( Becker et al. 2021 ). Participants were titrated to 20 mg of escitalopram over 14 days and then administered one dose of psilocybin (25 mg p.o., day 14) 2 h after final escitalopram administration. Due to prior case reports on SSRI-induced attenuation of the effects of LSD ( Bonson 1996 ; Strassman 1992 ) researchers hypothesized a significant reduction in the subjective effects of psilocybin. Contrary to their hypothesis, escitalopram pretreatment did not significantly attenuate ratings of altered states of consciousness from psilocybin. Escitalopram pretreatment was associated with significant reductions in subjective ratings of bad drug effects, fear, talkativeness, openness, anxiety, ineffability, and global adverse effects. Physiologically, escitalopram pretreatment also significantly attenuated psilocybin-induced elevations in blood pressure and pupil dilation. Psilocybin alone did not alter the QTc interval and its co-administration with escitalopram had no effect on QTc. Escitalopram did not alter levels of psilocin.
Epidemiologic studies
Cohen et al. (2021) conducted a post-marketing surveillance association study that was hand-selected by the authors for inclusion in this systematic review as it was published shortly after the initial Pubmed query, met inclusion criteria, and is clinically relevant. Researchers analyzed 946 unique recreational ecstasy use reports from the FDA Adverse Event Reporting System (FAERS) database from 2000–2020. The mean age of the mostly male (70.1%) sample was 28 years. Several concomitant drug class ingestions were associated with an increased multivariate adjusted odds ratios of death: MDMA metabolites or analogs [aOR 8.71], muscle relaxants [aOR 8.17], anesthetics [aOR 7.13], amphetamines and stimulants [aOR 3.05], benzodiazepines [aOR 2.25], opioids [2.05], ethanol [2.03], and antidepressants [aOR 1.62]. Five psychiatric medications analyzed individually demonstrated increased univariate unadjusted odds ratios of death: bupropion [OR 2.82], sertraline [OR 2.36], venlafaxine [OR 1.97], citalopram [OR 1.92], and olanzapine [OR 1.86]. All 18 reported cases of metoclopramide resulted in death. Risperidone and lithium odds ratios were incalculable due to no fatal cases.
Copeland et al. (2006) conducted a cross-sectional survey study of 216 adults who co-ingested ecstasy and a pharmaceutical drug within the previous 6 months. The mean age of the participants was 26 years, mostly male (63%), with an average of 11 days of ecstasy use in the prior 6 months. 28% of the participants intentionally co-ingested a pharmaceutical drug to augment the effects of ecstasy, in particular sildenafil (77% reported use was to gain or maintain an erection) and benzodiazepines. 76% of participants who concomitantly used ecstasy and antidepressants still experienced euphoria; however, they experienced higher rates of adverse effects, including: muscle rigidity (0% vs 45%), nystagmus (0% vs 33%), dizziness (19% vs 42%), headache (21% vs 62%, and profuse sweating (28% vs 53%). Notably, antidepressants were not analyzed based on pharmacologic class and included MAOIs which may have contributed to the frequency of the aforementioned adverse effects.
Nayak et al. (2021) conducted an epidemiologic quantitative analysis, which was hand-selected by the authors as it was pre-published online shortly after the initial PubMed query and met inclusion criteria. Analysis of 96 first- or second-person accounts posted online (i.e., Erowid, the Shroomery, and Reddit) involving co-ingestion of a psychedelic and a mood stabilizer (i.e., lithium, lamotrigine, valproic acid, carbamazepine, and oxcarbazepine). The researchers looked at numerous psychedelic substances, including psilocybin, however most reports involved lysergic acid diethylamide (LSD), another “classic psychedelic.” Of the mood stabilizers, there was only data on lamotrigine and lithium being co-ingested with psilocybin. They found that 2 of the 6 reports of lithium plus psilocybin resulted in seizures. None of the 10 reports of lamotrigine plus psilocybin resulted in seizures. “Low quality evidence due to lack of standardization, selection bias, and lack of clinical verification” was acknowledged by the study authors.
To our knowledge, this is the first systematic review of drug-drug interactions between psychiatric medications and MDMA or psilocybin. Forty publications met our inclusion criteria, including 22 RCTs of MDMA administered with and without a psychiatric medication and 4 RCTs of psilocybin administered with and without a psychiatric medication. Cumulatively, these clinical trials included over 200 participants. We also identified 3 epidemiologic studies: one large cross-sectional survey, one large post-marketing surveillance association study involving ecstasy co-ingestion with medications, and one quantitative analysis of online “trip reports.”
This review demonstrates that the existing data on drug-drug interactions between a psychiatric medication and MDMA or psilocybin predominantly pertains to MDMA. There are only 2 studies on psilocybin captured in this review that were published within the last decade, highlighting a limited body of scientific literature related to drug-drug interactions with psilocybin. It is important to note that the clinical trials in this review were primarily designed to ascertain the mechanisms of MDMA or psilocybin. Therefore, all the study participants were young healthy adults who were either administered a psychiatric medication only once or, rarely, over several days for a maximum of 14 days ( Becker et al. 2021 ). Therefore, these studies are limited in their extrapolation to real world clinical settings where psychiatric medications are often taken daily for months or years. Other factors that limit the extrapolation of these studies to clinical settings is that some studies instituted less common routes of administration of psychiatric medications, such as intravenous haloperidol ( Vollenweider et al. 1998 ) or intravenous citalopram ( Liechti and Vollenweider 2000a ). Some studies had unique exclusion criteria that may limit the generalizability of outcomes further, such as high levels of neuroticism ( Liechti and Vollenweider 2000a , 2000b )—which recently has been shown to predict negative psychological responses to MDMA ( Studerus et al. 2021 )—or inclusion of only individuals with prior recreational ecstasy use ( Farré et al. 2007 ; Tancer and Johanson 2006 ).
MDMA psychopharmacology
Pharmacokinetic interactions—mdma.
MDMA’s pharmacokinetics are complex, involving several cytochrome P450 enzymes, which makes MDMA particularly susceptible to drug-drug interactions with strong pan-CYP inhibitors like ritonavir—which has resulted in significant toxicity ( Papaseit et al. 2012 ). Many psychiatric medications have significant inhibitory effects on CYP2D6, and it is also an enzyme that displays a wide range in metabolic capacity throughout the population ( Bertilsson et al. 2002 ). The studies included in this review had numerous instances of CYP2D6 interactions with MDMA including paroxetine, fluoxetine, duloxetine, reboxetine, and bupropion.
Pharmacodynamic interactions—MDMA
MDMA’s effects on monoamine transporters, namely SERT and NET, are unique. MDMA acts as a SERT and NET substrate, resulting in reverse transport and exocytotic release of 5HT and NE ( Hilber et al. 2005 ; Verrico et al. 2007 ). In contrast: antidepressants (i.e., SSRIs, SNRIs, NRIs, and NDRIs) capture the monoamine transporter (i.e., SERT, NET, and DAT) in an inhibitor-bound conformation, preventing substrate binding ( Coleman et al. 2016 ; Penmatsa et al. 2013 , 2015 ) and resulting in higher monoamine concentrations in the synaptic cleft.
Researchers primarily from the same laboratory group systematically conducted a series of clinical trials on drug-drug combinations of MDMA with various monoamine reuptake blocking agents to ascertain relative contributions of different monoamine systems to MDMA’s mechanism of action. SERT inhibitors (SSRIs), including citalopram ( Liechti 2000 ; Liechti et al. 2001 ; Liechti and Vollenweider 2000a ), paroxetine ( Farré et al. 2007 ; Pacifici et al. 2004 ; Segura et al. 2005 ), and fluoxetine ( Tancer and Johanson 2006 ), reduce MDMA’s physiological and subjective effects broadly. NET-specific inhibition by reboxetine reduced MDMA’s NE-mediated cardiostimulant properties and some psychological outcomes ( Hysek et al. 2011 ; Hysek and Liechti 2012 ); while combined NET and SERT inhibition by duloxetine broadly attenuated physiological and psychological outcomes, similar to outcomes from SSRI + MDMA combinations ( Hysek et al. 2012d ; Hysek and Liechti 2012 ; Simmler et al. 2011 ). Overall, monoamine reuptake inhibitors resulted in attenuation of MDMA’s physiological and subjective effects, even in instances of higher MDMA plasma levels by means of CYP2D6 inhibition. This consistent outcome may suggest that, when administered together, monoamine reuptake inhibitors outcompete MDMA by binding to monoamine transporters (i.e., SERT, NET, DAT), preventing the efflux of monoamines into the synaptic cleft, thus attenuating the effects of MDMA. Exceptions to this trend include the combined NET and DAT inhibitor, bupropion, which prolonged the subjective effects and heightened the positive mood effects of MDMA. In this case, CYP2D6 and CYP2B6 pharmacokinetic interactions and bupropion’s relatively low ability to inhibit NET or DAT ( Schmid et al. 2015 ; Steuer et al. 2016 ) may explain this outcome. While no serious adverse effects of these combinations were observed in clinical trial settings, there are risks to combining SSRIs or bupropion with MDMA in uncontrolled settings. For example, a recent large-scale surveillance study of data from the FDA’s Adverse Event Reporting Systems (FAERS) reviewed reports of co-ingestion of MDMA in non-clinical settings with medications, finding that several antidepressant + MDMA combinations increased mortality, with bupropion having the highest odds ratio for death of any antidepressant [OR 2.82] ( Cohen et al. 2021 ). It is plausible that the combination of bupropion and MDMA increases the risk of seizures, stimulant toxicity, or serotonin syndrome given that both drugs are stimulants capable of lowering seizure thresholds and that they increase blood concentrations of each other when taken together.
Relevant to the co-administration of monoamine reuptake inhibitors and MDMA, there has been ongoing attention paid to the risk of serotonin syndrome with the combination of SSRIs and MDMA, theorized to be related to a rise of 5HT in the central nervous system ( Copeland et al. 2006 ; Dobry et al. 2013 ). The RCTs in this review show attenuation of MDMA’s physiological effects, suggesting a reduced odds of serotonin syndrome, at least with acute SSRI dosing. This is corroborated by at least one other scientific review positing SSRIs, SNRIs, and TCAs are not likely to increase serotonin to life-threatening toxicity when combined with MDMA ( Silins et al. 2007 ). This may be due to the fact that MDMA’s reversal of monoamine transporters is negated by the inhibition of monoamine transporters by most antidepressants; therefore, there is not an increase in intrasynaptic serotonin which is the hallmark mechanism for serotonin toxicity to occur. A notable downside of SSRI or SNRI use in conjunction with MDMA is attenuation of subjective effects and the potential for reduced MAP treatment efficacy ( Hysek et al. 2012d ; Feduccia et al. 2020 ). However, discontinuation of psychiatric medications poses a risk of antidepressant discontinuation syndromes or relapse of psychiatric symptoms that must be weighed in clinical decision-making by the prescribing provider. An important outlier when it comes to serotonergic agents and MDMA is the MAOI class. MAOIs prevent breakdown of monoamines and, when combined with MDMA, result in dangerous elevations in intrasynaptic serotonin. This has contributed to the majority of deaths cited in published case studies (see summary of case studies in Supplementary Materials ).
Stimulants have been proposed to induce exocytotic release of monoamines via DAT and NET, similar to MDMA ( Fleckenstein and Hanson 2003 ), or to only inhibit DAT and NET reuptake similar to methylphenidate ( Hysek et al. 2014a , b ). In fact, the combination of methylphenidate and MDMA resulted in synergistic effects: higher rates of self-reported complaints and heightened cardiostimulant effects ( Hysek et al. 2014a , b ). Dopamine blockade via co-administration of haloperidol did not alter MDMA’s physiological effects ( Liechti and Vollenweider 2000b ), which is unsurprising given MDMA’s limited impact on the dopamine system. However, it is intriguing that MDMA’s typically euphoric effects were absent, while trait anxiety and dysphoria were exaggerated, potentially related to haloperidol’s dysphoric effects.
Regarding adrenergic agents and MDMA: carvedilol ( Hysek et al. 2012c ) dramatically reduced MDMA-induced cardiostimulant and hyperthermic effects without influencing MDMA’s psychological effects, while clonidine and doxazosin had a minimal effect on physiology ( Hysek et al. 2012a ; Hysek et al. 2013 ). It is not fully clear if combining an adrenergic agent with MDMA reflects additive effects or a pharmacodynamic interaction. The notion of additive effects is supported by the fact that carvedilol ( Hysek et al. 2012c ), pindolol ( Hysek et al. 2010 ), and clonidine ( Hysek et al. 2012a ) reduced adrenergic activity but did not significantly alter the subjective effects of MDMA ( Hasler et al. 2009 ; Hysek et al. 2010 , 2012a , c ). However, doxazosin is an outlier as it attenuated attenuated MDMA’s mood heightening effects ( Hysek et al. 2013 ). Doxazosin also increased MDMA-induced tachycardia which may be a result of its α 1 specific blockade resulting in compensatory activation of other α- and β-adrenoreceptors as described elsewhere in the literature ( Richards et al. 2017 ). Regardless, the interaction between adrenergic agents and MDMA would be a valuable area of additional research, as well as clinically useful information in choosing an antihypertensive or antipyretic to address MDMA-related adverse effects in the setting of MAP treatment without compromising the potentially beneficial affective effects of MDMA.
Pharmacogenetics & MDMA
It has been demonstrated that CYP2D6 poor metabolizers carrying only *3, *4, or *5 alleles administered MDMA reached an average maximum concentration (C max ) that is 19% higher and an initial drug exposure (AUC 0–6 h ) that is 25% higher than extensive metabolizers carrying only *1 and *2 alleles, which corresponded to a more rapid onset of subjective effects and elevated blood pressure ( Schmid et al. 2016 ). Recent pooled RCT data demonstrated that the physiological and psychological effects of MDMA were most strongly dependent on plasma concentration, while higher activity scores for CYP2D6 metabolizer status predicted a lower MDMA plasma concentration ( Studerus et al. 2021 ).
Psilocybin psychopharmacology
Pharmacokinetic interactions—psilocybin.
Compared to MDMA, psilocybin is less likely to contribute to pharmacokinetic drug-drug interactions given that its metabolic pathway predominantly involves UGT1A10 and UGT1A9 ( Manevski et al. 2010 ). Diclofenac and probenecid are examples of UGT1A9/10 inhibitors that may hypothetically alter psilocybin metabolism if co-ingested; however, there is no evidence to confirm this hypothesis beyond shared metabolism. There are few pharmacologic agents that influence UGT1A9 and UGT1A10 ( Liu et al. 2011 ). Furthermore, the pharmacokinetics of psilocin, the active metabolite of psilocybin, is linear and is minimally affected by renal clearance ( Brown et al. 2017 ).
Pharmacodynamic interactions—psilocybin
Research into drug interactions with psilocybin is sparse yet paints an interesting picture of its mechanism. When 5 HT 2A is blocked pharmacologically, such as by buspirone ( Pokorny et al. 2016 ; Bonhaus et al. 1997 ), chlorpromazine ( Keeler 1967 ), ketanserin, or risperidone ( Vollenweider et al. 1998 ), there is a consistent pattern of attenuation of psilocybin’s subjective effects. However, 5HT 2A and 5HT 1A agonism, such as from ergotamine ( Pokorny et al. 2016 ) does not seem to have an effect on psilocybin nor LSD’s subjective effects ( Mattusek and Halbach 1964 ). D 2 antagonism alone, in the case of haloperidol, does not attenuate psilocybin’s effects, and, in fact, exacerbates anxiety and produces dysphoria ( Vollenweider et al. 1998 ). Interestingly, when blocking SERT pharmacologically with escitalopram ( Becker et al. 2021 ), there is no attenuation of psilocybin’s psychedelic effects and in fact reduced measures of anxious distress and participant complaints. Collectively, this data points towards psilocybin’s unique mechanism of action which is contingent on direct serotonin receptor agonism that does not compete nor rely on SERT activity. We would hypothesize that other SERT blockers, such as sertraline, in combination with psilocybin would reproduce similar findings as Becker et al. (2021) while 5HT 2A blockade would attenuate psilocybin’s effects, both subjectively and physiologically.
Trends in case studies
We identified 11 case study manuscripts ( Akhondzadeh and Hampa 2005 ; Bingham 1998 ; Delgado et al. 2004 ; Kaskey 1992 ; Lauerma et al. 1998 ; McCann and Ricaurte 1993 ; Pilgrim et al. 2012 ; Ramcharan et al. 1998 ; Smilkstein et al. 1987 ; Stein and Rink 1999 ; Vuori et al. 2003 ), all of which involve the recreational ingestion of ecstasy and provide helpful insights on the implications of co-ingestion in the context of illicit use. However, these data are limited by the inability to ascertain drug levels of MDMA or other potential adulterants in most cases; therefore, case studies are described in Supplemental Materials . These case studies reveal a trend that the highest rates of morbidity occurred from the combination of MDMA with MAOIs, such as moclobemide or phenelzine. A number of these cases involved significant hyperthermia, seizure-like activity, and altered mental status, suggestive of unrecognized symptoms of serotonin syndrome, many of which resulted in fatality. In several cases, coronary artery disease was noted upon autopsy and was a suggested risk factor in the cause of death. In one notable case of a young man with bipolar disorder prescribed moclobemide and lithium who ingested ecstasy, the symptoms of serotonin syndrome were misattributed by his peers to a “psychotic episode” whereupon he was left unaccompanied for 4 h and after which he was found deceased ( Pilgrim et al. 2012 ). The combination of SSRIs with ecstasy in case reports are consistent with lab data, suggesting attenuation of MDMA’s effects. However, the attenuated subjective effects of MDMA from SSRIs may drive individuals to take escalating drug doses to achieve effects, resulting in the elevated odds-ratio for mortality observed by Cohen et al. (2021) ) in instances of concomitant MDMA use with SSRIs.
Limitations
This review focuses on MDMA and psilocybin, thus did not include literature on other psychedelic substances, such as: lysergic acid diethyladmide (LSD), ayahuasca or N, N-demethyltryptamine (DMT), mescaline, or designer drugs. Ketamine can be used in combination with psychotherapy for its psychedelic effects ( Dore et al. 2019 ); we included ketamine in our search as an antidepressant rather than a psychedelic, but did not find any literature on interaction with MDMA or psilocybin. We also did not include the effects of repeated dosing of MDMA ( Farré et al. 2004 ; Peiró et al. 2013; Farré et al. 2015) or psilocybin on subsequent effects. Additionally, our scope was limited to psychiatric medications rather than other medications that may have the propensity for drug-drug interactions with MDMA and psilocybin. Although this review attempts to capture all relevant clinical data to date on co-administration of a psychiatric medication with MDMA or psilocybin, the window of permissible scientific study on psychedelics has been narrow in comparison to groups who have implemented psychedelics into their cultural and spiritual practices for longer than psychiatric medications have been around (e.g., the Mazatec people of Oaxaca) or in comparison to other forms of collective knowledge (e.g., the Erowid Experience Vaults).
Considerations for future research
Modern research protocols for MAP and PAP have either excluded participants taking psychiatric medications or discontinued psychiatric medications prior to administration of MDMA or psilocybin. Tapering psychiatric medications before MAP or PAP poses unique challenges and vulnerabilities to those suffering from psychiatric illnesses by way of increased risk of illness relapse, serotonin discontinuation syndrome, and reduced treatment efficacy ( Feduccia et al. 2020 ). It is apparent that developing optimal strategic approaches for patients who may benefit from MAP or PAP, but are currently prescribed psychiatric medications, will require additional clinical research. In particular, there is a dearth of studies on psilocybin drug-drug interactions, signaling a need for additional research on how psychiatric medications and psilocybin interact. Additionally, of the psilocybin RCTs in this review, none included measures of physiological outcomes. Additional studies of psilocybin drug-drug interactions are pending completion, including a cross-sectional online survey being conducted by the Johns Hopkins Center for Psychedelic and Consciousness Research investigating psilocybin mushrooms taken with antidepressants ( https://hopkinspsychedelic.org/adsurvey ).
Certain groups have been excluded from the clinical trial samples described in this systematic review, including those with particular psychiatric symptoms or medical illnesses such as uncontrolled hypertension, cardiovascular disease, and liver disease. It remains unclear how to safely administer MAP or PAP to medically ill individuals, including individuals with hepatic impairment that would affect drug metabolism. At this time, research is underway to ascertain how hepatic impairment may affect MDMA’s pharmacokinetics ( {"type":"clinical-trial","attrs":{"text":"NCT03606538","term_id":"NCT03606538"}} NCT03606538 ), which is an FDA requirement for drug development and may broaden inclusion in future studies. Additionally, none of the included studies reported on the race or ethnicity of participants nor commented on the inclusion of sexual or gender minorities. This corresponds to the lack of diverse participants in MAP and PAP clinical trials ( Fogg et al. 2021 ). Additionally, there is evidence that estradiol up-regulates expression of UGT1A9 resulting in increased glucuronidation of UGT1A9 substrates ( Cho et al. 2016 ). This suggests that hormone replacement therapy, oral contraceptives, and cyclical hormonal changes may affect the metabolism of psilocybin, highlighting the need for more inclusive research.
There are a number of psychiatric medications commonly used in the management of acute psychological distress sometimes experienced acutely with MDMA or psilocybin administration. Benzodiazepines have been suggested by guidelines, informed by research on management of LSD-related psychological distress, to address extremely challenging psychedelic experiences that don’t respond to behavioral interventions ( Johnson et al. 2008 ). We did not find any studies on the concomitant use of benzodiazepines with MDMA nor psilocybin. In fact, Cohen et al. (2021) found that, among several other drug class co-ingestions with recreational MDMA, benzodiazepines were associated with an increased multivariate adjusted odds ratio of death—higher than that of co-ingested opioids, ethanol, or antidepressants. Online communities have encouraged using olanzapine as a “trip terminator”; in other words, a pharmacologic technique for self-management of psychedelic crises ( Valeriani et al. 2015 ). However, it remains unclear if atypical antipsychotics would be an appropriate approach to manage psychological distress related to MDMA or psilocybin. Recent data from Cohen et al. (2021) demonstrated that olanzapine had an increased univariate unadjusted odds ratio of death among adverse reports of MDMA co-ingestion, while there were no cases of death with risperidone co-ingestion. It is notable that the study by Cohen et al. (2021) was in regards to unregulated ecstasy use in uncontrolled non-clinical settings. The absence of clinical trials on the combination of benzodiazepines or atypical antipsychotics with MDMA, and mixed data regarding heightened risk with psilocybin, suggest that it would be valuable to investigate these drug-drug interactions in future research.
The mechanism in which MAP or PAP lead to psychiatric recovery remains unclear as is the mechanism in which psychiatric drugs affect MAP or PAP outcomes. Of the current body of literature, 5HT 2A serotonin receptor modulation ( Carhart-Harris and Nutt 2017 ), changes in resting state functional connectivity in the default mode network ( Carhart-Harris et al. 2014 ; Müller et al. 2021 ; Roseman et al. 2014 ), and neuroplasticity ( Artin et al. 2021 ; Harmer et al. 2017 ) are among some of the prevailing hypotheses. Whether or not combinations of psychiatric medications with MDMA or psilocybin would interfere with these processes specifically has not been studied. However, there are surprising results from a sub-analysis of pooled Phase 2 MAP studies demonstrating that participants who recently tapered off of prescription antidepressants (e.g. SSRIs, SNRIs, etc.) had a higher PTSD symptom burden and were more likely than the non-taper group to still meet PTSD criteria at the primary study endpoint (63.6% vs. 25.0%), despite completing the taper by an average of 25.1 days before their first MDMA administration session ( Feduccia et al. 2020 ). This suggests that mechanisms beyond direct and immediate pharmacodynamic interactions may have an influence on how drug-drug interactions affect MAP and PAP outcomes. It would be valuable to further study how lifelong psychiatric medication adherence or enduring psychedelic use would affect MAP or PAP outcomes.
As MDMA and psilocybin continue to move through the FDA drug development process, this systematic review offers a compilation of existing research on psychiatric drug-drug interactions with MDMA or psilocybin. There are clear acute pharmacokinetic and pharmacodynamic interactions between many common psychiatric medications and MDMA or psilocybin which affect their physiological and subjective effects and help us better understand the mechanisms of action of these substances. However, the existing body of literature is not readily applicable to the clinical setting, prompting the need for additional research on the topic of drug-drug interactions with MDMA or psilocybin.
Supplementary Material
Supplementary, acknowledgements.
The authors thank Paul Bonney and Jason Jarria for assisting in abstract review. Salary support for CSS provided by the Department of Veterans Affairs, Clinical Science Research & Development, Federal Award Identification Number IK2CX001495.
Declarations
Conflict of interest CSS has received payment from the MAPS Public Benefit Corporation for Training clinicians in MAP. BM runs www.spiritpharmacist.com , which offers a monthly membership service for access to drug interactions guides, courses, and consultation services. AS and KT have no conflicts of interest to report.
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s00213-022-06083-y .
- Abraham TT, Barnes AJ, Lowe RH, Spargo EAK, Milman G, Pirnay SO, Gorelick DA, Goodwin RS, Huestis MA (2009) Urinary MDMA, MDA, HMMA, and HMA Excretion Following Controlled MDMA Administration to Humans . J Anal Toxicol 33 ( 8 ):439–446 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Akhondzadeh S, Hampa AD (2005) Topiramate prevents ecstasy consumption: A case report. Fundam Clin Pharmacol 19 ( 5 ):601–602. 10.1111/j.1472-8206.2005.00355.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Artin H, Zisook S, Ramanathan D (2021) How do serotonergic psychedelics treat depression: The potential role of neuroplasticity . World J Psychiatr 11 ( 6 ):201–214. 10.5498/wjp.v11.i6.201 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baggott MJ, Kirkpatrick MG, Bedi G, de Wit H (2015) Intimate insight: MDMA changes how people talk about significant others . J Psychopharmacol 29 ( 6 ):669–677. 10.1177/0269881115581962 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barrett FS, Bradstreet MP, Leoutsakos JMS, Johnson MW, Griffiths RR (2016) The Challenging Experience Questionnaire: Characterization of challenging experiences with psilocybin mushrooms . J Psychopharmacol 30 ( 12 ):1279–1295 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barrett FS, Griffiths RR (2018) Classic Hallucinogens and Mystical Experiences: Phenomenology and Neural Correlates . Curr Top Behav Neurosci 36 :393–430. 10.1007/7854_2017_474 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Battaglia G, Brooks BP, Kulsakdinun C, De Souza EB (1988) Pharmacologic profile of MDMA (3,4-methylenedioxymethamphetamine) at various brain recognition sites . Eur J Pharmacol 149 ( 1–2 ):159–163. 10.1016/0014-2999(88)90056-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baylen CA, Rosenberg H (2006) A review of the acute subjective effects of MDMA/ecstasy . Addiction 101 ( 7 ):933–947. 10.1111/j.1360-0443.2006.01423.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Becker AM, Holze F, Grandinetti T, Klaiber A, Toedtli VE, Kolaczynska KE, Duthaler U, Varghese N, Eckert A, Grünblatt E, Liechti ME (2021) Acute Effects of Psilocybin After Escitalopram or Placebo Pretreatment in a Randomized, Double-Blind, Placebo-Controlled, Crossover Study in Healthy Subjects . Clin Pharmacol Ther n/a ( n/a ). 10.1002/cpt.2487 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bertilsson L, Dahl M-L, Dalén P, Al-Shurbaji A (2002) Molecular genetics of CYP2D6: Clinical relevance with focus on psychotropic drugs: Molecular genetics of CYP2D6 . Br J Clin Pharmacol 53 ( 2 ):111–122. 10.1046/j.0306-5251.2001.01548.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bigler MB, Egli SB, Hysek CM, Hoenger G, Schmied L, Baldin FS, Marquardsen FA, Recher M, Liechti ME, Hess C, Berger CT (2015) Stress-Induced In Vivo Recruitment of Human Cytotoxic Natural Killer Cells Favors Subsets with Distinct Receptor Profiles and Associates with Increased Epinephrine Levels . PLoS ONE 10 ( 12 ):e0145635. 10.1371/journal.pone.0145635 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bingham C (1998) Necrotizing renal vasculopathy resulting in chronic renal failure after ingestion of methamphetamine and 3,4-methylenedioxymethamphetamine (‘ecstasy’) . Nephrol Dial Transplant 13 ( 10 ):2654–2655. 10.1093/ndt/13.10.2654 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blier P, Ward HE, Tremblay P, Laberge L, Hébert C, Bergeron R (2010) Combination of Antidepressant Medications From Treatment Initiation for Major Depressive Disorder: A Double-Blind Randomized Study . Am J Psychiatry 167 ( 3 ):281–288. 10.1176/appi.ajp.2009.09020186 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bogen IL, Haug KH, Myhre O, Fonnum F (2003) Short- and long-term effects of MDMA (“ecstasy”) on synaptosomal and vesicular uptake of neurotransmitters in vitro and ex vivo . Neurochem Int 43 ( 4–5 ):393–400. 10.1016/S0197-0186(03)00027-5 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bogenschutz MP, Forcehimes AA, Pommy JA, Wilcox CE, Barbosa P, Strassman RJ (2015) Psilocybin-assisted treatment for alcohol dependence: A proof-of-concept study . J Psychopharmacol 29 ( 3 ):289–299. 10.1177/0269881114565144 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bonhaus DW, Weinhardt KK, Taylor M, Desouza A, Mcneeley PM, Szczepanski K, Fontana DJ, Trinh J, Rocha CL, Dawson MW, Flippin LA, Eglen RM (1997) RS-102221: A Novel High Affinity and Selective, 5-HT 2C Receptor Antagonist . Neuropharmacology 36 ( 4–5 ):621–629. 10.1016/S0028-3908(97)00049-X [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bonson K (1996) Chronic Administration of Serotonergic Antidepressants Attenuates the Subjective Effects of LSD in Humans . Neuropsychopharmacology 14 ( 6 ):425–436. 10.1016/0893-133X(95)00145-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Borowiak KS, Ciechanowski K, Waloszczyk P (1998) Psilocybin mushroom (Psilocybe semilanceata) intoxication with myocardial infarction . J Toxicol Clin Toxicol 36 ( 1–2 ):47–49. 10.3109/15563659809162584 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown RT, Nicholas CR, Cozzi NV, Gassman MC, Cooper KM, Muller D, Thomas CD, Hetzel SJ, Henriquez KM, Ribaudo AS, Hutson PR (2017) Pharmacokinetics of Escalating Doses of Oral Psilocybin in Healthy Adults . Clin Pharmacokinet 56 ( 12 ):1543–1554. 10.1007/s40262-017-0540-6 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carhart-Harris R, Giribaldi B, Watts R, Baker-Jones M, Murphy-Beiner A, Murphy R, Martell J, Blemings A, Erritzoe D, Nutt DJ (2021) Trial of Psilocybin versus Escitalopram for Depression . N Engl J Med 384 ( 15 ):1402–1411. 10.1056/NEJMoa2032994 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carhart-Harris R, Leech R, Hellyer PJ, Shanahan M, Feilding A, Tagliazucchi E, Chialvo DR, Nutt D (2014) The entropic brain: A theory of conscious states informed by neuroimaging research with psychedelic drugs . Front Hum Neurosci 8 . 10.3389/fnhum.2014.00020 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carhart-Harris R, Nutt D (2017) Serotonin and brain function: A tale of two receptors . J Psychopharmacol 31 ( 9 ):1091–1120. 10.1177/0269881117725915 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carpenter LL, Yasmin S, Price LH (2002) A double-blind, placebo-controlled study of antidepressant augementation with mirtazapine . Biol Psychiat 51 ( 2 ):183–188. 10.1016/S0006-3223(01)01262-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Castro Santos H, Gama Marques J (2021) What is the clinical evidence on psilocybin for the treatment of psychiatric disorders? A Systematic Review Porto Biomedical Journal 6 ( 1 ):e128. 10.1097/j.pbj.0000000000000128 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Center for Behavioral Health Statistics and Quality (2020) National Survey on Drug Use and Health—2019 . Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/ [ PubMed ] [ Google Scholar ]
- Cho S, Ning M, Zhang Y, Rubin LH, Jeong H (2016) 17β-Estradiol up-regulates UDP-glucuronosyltransferase 1A9 expression via estrogen receptor α . Acta Pharmaceutica Sinica B 6 ( 5 ):504–509. 10.1016/j.apsb.2016.04.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen IV, Makunts T, Abagyan R, Thomas K (2021) Concomitant drugs associated with increased mortality for MDMA users reported in a drug safety surveillance database . Sci Rep 11 ( 1 ):5997. 10.1038/s41598-021-85389-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coleman JA, Green EM, Gouaux E (2016) X-ray structures and mechanism of the human serotonin transporter . Nature 532 ( 7599 ):334–339. 10.1038/nature17629 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Copeland J, Dillon P, Gascoigne M (2006) Ecstasy and the concomitant use of pharmaceuticals . Addict Behav 31 ( 2 ):367–370. 10.1016/j.addbeh.2005.05.025 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Danforth AL, Grob CS, Struble C, Feduccia AA, Walker N, Jerome L, Yazar-Klosinski B, Emerson A (2018) Reduction in social anxiety after MDMA-assisted psychotherapy with autistic adults: A randomized, double-blind, placebo-controlled pilot study . Psychopharmacology 235 ( 11 ):3137–3148. 10.1007/s00213-018-5010-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davis AK, Barrett FS, May DG, Cosimano MP, Sepeda ND, Johnson MW, Finan PH, Griffiths RR (2021) Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial . JAMA Psychiat 78 ( 5 ):481–489. 10.1001/jamapsychiatry.2020.3285 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- De Jong J, Wauben P, Huijbrechts I, Oolders H, Haffmans J (2010) Doxazosin treatment for posttraumatic stress disorder . J Clin Psychopharmacol 30 ( 1 ):84–85. 10.1097/JCP.0b013e3181c827ae [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Perna DSF EB, Theunissen EL, Kuypers KP, Heckman P, de la Torre R, Farre M, & Ramaekers JG (2014) Memory and mood during MDMA intoxication, with and without memantine pretreatment . Neuropharmacology 87 :198–205. 10.1016/j.neuropharm.2014.03.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Delgado JH, Caruso MJ, Waksman JC, Honigman B, Stillman D (2004) Acute, transient urinary retention from combined ecstasy and methamphetamine use . J Emerg Med 26 ( 2 ):173–175. 10.1016/j.jemermed.2003.05.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dinis-Oliveira RJ (2017) Metabolism of psilocybin and psilocin: Clinical and forensic toxicological relevance . Drug Metab Rev 49 ( 1 ):84–91. 10.1080/03602532.2016.1278228 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dobry Y, Rice T, Sher L (2013) Ecstasy use and serotonin syndrome: A neglected danger to adolescents and young adults prescribed selective serotonin reuptake inhibitors . Int J Adolesc Med Health 25 ( 3 ):193–199. 10.1515/ijamh-2013-0052 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dore J, Turnipseed B, Dwyer S, Turnipseed A, Andries J, Ascani G, Monnette C, Huidekoper A, Strauss N, Wolfson P (2019) Ketamine Assisted Psychotherapy (KAP): Patient Demographics, Clinical Data and Outcomes in Three Large Practices Administering Ketamine with Psychotherapy . J Psychoactive Drugs 51 ( 2 ):189–198. 10.1080/02791072.2019.1587556 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- English BA, Dortch M, Ereshefsky L, Jhee S (2012) Clinically Significant Psychotropic Drug-Drug Interactions in the Primary Care Setting . Curr Psychiatry Rep 14 ( 4 ):376–390. 10.1007/s11920-012-0284-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Farré M, de la Torre R, Mathúna BO, Roset PN, Peiró AM, Torrens M, Ortuño J, Pujadas M, Camí J (2004) Repeated doses administration of MDMA in humans: pharmacological effects and pharmacokinetics . Psychopharmacology (Berl) 173 ( 3–4 ):364–75 [ PubMed ] [ Google Scholar ]
- Farré M, Abanades S, Roset PN, Peiró AM, Torrens M, O’Mathúna B, Segura M, de la Torre R (2007) Pharmacological Interaction between 3,4-Methylenedioxymethamphetamine (Ecstasy) and Paroxetine: Pharmacological Effects and Pharmacokinetics . J Pharmacol Exp Ther 323 ( 3 ):954–962. 10.1124/jpet.107.129056 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Feduccia AA, Jerome L, Mithoefer MC, Holland J (2020) Discontinuation of medications classified as reuptake inhibitors affects treatment response of MDMA-assisted psychotherapy . Psychopharmacology . 10.1007/s00213-020-05710-w [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Feduccia AA, Mithoefer MC (2018) MDMA-assisted psychotherapy for PTSD: Are memory reconsolidation and fear extinction underlying mechanisms ? Prog Neuropsychopharmacol Biol Psychiatry 84 :221–228. 10.1016/j.pnpbp.2018.03.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fleckenstein AE, Hanson GR (2003) Impact of psychostimulants on vesicular monoamine transporter function . Eur J Pharmacol 479 ( 1 ):283–289. 10.1016/j.ejphar.2003.08.077 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fogg C, Michaels TI, de la Salle S, Jahn ZW, Williams MT (2021) Ethnoracial health disparities and the ethnopsychopharmacology of psychedelic-assisted psychotherapies . Exp Clin Psychopharmacol . 10.1037/pha0000490 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gable RS (2004) Comparison of acute lethal toxicity of commonly abused psychoactive substances . Addiction 99 ( 6 ):686–696. 10.1111/j.1360-0443.2004.00744.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gorman I, Belser AB, Jerome L, Hennigan C, Shechet B, Hamilton S, Yazar-Klosinski B, Emerson A, Feduccia AA (2020) Post-traumatic Growth After MDMA-Assisted Psychotherapy for Posttraumatic Stress Disorder . J Trauma Stress 33 ( 2 ):161–170. 10.1002/jts.22479 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Griffiths RR, Richards WA, Johnson MW, McCann UD, Jesse R (2008) Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later . Journal of Psychopharmacology (oxford, England) 22 ( 6 ):621–632. 10.1177/0269881108094300 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Griffiths RR, Richards WA, McCann U, & Jesse R (2006). Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance . Psychopharmacology , 187 ( 3 ), 268–283 284–292. 10.1007/s00213-006-0457-5 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Grob CS, & Grigsby J (Eds.). (2021). Handbook of medical hallucinogens . The Guilford Press. [ Google Scholar ]
- Grob CS, Poland RE, Chang L, Ernst T (1995) Psychobiologic effects of 3,4-methylenedioxymethamphetamine in humans: Methodological considerations and preliminary observations . Behav Brain Res 73 ( 1 ):103–107. 10.1016/0166-4328(96)00078-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Harmer CJ, Duman RS, Cowen PJ (2017) How do antidepressants work? New perspectives for refining future treatment approaches . The Lancet Psychiatry 4 ( 5 ):409–418. 10.1016/S2215-0366(17)30015-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hasler F, Grimberg U, Benz MA, Huber T, Vollenweider FX (2004) Acute psychological and physiological effects of psilocybin in healthy humans: a double-blind, placebo-controlled dose-effect study . Psychopharmacology (Berl) 172 ( 2 ):145–56 [ PubMed ] [ Google Scholar ]
- Hasler F, Studerus E, Lindner K, Ludewig S, Vollenweider F (2009) Investigation of serotonin-1A receptor function in the human psychopharmacology of MDMA . J Psychopharmacol 23 ( 8 ):923–935. 10.1177/0269881108094650 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hilber B, Scholze P, Dorostkar MM, Sandtner W, Holy M, Boehm S, Singer EA, Sitte HH (2005) Serotonin-transporter mediated efflux: A pharmacological analysis of amphetamines and non-amphetamines . Neuropharmacology 49 ( 6 ):811–819. 10.1016/j.neuropharm.2005.08.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hofmann A, Frey A, Ott H, Petrzilka Th, Troxler F (1958) Konstitutionsaufklärung und Synthese von Psilocybin . Experientia 14 ( 11 ):397–399. 10.1007/BF02160424 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Brugger R, Simmler LD, Bruggisser M, Donzelli M, Grouzmann E, Hoener MC, Liechti ME (2012a) Effects of the α 2 -Adrenergic Agonist Clonidine on the Pharmacodynamics and Pharmacokinetics of 3,4-Methylenedioxymethamphetamine in Healthy Volunteers . J Pharmacol Exp Ther 340 ( 2 ):286–294. 10.1124/jpet.111.188425 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Domes G, Liechti ME (2012b) MDMA enhances “mind reading” of positive emotions and impairs “mind reading” of negative emotions . Psychopharmacology 222 ( 2 ):293–302. 10.1007/s00213-012-2645-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Fink AE, Simmler LD, Donzelli M, Grouzmann E, Liechti ME (2013) Α 1 -Adrenergic receptors contribute to the acute effects of 3,4-methylenedioxymethamphetamine in humans . J Clin Psychopharmacol 33 ( 5 ):658–666. 10.1097/JCP.0b013e3182979d32 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Liechti ME (2012) Effects of MDMA alone and after pretreatment with reboxetine, duloxetine, clonidine, carvedilol, and doxazosin on pupillary light reflex . Psychopharmacology 224 ( 3 ):363–376. 10.1007/s00213-012-2761-6 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Schmid Y, Rickli A, Simmler L, Donzelli M, Grouzmann E, Liechti ME (2012c) Carvedilol inhibits the cardiostimulant and thermogenic effects of MDMA in humans . Br J Pharmacol 166 ( 8 ):2277–2288. 10.1111/j.1476-5381.2012.01936.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Schmid Y, Simmler LD, Domes G, Heinrichs M, Eisenegger C, Preller KH, Quednow BB, Liechti ME (2014a) MDMA enhances emotional empathy and prosocial behavior . Social Cognitive and Affective Neuroscience 9 ( 11 ):1645–1652. 10.1093/scan/nst161 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Simmler LD, Ineichen M, Grouzmann E, Hoener MC, Brenneisen R, Huwyler J, Liechti ME (2011) The Norepinephrine Transporter Inhibitor Reboxetine Reduces Stimulant Effects of MDMA (“Ecstasy”) in Humans . Clin Pharmacol Ther 90 ( 2 ):246–255. 10.1038/clpt.2011.78 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Simmler LD, Nicola VG, Vischer N, Donzelli M, Krähenbühl S, Grouzmann E, Huwyler J, Hoener MC, Liechti ME (2012d) Duloxetine Inhibits Effects of MDMA (“Ecstasy”) In Vitro and in Humans in a Randomized Placebo-Controlled Laboratory Study . PLoS ONE 7 ( 5 ):e36476. 10.1371/journal.pone.0036476 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Simmler LD, Schillinger N, Meyer N, Schmid Y, Donzelli M, Grouzmann E, Liechti ME (2014b) Pharmacokinetic and pharmacodynamic effects of methylphenidate and MDMA administered alone or in combination . Int J Neuropsychopharmacol 17 ( 03 ):371–381. 10.1017/S1461145713001132 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hysek CM, Vollenweider FX, Liechti ME (2010) Effects of a beta-blocker on the cardiovascular response to MDMA (Ecstasy) . Emergency Medicine Journal : EMJ 27 ( 8 ):586–589. 10.1136/emj.2009.079905 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jerome L, Feduccia AA, Wang JB, Hamilton S, Yazar-Klosinski B, Emerson A, Mithoefer MC, Doblin R (2020) Long-term follow-up outcomes of MDMA-assisted psychotherapy for treatment of PTSD: A longitudinal pooled analysis of six phase 2 trials . Psychopharmacology 237 ( 8 ):2485–2497. 10.1007/s00213-020-05548-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnson MW, Garcia-Romeu A, Cosimano MP, Griffiths RR (2014) Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction . J Psychopharmacol 28 ( 11 ):983–992. 10.1177/0269881114548296 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnson MW, Griffiths RR, Hendricks PS, Henningfield JE (2018) The abuse potential of medical psilocybin according to the 8 factors of the Controlled Substances Act . Neuropharmacology 142 :143–166. 10.1016/j.neuropharm.2018.05.012 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnson MW, Hendricks PS, Barrett FS, Griffiths RR (2019) Classic psychedelics: An integrative review of epidemiology, therapeutics, mystical experience, and brain network function . Pharmacol Ther 197 :83–102. 10.1016/j.pharmthera.2018.11.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Johnson MW, Richards WA, Griffiths RR (2008) Human Hallucinogen Research: Guidelines for Safety . Journal of Psychopharmacology (oxford, England) 22 ( 6 ):603–620. 10.1177/0269881108093587 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaskey G (1992) Possible interaction between an MAOI and “ecstasy .” Am J Psychiatry 149 ( 3 ):411a–4412. 10.1176/ajp.149.3.411a [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Keeler MH (1967). Chlorpromazine Antagonism of Psilocybin Effect . International Journal of Neuropsychiatry , 3 , 66–71. https://bibliography.maps.org/bibliography/default/citation/1972 [ Google Scholar ]
- Khachatryan D, Groll D, Booij L, Sepehry AA, Schütz CG (2016) Prazosin for treating sleep disturbances in adults with posttraumatic stress disorder: A systematic review and meta-analysis of randomized controlled trials . Gen Hosp Psychiatry 39 :46–52. 10.1016/j.genhosppsych.2015.10.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kinzie JD, Leung P (1989) Clonidine in Cambodian patients with posttraumatic stress disorder . J Nerv Ment Dis 177 ( 9 ):546–550. 10.1097/00005053-198909000-00005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kirkpatrick MG, de Wit H (2015) MDMA: A social drug in a social context . Psychopharmacology 232 ( 6 ):1155–1163. 10.1007/s00213-014-3752-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kolbrich EA, Goodwin RS, Gorelick DA, Hayes RJ, Stein EA, Huestis MA (2008) Plasma pharmacokinetics of 3,4-methylenedioxymethamphetamine after controlled oral administration to young adults . Ther Drug Monit 30 ( 3 ):320–332. 10.1097/FTD.0b013e3181684fa0 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krystal JH, Rosenheck RA, Cramer JA, Vessicchio JC, Jones KM, Vertrees JE, Horney RA, Huang GD, Stock C, & Veterans Affairs Cooperative Study No. 504 Group (2011) Adjunctive risperidone treatment for antidepressant-resistant symptoms of chronic military service-related PTSD: A randomized trial . JAMA 306 ( 5 ):493–502. 10.1001/jama.2011.1080 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lauerma H, Wuorela M, Halme M (1998) Interaction of serotonin reuptake inhibitor and 3,4-methylenedioxymethamphetamine? Biol Psychiat 43 ( 12 ):929 [ PubMed ] [ Google Scholar ]
- Leonard JB, Anderson B, Klein-Schwartz W (2018) Does getting high hurt? Characterization of cases of LSD and psilocybin-containing mushroom exposures to national poison centers between 2000 and 2016 . Journal of Psychopharmacology (oxford, England) 32 ( 12 ):1286–1294. 10.1177/0269881118793086 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liechti ME (2000) Acute Psychological Effects of 3,4-Methylenedioxymethamphetamine (MDMA, “Ecstasy”) are Attenuated by the Serotonin Uptake Inhibitor Citalopram . Neuropsychopharmacology 22 ( 5 ):513–521. 10.1016/S0893-133X(99)00148-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liechti ME, Geyer MA, Hell D, & Vollenweider FX (2001). Effects of MDMA (ecstasy) on prepulse inhibition and habituation of startle in humans after pretreatment with citalopram, haloperidol, or ketanserin . Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology , 24 ( 3 ), 240–252. 10.1016/S0893-133X(00)00199-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liechti ME, Vollenweider FX (2000a) The serotonin uptake inhibitor citalopram reduces acute cardiovascular and vegetative effects of 3, 4-methylenedioxymethamphetamine (‘Ecstasy’) in healthy volunteers . J Psychopharmacol 14 ( 3 ):269–274. 10.1177/026988110001400313 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liechti ME, Vollenweider FX (2000b) Acute psychological and physiological effects of MDMA (“Ecstasy”) after haloperidol pretreatment in healthy humans . Eur Neuropsychopharmacol 10 ( 4 ):289–295. 10.1016/S0924-977X(00)00086-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu Y, She M, Wu Z, Dai R (2011) The inhibition study of human UDP-glucuronosyltransferases with cytochrome P450 selective substrates and inhibitors . J Enzyme Inhib Med Chem 26 ( 3 ):386–393. 10.3109/14756366.2010.518965 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lyon RA, Glennon RA, Titeler M (1986) 3,4-Methylenedioxymethamphetamine (MDMA): Stereoselective interactions at brain 5-HT1 and 5-HT2 receptors . Psychopharmacology 88 ( 4 ):525–526. 10.1007/BF00178519 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Malcolm B, Thomas K (2021) Serotonin toxicity of serotonergic psychedelics . Psychopharmacology . 10.1007/s00213-021-05876-x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Manevski N, Kurkela M, Höglund C, Mauriala T, Court MH, Yli-Kauhaluoma J, Finel M (2010) Glucuronidation of psilocin and 4-hydroxyindole by the human UDP-glucuronosyltransferases . Drug Metabolism and Disposition: the Biological Fate of Chemicals 38 ( 3 ):386–395. 10.1124/dmd.109.031138 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mattusek N, & Halbach A (1964). Über den Einfluss von Ergotamin auf die LSD-”Psychose” beim Menschen. [On the Influence of Ergotamine on LSD-”Psychosis” in Man] . In Psychopharmacologia (Vol. 5 , pp. 158–160). 10.1007/BF00413052 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McCann UD, Ricaurte GA (1993) Reinforcing subjective effects of (+/−) 3,4-methylenedioxymethamphetamine (“ecstasy”) may be separable from its neurotoxic actions: Clinical evidence . J Clin Psychopharmacol 13 ( 3 ):214–217 [ PubMed ] [ Google Scholar ]
- Mitchell JM, Bogenschutz M, Lilienstein A, Harrison C, Kleiman S, Parker-Guilbert K, G MO, Garas W, Paleos C, Gorman I, Nicholas C, Mithoefer M, Carlin S, Poulter B, Mithoefer A, Quevedo S, Wells G, Klaire SS, van der Kolk B, … Doblin R. (2021) MDMA-assisted therapy for severe PTSD: A randomized, double-blind, placebo-controlled phase 3 study . Nat Med 27 ( 6 ):1025–1033. 10.1038/s41591-021-01336-3 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mithoefer MC, Grob CS, Brewerton TD (2016) Novel psychopharmacological therapies for psychiatric disorders: Psilocybin and MDMA . The Lancet Psychiatry 3 ( 5 ):481–488. 10.1016/S2215-0366(15)00576-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mithoefer MC, Wagner MT, Mithoefer AT, Jerome L, Doblin R (2011) The safety and efficacy of ±3,4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: The first randomized controlled pilot study . Journal of Psychopharmacology (oxford, England) 25 ( 4 ):439–452. 10.1177/0269881110378371 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morefield KM, Keane M, Felgate P, White JM, Irvine RJ (2011) Pill content, dose and resulting plasma concentrations of 3,4-methylendioxymethamphetamine (MDMA) in recreational ‘ecstasy’ users . Addiction 106 ( 7 ):1293–1300. 10.1111/j.1360-0443.2011.03399.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moreno FA, Wiegand CB, Taitano EK, Delgado PL (2006) Safety, tolerability, and efficacy of psilocybin in 9 patients with obsessive-compulsive disorder . J Clin Psychiatry 67 ( 11 ):1735–1740. 10.4088/jcp.v67n1110 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Müller F, Holze F, Dolder P, Ley L, Vizeli P, Soltermann A, Liechti ME, Borgwardt S (2021) MDMA-induced changes in within-network connectivity contradict the specificity of these alterations for the effects of serotonergic hallucinogens . Neuropsychopharmacology 46 ( 3 ):545–553. 10.1038/s41386-020-00906-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Multidisciplinary Association for Psychedelic Studies . (2021). MAPS MDMA Investigator’s Brochure. [ Google Scholar ]
- Nardou R, Lewis EM, Rothhaas R, Xu R, Yang A, Boyden E, Dölen G (2019) Oxytocin-dependent reopening of a social reward learning critical period with MDMA . Nature 569 ( 7754 ):116–120. 10.1038/s41586-019-1075-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nayak S, Gukasyan N, Barrett FS, Erowid E, Erowid F, & Griffiths RR (2021). Classic psychedelic coadministration with lithium, but not lamotrigine, is associated with seizures: An analysis of online psychedelic experience reports . PsyArXiv . 10.31234/osf.io/r726d [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nichols DE (2020) Psilocybin: From ancient magic to modern medicine . J Antibiot 73 ( 10 ):679–686. 10.1038/s41429-020-0311-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oeri HE (2021) Beyond ecstasy: Alternative entactogens to 3,4-methylenedioxymethamphetamine with potential applications in psychotherapy . J Psychopharmacol 35 ( 5 ):512–536. 10.1177/0269881120920420 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O’Mathúna B, Farré M, Rostami-Hodjegan A, Yang J, Cuyàs E, Torrens M, Pardo R, Abanades S, Maluf S, Tucker GT, Torre R (2008) The consequences of 3,4-methylenedioxymethamphetamine induced CYP2D6 inhibition in humans . J Clin Psychopharmacol 28 ( 5 ):523–529. 10.1097/JCP.0b013e318184ff6e [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pacifici R, Pichini S, Zuccaro P, Farré M, Segura M, Ortuño J, Di Carlo S, Bacosi A, Roset PN, Segura J, de la Torre R (2004) Paroxetine Inhibits Acute Effects of 3,4-Methylenedioxymethamphetamine on the Immune System in Humans . J Pharmacol Exp Ther 309 ( 1 ):285–292. 10.1124/jpet.103.061374 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Papaseit E, Pérez-Mañá C, Torrens M, Farré A, Poyatos L, Hladun O, Sanvisens A, Muga R, Farré M (2020) MDMA interactions with pharmaceuticals and drugs of abuse . Expert Opin Drug Metab Toxicol 16 ( 5 ):357–369. 10.1080/17425255.2020.1749262 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Papaseit E, Vázquez A, Pérez-Mañá C, Pujadas M, de la Torre R, Farré M, Nolla J (2012) Surviving life-threatening MDMA (3,4-methylenedioxymethamphetamine, ecstasy) toxicity caused by ritonavir (RTV) . Intensive Care Med 38 ( 7 ):1239–1240. 10.1007/s00134-012-2537-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Partilla JS, Dempsey AG, Nagpal AS, Blough BE, Baumann MH, Rothman RB (2006) Interaction of Amphetamines and Related Compounds at the Vesicular Monoamine Transporter . J Pharmacol Exp Ther 319 ( 1 ):237–246. 10.1124/jpet.106.103622 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Passie T (2018) The early use of MDMA (‘Ecstasy’) in psychotherapy (1977–1985) . Drug Science, Policy and Law 4 :2050324518767442. 10.1177/2050324518767442 [ CrossRef ] [ Google Scholar ]
- Penmatsa A, Wang KH, Gouaux E (2013) X-ray structure of dopamine transporter elucidates antidepressant mechanism . Nature 503 ( 7474 ):85–90. 10.1038/nature12533 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Penmatsa A, Wang KH, Gouaux E (2015) X-ray structures of Drosophila dopamine transporter in complex with nisoxetine and reboxetine . Nat Struct Mol Biol 22 ( 6 ):506–508. 10.1038/nsmb.3029 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pilgrim JL, Gerostamoulos D, Woodford N, Drummer OH (2012) Serotonin toxicity involving MDMA (ecstasy) and moclobemide . Forensic Sci Int 215 ( 1–3 ):184–188. 10.1016/j.forsciint.2011.04.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pokorny T, Preller KH, Kraehenmann R, Vollenweider FX (2016) Modulatory effect of the 5-HT1A agonist buspirone and the mixed non-hallucinogenic 5-HT1A/2A agonist ergotamine on psilocybin-induced psychedelic experience . Eur Neuropsychopharmacol 26 ( 4 ):756–766. 10.1016/j.euroneuro.2016.01.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ramcharan S, Meenhorst P, Otten J, Koks C, de Boer D, Maes R, Beijnen J (1998) Survival After Massive Ecstasy Overdose . J Toxicol Clin Toxicol 36 ( 7 ):727–731. 10.3109/15563659809162623 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Richards JR, Hollander JE, Ramoska EA, Fareed FN, Sand IC, Gómez MMI, Lange RA (2017) β-Blockers, Cocaine, and the Unopposed α-Stimulation Phenomenon . J Cardiovasc Pharmacol Ther 22 ( 3 ):239–249. 10.1177/1074248416681644 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rickli A, Moning OD, Hoener MC, Liechti ME (2016) Receptor interaction profiles of novel psychoactive tryptamines compared with classic hallucinogens . Eur Neuropsychopharmacol 26 ( 8 ):1327–1337. 10.1016/j.euroneuro.2016.05.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rigg KK, Sharp A (2018) Deaths related to MDMA (ecstasy/molly): Prevalence, root causes, and harm reduction interventions . Journal of Substance Use 23 ( 4 ):345–352. 10.1080/14659891.2018.1436607 [ CrossRef ] [ Google Scholar ]
- Roseman L, Leech R, Feilding A, Nutt DJ, Carhart-Harris RL (2014) The effects of psilocybin and MDMA on between-network resting state functional connectivity in healthy volunteers . Front Hum Neurosci 8 . 10.3389/fnhum.2014.00204 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rudnick G, Wall SC (1992) The molecular mechanism of “ecstasy” [3,4-methylenedioxy-methamphetamine (MDMA)]: Serotonin transporters are targets for MDMA-induced serotonin release . Proc Natl Acad Sci 89 ( 5 ):1817–1821. 10.1073/pnas.89.5.1817 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Saleemi S, Pennybaker SJ, Wooldridge M, Johnson MW (2017) Who is “Molly”? MDMA adulterants by product name and the impact of harm-reduction services at raves . Journal of Psychopharmacology (oxford, England) 31 ( 8 ):1056–1060. 10.1177/0269881117715596 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schatzberg AF, & Nemeroff CB (2017). The American Psychiatric Association Publishing Textbook Of Psychopharmacology . American Psychiatric Pub. [ Google Scholar ]
- Scherrer JF, Salas J, Cohen BE, Schnurr PP, Schneider FD, Chard KM, Tuerk P, Friedman MJ, Norman SB, van den Berk-Clark C, & Lustman PJ (2019). Comorbid Conditions Explain the Association Between Posttraumatic Stress Disorder and Incident Cardiovascular Disease . Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease , 8 ( 4 ). 10.1161/JAHA.118.011133 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schmid Y, Rickli A, Schaffner A, Duthaler U, Grouzmann E, Hysek CM, Liechti ME (2015) Interactions between Bupropion and 3,4-Methylenedioxymethamphetamine in Healthy Subjects . J Pharmacol Exp Ther 353 ( 1 ):102–111. 10.1124/jpet.114.222356 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schmid Y, Vizeli P, Hysek CM, Prestin K, Meyer zu Schwabedissen HE, & Liechti ME (2016) CYP2D6 function moderates the pharmacokinetics and pharmacodynamics of 3,4-methylenedioxymethamphetamine in a controlled study in healthy individuals . Pharmacogenet Genomics 26 ( 8 ):397–401. 10.1097/FPC.0000000000000231 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Scriba GKE (2011). Sweetman Sean C.(Ed.): Martindale: The Complete Drug Reference . Chromatographia , 74 ( 7 ), 647–648. 10.1007/s10337-011-2101-8 [ CrossRef ] [ Google Scholar ]
- Segura M, Farre M, Pichini S, Peiro AM, Roset PN, Ramirez A, Ortuno J, Pacifici R, Zuccaro P, Segura J, de la Torre R (2005) Contribution of Cytochrome P450 2D6 to 3,4-Methylenedioxymethamphetamine Disposition in Humans: Use of Paroxetine as a Metabolic Inhibitor Probe . Clin Pharmacokinet 44 ( 6 ):649–660. 10.2165/00003088-200544060-00006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sessa B (2017) MDMA and PTSD treatment: “PTSD: From novel pathophysiology to innovative therapeutics .” Neurosci Lett 649 :176–180. 10.1016/j.neulet.2016.07.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sessa B, Higbed L, O’Brien S, Durant C, Sakal C, Titheradge D, Williams TM, Rose-Morris A, Brew-Girard E, Burrows S, Wiseman C, Wilson S, Rickard J, Nutt DJ (2021) First study of safety and tolerability of 3,4-methylenedioxymethamphetamine-assisted psychotherapy in patients with alcohol use disorder . J Psychopharmacol 35 ( 4 ):375–383. 10.1177/0269881121991792 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shulgin AT (1986) The background and chemistry of MDMA . J Psychoactive Drugs 18 ( 4 ):291–304. 10.1080/02791072.1986.10472361 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Silins E, Copeland J, Dillon P (2007) Qualitative Review of Serotonin Syndrome, Ecstasy (MDMA) and the use of Other Serotonergic Substances: Hierarchy of Risk . Aust N Z J Psychiatry 41 ( 8 ):649–655. 10.1080/00048670701449237 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Simmler LD, Hysek CM, Liechti ME (2011) Sex Differences in the Effects of MDMA (Ecstasy) on Plasma Copeptin in Healthy Subjects . J Clin Endocrinol Metab 96 ( 9 ):2844–2850. 10.1210/jc.2011-1143 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smilkstein MJ, Smolinske SC, Rumack BH (1987) A Case of Mao Inhibitor/MDMA Interaction: Agony After Ecstasy . J Toxicol Clin Toxicol 25 ( 1–2 ):149–159. 10.3109/15563658708992620 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stein DJ, & Rink J (1999). Effects of “Ecstasy” Blocked by Serotonin Reuptake Inhibitors . The Journal of Clinical Psychiatry , 60 ( 7 ), 485–485. https://www.psychiatrist.com/JCP/article/Pages/effects-ecstasy-blocked-serotonin-reuptake-inhibitors.aspx [ PubMed ] [ Google Scholar ]
- Steuer AE, Schmidhauser C, Tingelhoff EH, Schmid Y, Rickli A, Kraemer T, Liechti ME (2016) Impact of Cytochrome P450 2D6 Function on the Chiral Blood Plasma Pharmacokinetics of 3,4-Methylenedioxymethamphetamine (MDMA) and Its Phase I and II Metabolites in Humans . PLoS ONE 11 ( 3 ):e0150955. 10.1371/journal.pone.0150955 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Strassman R (1992). Human Hallucinogen Interactions with Drugs Affecting Serotonergic . Neuropsychopharmacol , 7 ( 3 ). [ PubMed ] [ Google Scholar ]
- Studerus E, Gamma A, & Vollenweider FX (2010). Psychometric Evaluation of the Altered States of Consciousness Rating Scale (OAV) . PLoS ONE , 5 ( 8 ). 10.1371/journal.pone.0012412 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Studerus E, Vizeli P, Harder S, Ley L, Liechti ME (2021) Prediction of MDMA response in healthy humans: A pooled analysis of placebo-controlled studies . J Psychopharmacol 0269881121998322. 10.1177/0269881121998322 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tancer M, Johanson C-E (2006) The effects of fluoxetine on the subjective and physiological effects of 3,4-methylenedioxymethamphetamine (MDMA) in humans . Psychopharmacology 189 ( 4 ):565–573. 10.1007/s00213-006-0576-z [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thomas K, Malcolm B, Lastra D (2017) Psilocybin-Assisted Therapy: A Review of a Novel Treatment for Psychiatric Disorders . J Psychoactive Drugs 49 ( 5 ):446–455. 10.1080/02791072.2017.1320734 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Togni LR, Lanaro R, Resende RR, Costa JL (2015) The variability of ecstasy tablets composition in Brazil . J Forensic Sci 60 ( 1 ):147–151. 10.1111/1556-4029.12584 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Usona Institute. (2021). Usona Institute Psilocybin Investigator’s Brochure (Vol. 4 ). [ Google Scholar ]
- VA/DOD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder . (2017) 200
- Valeriani G, Corazza O, Bersani FS, Melcore C, Metastasio A, Bersani G, Schifano F (2015) Olanzapine as the ideal “trip terminator”? Analysis of online reports relating to antipsychotics’ use and misuse following occurrence of novel psychoactive substance-related psychotic symptoms . Hum Psychopharmacol 30 ( 4 ):249–254. 10.1002/hup.2431 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vargas AS, Luís Â, Barroso M, Gallardo E, Pereira L (2020) Psilocybin as a New Approach to Treat Depression and Anxiety in the Context of Life-Threatening Diseases—A Systematic Review and Meta-Analysis of Clinical Trials . Biomedicines 8 ( 9 ):331. 10.3390/biomedicines8090331 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Verrico CD, Miller GM, Madras BK (2007) MDMA (Ecstasy) and human dopamine, norepinephrine, and serotonin transporters: Implications for MDMA-induced neurotoxicity and treatment . Psychopharmacology 189 ( 4 ):489–503. 10.1007/s00213-005-0174-5 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vizeli P, Schmid Y, Prestin K, Schwabedissen MZ, H E, & Liechti ME. (2017) Pharmacogenetics of ecstasy: CYP1A2, CYP2C19, and CYP2B6 polymorphisms moderate pharmacokinetics of MDMA in healthy subjects . European Neuropsychopharmacology: the Journal of the European College of Neuropsychopharmacology 27 ( 3 ):232–238. 10.1016/j.euroneuro.2017.01.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vollenweider FX, Vollenweider-Scherpenhuyzen MFI, Bäbler A, Vogel H, & Hell D (1998). Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action : NeuroReport , 9 ( 17 ), 3897–3902. 10.1097/00001756-199812010-00024 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vuori E, Henry JA, Ojanperä I, Nieminen R, Savolainen T, Wahlsten P, Jäntti M (2003) Death following ingestion of MDMA (ecstasy) and moclobemide: Fatal MDMA-moclobemide interaction . Addiction 98 ( 3 ):365–368. 10.1046/j.1360-0443.2003.00292.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wagner MT, Mithoefer MC, Mithoefer AT, MacAulay RK, Jerome L, Yazar-Klosinski B, Doblin R (2017) Therapeutic effect of increased openness: Investigating mechanism of action in MDMA-assisted psychotherapy . Journal of Psychopharmacology (oxford, England) 31 ( 8 ):967–974. 10.1177/0269881117711712 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- White TL, Justice AJH, de Wit H (2002) Differential subjective effects of D-amphetamine by gender, hormone levels and menstrual cycle phase . Pharmacol Biochem Behav 73 ( 4 ):729–741. 10.1016/s0091-3057(02)00818-3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wood DM, Stribley V, Dargan PI, Davies S, Holt DW, Ramsey J (2011) Variability in the 3,4-methylenedioxymethamphetamine content of “ecstasy” tablets in the UK . Emergency Medicine Journal: EMJ 28 ( 9 ):764–765. 10.1136/emj.2010.092270 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yockey A, King K (2021) Use of psilocybin (“mushrooms”) among US adults: 2015–2018 . Journal of Psychedelic Studies 5 ( 1 ):17–21. 10.1556/2054.2020.00159 [ CrossRef ] [ Google Scholar ]

Using ‘trip killers’ to cut short bad drug trips is potentially dangerous
Professor of Neuropharmacology, University of Central Lancashire
Disclosure statement
Colin Davidson has previously received funding from the National Institute on Drug Abuse (NIH, USA) and the European Community for projects related to stimulant drug abuse and novel psychoactive compounds respectively. He is currently a paid consultant with the Defence Science Technology Laboratory (MOD) working on new psychoactive compounds.
University of Central Lancashire provides funding as a member of The Conversation UK.
View all partners
As interest in psychedelics has grown, so has interest in ways to end a bad trip. Recent research reveals that people are giving potentially dangerous advice on social media on how to stop a trip that is less than pleasurable.
Psychedelics cause changes in a person’s perception of reality. One of the earliest descriptions of a psychedelic experience in western literature can be found in Aldous Huxley’s 1953 book The Doors of Perception . Huxley describes mostly beautiful visions while tripping on mescaline.
And then there were the Beatles seeing “tangerine trees” and “marmalade skies” and “a girl with kaleidoscope eyes”.
The last few years have seen a resurgence of illicit use, not only of established psychedelics, such as LSD and magic mushrooms (psilocybin), but also of the novel psychoactive substances that are psychedelics, such as AMT, 5-MeO-DALT, mCPP and methoxetamine.
There is also renewed interest in studying these drugs as treatments for mental health conditions, such as post-traumatic stress disorder (PTSD) and depression. Even a single dose of these drugs appears to have long-term therapeutic effects.
But not all trips are pleasurable. Research shows that if someone is in a bad mood or depressed then they are more likely to have a bad trip , as are people who take too high a dose.
This sort of experience might include extreme fear, time standing still and mood swings. Very high doses of LSD can also cause agitation, vomiting, high blood pressure, hyperthermia and other nasty side-effects. But at regular doses, psychedelics are relatively safe .
To mitigate against bad trips, people will often take the drug in a relaxing and safe environment, and they might include a friend, or “trip sitter” to look after them for the duration of the trip. This was a common practice in the 1960s among people taking psychedelics.

Trip killers
More recently, though, some psychedelic users have been turning to “trip killers” to end a bad trip. These are drugs that can either block the direct effects of the psychedelic or simply reduce the anxiety associated with a bad trip.
Few clinical studies have examined trip killers, but one has found that ketanserin – a drug used to treat high blood pressure – reverses the psychedelic effects of LSD.
A recent article in the Emergency Medical Journal analysed posts on Reddit about trip killers. The researchers found 128 threads with 709 posts from 2015 to 2023.
Trip killers were discussed most often for LSD (235 posts), magic mushrooms (143 posts) and MDMA (21 posts). The most commonly suggested trip killer was Xanax (an anxiolytic) followed by quetiapine (an antipsychotic), trazodone (an antidepressant) and diazepam (an anxiolytic). Alcohol, herbal remedies, opioids, antihistamines, sleep medication and cannabinoids were barely mentioned.
Receptor blocking
LSD and magic mushrooms create their effects by activating certain proteins in the brain. These are called 5-HT2A receptors and are usually activated by the neurotransmitter serotonin (5-HT). There are 14 known 5-HT receptors, but psychedelics have specific activity at only the 5-HT2A subtype.
To kill a trip then, one simply has to give the drug user another drug that blocks (rather than activates) the 5-HT2A receptor. Many prescription drugs can do this and they tend to be antipsychotic drugs .
Quetiapine from the list above is one popular example, while another antipsychotic, olanzapine, was mentioned in 14 posts in that study. Similarly, the atypical antidepressants trazodone and mirtazapine also block the 5-HT2A receptor.
One can think of these trip killers as working in the same way that naloxone would be used for heroin or fentanyl overdose. These drugs activate mu opioid receptors in the brain, while naloxone blocks these receptors. Naloxone is therefore used to treat life-threatening respiratory depression from opioid overdose.
Another option for the psychedelics would be to decrease the anxiety associated with the trip by taking anxiolytics, such as benzodiazapines – alprazolam (Xanax) and diazepam (Valium) being the most popular in the posts analysed above. These would also help the drug taker to fall asleep.
Some of the trip-killing drug doses suggested in the Reddit posts were high. For example, quetiapine was suggested to be used at 25mg to 600mg, but clinical guidance for these drugs suggests a single dose of up to 225mg.
The doses suggested on Reddit for alprazolam are 0.5mg to 4mg but the clinically suggested maximum dose is usually 2mg to 3mg. Four milligrams could cause low blood pressure, oversedation and respiratory depression. Unfortunately, benzodiazepines are also highly addictive and can lead to overdose deaths.
People who turn up at A&E suffering from a bad trip or overdose of a psychedelic will be reassured in a calm environment. If that doesn’t work, they are likely to be given an antipsychotic or low-dose benzodiazepine, at a clinically advised dose.
Read more: A brief history of drug-fuelled combatants
- War on Drugs
- Psychedelics
- Richard Nixon

Events Officer

Lecturer (Hindi-Urdu)

Director, Defence and Security

Opportunities with the new CIEHF

School of Social Sciences – Public Policy and International Relations opportunities
The Truth About Mushrooms & Meds: Are They Safe to Mix?
In this guide, we explore the potential interactions between psilocybin, the primary psychoactive compound in magic mushrooms, and various pharmaceutical medications.
Many people are wondering whether they can combine magic mushrooms with their prescription medicines, like antidepressants , or anxiolytics, or even antipsychotics. And it's no wonder—we've all heard of their seemingly miraculous ability to reset the brain. The promise of healing and transformation, of reclaiming ourselves with minimal side effects or addiction, is enticing, to say the least.
At the same time, you're likely here because you're not sure whether it's safe to combine your prescription meds with those nootropic microdose caps you saw an ad for.
In our mission to make access to plant medicines safer and more accessible, and to help reduce the potential for harm, we put together this systematic review of Randomized Clinical Trials (RCTs) studying the interactions between magic mushrooms and pharmaceutical medications.
This systematic review aims to bring together all the available data concerning the pharmacokinetic (how the body interacts with it), physiological, and subjective effects of drug interactions between psilocybin and medications prescribed in psychiatry. We shed light on how these fascinating fungi may interact with different types of medications, and how they might potentially affect each other.
While reviews of drug interactions with psilocybin have been published, none have been systematic, and this review serves as the first comprehensive exploration of drug interactions involving psilocybin.
Let's delve into the findings.
What is psilocybin?

Psilocybin is a naturally occurring compound and renowned psychoactive tryptamine found in over 200 species of mushrooms , particularly in the Psilocybe genus. Often referred to as a " classic psychedelic ," psilocybin's effects on perception, emotion, and cognition primarily stem from its interaction with 5-HT2A receptors, although it also binds to other 5-HT receptor subtypes.
Psilocybin has long been enjoyed both medicinally and recreationally. In both spiritual and clinical settings. In its raw form, lemon juice extractions , or ground into capsules and combined with other functional foods. Foodies delight in their brownies and gummies .
Clinical trials have administered psilocybin in various doses , ranging from very low to high, with effects typically beginning within 20-40 minutes, peaking around 60-90 minutes, and lasting for approximately 6 hours.
The metabolism of psilocybin.

When you ingest magic mushrooms, the psilocybin hidden in their cell walls rapidly converts to its active form, psilocin, through enzymatic processes (your liver).
Unlike some substances, psilocybin and psilocin do not significantly inhibit monoamine reuptake pumps, reducing the risk of increased serotonin levels, and thus, serotonin toxicity.
Psilocybin's physiological and psychological effects.
Physiologically, psilocybin can cause mild increases in blood pressure and heart rate, with common adverse effects including headache, nausea, dizziness, and fatigue.
On a psychological level, psilocybin often induces mystical-type experiences, characterized by a heightened sense of unity, altered perception of time and space, and feelings of euphoria. These experiences are associated with decreased activity in specific brain circuits known as the default mode network (DMN) and long-term improvements in well-being.
It's worth noting that psilocybin lacks dopamine-mediated reinforcement and does not appear to lead to habituation or addiction.
However, psilocybin is not for everyone. It's likely a bad idea to trip if you're grieving. Some users may experience transient anxiety, dysphoria, impaired sleep, paranoia, grief, and preoccupation with death.
Speak to a trusted therapist who is trained in psilocybin-assisted therapy to make sure it's right for you. They can guide you through from preparation to integration, ensuring a safe and optimal journey to personal growth and healing.
How psilocybin works.

As you can see in the figure above, psilocin and serotonin are structurally similar.
Psilocin is psilocybin's active form. Because of its similarity to serotonin, it activates serotonin 5-hydroxytryptamine-2A (5-HT2A) receptors, creating an altered state of mind that can produce positive mood effects , including mystical experiences and feelings of bliss. These acute effects have been linked to long-term improvements in depression , anxiety, and addiction .
Psilocybin may also promote neuroplasticity and increase markers of neuroregeneration, such as brain-derived neurotrophic factor (BDNF).
However, it's important to note that psilocybin can also lead to short-term adverse effects like anxiety, headache, insomnia, and nausea.
Psilocybin's drug interaction potential.
The potential for drug interactions with psilocybin is an important consideration, especially when combined with medications that also affect the serotonin system, such as SSRIs, SNRIs, TCAs, MAOIs , mirtazapine, trazodone, lithium, buspirone, atypical antipsychotics, and others.
Some interactions may increase the risk of toxidromes like serotonin syndrome. Additionally, the effects of psilocybin can be attenuated by recent exposure to antidepressants. This requires careful consideration of washout periods.
Furthermore, there are potential interactions with drugs targeting neurotransmitter systems beyond serotonin, such as norepinephrine and dopamine, which can impact the effects of psilocybin. Benzodiazepines may be used to mitigate acute adverse effects related to psychedelics, and some medications can influence the metabolism of psilocybin through their impact on enzymes.
Antipsychotics and psilocybin.
There are three Randomized Controlled Trials (RCTs) where researchers combined psilocybin with three antipsychotics: chlorpromazine, haloperidol, and risperidone.
The first study paired chlorpromazine, a typical antipsychotic, with psilocybin, resulting in a reduction in psilocybin-induced eye dilation and visual perceptual changes.
In 1998, Vollenweider et al. conducted the two other studies, one investigating the effects of haloperidol and the other investigating risperidone, which antagonize D2 receptors. Haloperidol had no impact on psilocybin-induced perceptual changes but increased the sense of "dread of ego dissolution." On the other hand, risperidone reduced various aspects of altered consciousness induced by psilocybin, including the reduction of dread of ego dissolution. Working memory was tested, revealing that psilocybin alone delayed reaction time, but this delay was less pronounced when co-administered with risperidone.
Antidepressants and psilocybin.

Psilocybin is often studied for use in patients with psychiatric disorders, many of whom are already on antidepressant medications, particularly serotonin transporter inhibitors.
Previous case reports and clinical practices suggested that antidepressants might diminish the effects of psychedelics. Therefore, it has been a common practice to discontinue antidepressant treatment before administering psychedelics, raising concerns about withdrawal symptoms and potential relapses of depression.
Below, we investigate the 3 clinical studies to date on combining antidepressants with psilocybin.
Serotonin agonists and psilocybin.
A single RCT by Pokorny et al. in 2016 explored the combination of psilocybin with serotonin agonists .
Psilocybin binds to 5-HT1A and 5-HT2A receptors, and the researchers examined its effects when combined with buspirone and ergotamine, both of which have similar receptor affinities.
Buspirone reduced visionary restructuralization (the visual elements of the trip), suggesting that it reduced psilocybin-induced visual perceptual changes. Ergotamine, on the other hand, had no significant effect on psilocybin-induced subjective experiences, possibly due to differing receptor profiles.
Selective serotonin reuptake inhibitors (SSRIs) and psilocybin.
Conducted in 2021, Becker et al. combined psilocybin with the SSRI escitalopram in one of the only two RCT on SSRIs and psilocybin as of this writing.
Contrary to earlier reports stating that SSRIs reduced the effects of LSD, escitalopram did not significantly diminish the subjective effects of psilocybin. Instead, it was associated with reductions in negative experiences like fear, anxiety, and ineffability.
Physiologically, escitalopram reduced psilocybin-induced elevations in blood pressure and pupil dilation, without altering levels of psilocin.
Exploring escitalopram's impact on psilocybin.
In this double-blind, placebo-controlled, crossover study, healthy subjects underwent two experimental test sessions, each involving psilocybin (25 mg) after either escitalopram pretreatment or placebo. The order of treatment was randomized and counterbalanced.
Escitalopram pretreatment involved daily doses of 10 mg for 7 days, followed by 20 mg for another 7 days, including the day of psilocybin administration. In contrast, the placebo group received 14 days of pretreatment with a placebo before the psilocybin session.
The study assessed various outcome measures, including subjective effects, adverse effects, cardiovascular responses, plasma BDNF levels, gene expression, and pharmacokinetics.
Key findings and implications.
The results of the study indicated that escitalopram pretreatment did not have a significant effect on the positive mood effects of psilocybin. However, it did significantly reduce adverse effects, anxiety, adverse cardiovascular effects, and other negative effects associated with psilocybin when compared to placebo pretreatment.
Importantly, escitalopram did not alter the pharmacokinetics of psilocin, the psychoactive form of psilocybin.
This research sheds light on the potential safety of combining psilocybin with escitalopram treatment, offering an initial indication that such combinations may be viable. Further studies are needed, particularly with extended antidepressant pretreatment and with patients suffering from psychiatric disorders, to provide more comprehensive insights into the interactions between antidepressants and psilocybin.
COMPASS Pathways announces positive outcome of 25mg COMP360 psilocybin therapy as adjunct to SSRI antidepressants.

In 2021, an open-label study presented groundbreaking findings that challenged the widely-held belief that SSRI medications would interfere with the therapeutic effects of psilocybin, opening the door to new possibilities in depression treatment. This research paves the way for psilocybin therapy to be considered both as an adjunctive treatment to SSRI antidepressants and as a therapy on its own.
Breaking down the COMP360 study.
This open-label study involved 19 patients from clinical sites in Ireland and the United States. Most of the patients were female (68.4%), with an average age of 42 years. The primary objective was to assess the change in baseline MADRS (Montgomery-Åsberg Depression Rating Scale) total score at 3 weeks in patients receiving 25mg COMP360 psilocybin therapy alongside their existing SSRI antidepressant regimen.
The results were remarkable, with 42.1% of patients showing a positive response at week 3, and all of them achieving remission. The mean reduction in the MADRS total score at week 3 was 14.9, signifying a significant improvement. These findings were consistent with the phase IIb trial results and indicated a rapid response from day 2 to week 3 after COMP360 therapy.
The study participants initially had a baseline MADRS score of 31.7, indicating moderate to severe depression. In addition to MADRS scores, other measures also showed positive signals of improvement, including reduced anxiety, improved depressive symptoms (assessed by clinicians and self-rated), and enhanced positive and negative affect.
Safety and tolerability.
Importantly, the 25mg COMP360 psilocybin therapy was well-tolerated when administered alongside the patients' SSRI treatment. There were no serious treatment-emergent adverse events, and no adverse events related to suicidal ideation or self-injury.
Epidemiologic studies on psilocybin.
In 2021, Nayak et al. analyzed accounts of co-ingesting mood stabilizers (lithium and lamotrigine) with psychedelic substances, including psilocybin. Some reports involving lithium resulted in seizures, while those combining lamotrigine with psilocybin did not. Nevertheless, the evidence was considered low-quality due to a lack of standardization and clinical verification.
The researchers analyzed 96 accounts posted online, primarily on platforms like Erowid, the Shroomery, and Reddit. These accounts detailed experiences involving the concurrent use of mood stabilizers, including lithium, lamotrigine, valproic acid, carbamazepine, and oxcarbazepine, alongside various psychedelic substances. While the analysis covered a range of psychedelics, the majority of the reports centered around lysergic acid diethylamide (LSD), another well-known classic psychedelic.
In the context of mood stabilizers, the study focused on the combination of lamotrigine and lithium with psilocybin. Out of the six reports involving the combination of lithium and psilocybin, two cases resulted in seizures. Conversely, none of the ten reports involving lamotrigine and psilocybin reported seizures.
It's essential to note that the study authors acknowledged the evidence's low quality due to certain limitations, including a lack of standardization, potential selection bias, and the absence of clinical verification. These factors suggest that while the findings are valuable, further research with greater rigor and control is needed to draw more definitive conclusions about the potential interactions between psilocybin and mood stabilizers, particularly in the context of seizure risk.
The need for further exploration.

In the context of clinical research and the potential application of psilocybin in therapy, it is essential to explore these interactions to ensure safe and effective treatment protocols. These studies set the stage for more in-depth investigations and have the potential to reshape clinical practices, potentially eliminating the need to discontinue antidepressant treatment when administering psilocybin in clinical settings.
Always consult with a medical professional for personalized advice. While the effects of combining psilocybin with different types of medications can vary, it's important to consider these findings and exercise caution when combining these substances, especially if you are taking psychiatric medications.
If you are searching for professional support from a healthcare provider, please refer to our directory of psychedelic therapists in Canada , sorted by city.
Mixing mushrooms & meds FAQs.
What is psilocybin therapy, and how does it differ from traditional treatments for depression and anxiety.
Psilocybin therapy involves the controlled use of the psychoactive compound psilocybin, found in certain mushrooms, as a therapeutic intervention for mental health conditions. Unlike traditional treatments, it aims to address the root causes of depression and anxiety by promoting profound, introspective experiences that can lead to lasting improvements in mood and well-being.
Can I continue taking my prescribed antidepressant medication while undergoing psilocybin therapy?
In some cases, individuals may be able to continue their antidepressant medication while undergoing psilocybin therapy. However, it's essential to consult with a healthcare professional to determine the best approach for your specific situation.
Are there any known interactions between psilocybin and common antidepressant medications like SSRIs and SNRIs?
Some studies suggest that there may not be significant interactions between psilocybin and common antidepressants like SSRIs and SNRIs. However, individual responses can vary, so it's crucial to seek guidance from a healthcare provider.
Can highly potent mushroom strains be used for therapeutic purposes?
Not all strains of magic mushrooms are equally potent. Potency can vary significantly between strains due to differences in their psilocybin and psilocin content, genetics, and growing conditions. Some strains are notably more potent than others.
There is growing interest in using highly potent mushroom strains for therapeutic purposes, particularly for conditions like depression, anxiety, and PTSD. However, research in this area is ongoing and should only be done under the professional guidance of an experienced guide or psilocybin therapist.
Is it safe to combine psilocybin therapy with my existing antidepressant treatment?
The safety of combining psilocybin therapy with antidepressants may depend on various factors, including the specific medications you're taking and your overall health. Consultation with a qualified healthcare provider is essential to ensure safety.
What do the recent research findings suggest about the compatibility of psilocybin therapy and antidepressants?
Recent research findings indicate that psilocybin therapy can be compatible with some antidepressant treatments, and it may not significantly interfere with their therapeutic effects. This provides promising insights into potential treatment options.
Can psilocybin therapy be considered as both an adjunctive treatment to antidepressants and a standalone treatment for depression and anxiety?
Yes, psilocybin therapy is being explored as both an adjunctive treatment to existing antidepressants and a standalone treatment. The choice may depend on individual circumstances and the recommendations of healthcare professionals.
How can I discuss the possibility of psilocybin therapy with my healthcare provider if I'm already on antidepressant medication?
Initiate a conversation with your healthcare provider about the potential integration of psilocybin therapy into your treatment plan. Share relevant research and inquire about their insights and recommendations.
What are the potential benefits and risks of combining psilocybin therapy with my antidepressant treatment?
The benefits may include improved treatment outcomes for depression and anxiety. Risks may involve possible interactions between psilocybin and your antidepressant medication. Discuss these aspects with your healthcare provider.
How do I know if I'm a suitable candidate for psilocybin therapy, especially if I'm currently on antidepressants?
Your suitability for psilocybin therapy can be assessed by a healthcare professional. Factors like your medical history, current medications, and mental health condition will be considered in the evaluation.
What precautions should I take when considering the integration of psilocybin therapy with my antidepressant regimen?
Precautions include thorough medical evaluations, ongoing monitoring, and open communication with your healthcare provider. It's essential to follow their guidance closely.
Are there any recommended guidelines or best practices for managing the transition to psilocybin therapy while on antidepressants?
Best practices may involve a gradual reduction of antidepressants under medical supervision. Establishing a clear treatment plan and maintaining open communication with your healthcare provider are crucial.
How can I ensure my safety and well-being during psilocybin therapy, particularly if I'm already taking antidepressant medications?
Safety can be ensured by following your healthcare provider's recommendations, participating in sessions in a controlled environment, and having a support system in place.
What steps should I take if I experience adverse effects or unexpected reactions when combining psilocybin therapy with my antidepressants?
If adverse effects occur, immediately contact your healthcare provider for guidance. They can help manage any unexpected reactions or side effects.
Are there any upcoming clinical trials or research initiatives focused on psilocybin therapy and its interaction with antidepressants?
Ongoing research and clinical trials continue to explore the potential of psilocybin therapy and its interactions with antidepressants. Stay informed about these studies through reputable sources.
Where can I find reputable, licensed facilities or practitioners offering psilocybin therapy that take into account my antidepressant treatment?
Explore licensed psychedelic therapists near you through our Psychedelic-Assisted Therapy directory. There, you'll find licensed and reputable facilities or practitioners that offer psilocybin therapy. Ensure that the professionals are experienced in this field and operate legally.
Which type of magic mushroom is used for psilocybin therapy?
The Golden Teacher strain from the Psilocybe cubensis species is the most circulated strain for both research, therapeutic, and recreational purposes because of their potent yet gentle journeys. The Golden Teacher's ability to bring about introspective and transformational journeys in a mild and balanced manner is the reason we use it in all our formulations. Balanced High (aka Scooby Snacks) is a favourite among our customers and therapists we know for therapeutic outcomes.
Discover Magic Mushroom Strains.
Discover magic mushroom microdose supplements..

Brain Stack | Microdose Capsules
Optimal cognition + brain health.

Energy Stack | Microdose Capsules
Energy + mood + brain function.

Vitality Stack | Microdose Capsules
Age backwards, discover magic mushroom macrodose supplements..

Balanced High | Macrodose Capsules
Aka scooby snacks, 250mg psilocybin per capsule.

Extended Release | Macrodose Capsules
Aka increased tuc, 250mg psilocybe cubensis per capsule.
You must be logged in to post a comment.

- Psychedelic Coaching
- Bipolar Disorder
- Cluster Headaches
- End of Life
- Parkinson’s Disease
- Psychedelic Timeline
- Our Friends
Select Page
How to Use TripSit’s ‘Guide to Drug Combinations’ Chart
Posted by David Wilder | Jan 24, 2018 | Articles , Harm Reduction , Resources | 0

A Note from TripSit
WARNING! For educational purposes: We do not endorse any of these combinations. This [chart] will always be ‘work in progress’. It is extremely important to be safe at all times! See below the graphic for important information regarding specific combinations.
This chart is meant as a quick reference guide and additional research MUST always be done. If you use this chart or information on your site you must link to the full summaries and display this message.
If you want to give [TripSit] some feedback/recommendation/comment on the chart, you can contact [them]: Join #content channel on IRC Email: [email protected]
Although most psychoactive substances are quite powerful in their own rights, some psychonauts may choose to combine two or more of them at the same time to take their experience even further. Combining multiple psychoactive substances during one session has the potential to jettison the user into brand-new psychedelic territories, or catalyze new perspectives on life or the concept of reality. However, it can also result in severe physical discomfort, relentless psychological trauma, and even death. Because of the high risk potential, this advanced technique should not be attempted by those new to psychedelics, and even those with years of experience should still tread lightly and proceed with extreme caution.
In an effort to reduce the potential dangers of drug combining, the harm reduction website TripSit created Version 3.0 of the Guide to Drug Combinations chart in 2016 (shown above.) Although the image featured above is quite small, TripSit also offers a larger version of the chart for improved legibility. We advise taking a close look at the larger version if you want to learn more about the potential effects and risks that come with combining psychoactive substances. We have put together the following chart reading guide as an introduction to this resource, which we hope will help our readers make informed decisions and reduce any potential harms resulting from combining drugs.

How to Read the Chart
The Guide to Drug Combinations chart is fairly easy to read. First, simply identify the first substance you would like to reference on the chart’s X axis. Next, locate the second substance on the Y axis. The area in the center of the chart where the first substance’s column meets the second substance’s row will display the anticipated level of risk for that particular combination. More information about the various risk categories can be found below.
In addition to providing translated versions of this chart in Spanish , German , French , and Esperanto , TripSit also has detailed descriptions of specific combinations on its Drug Combinations webpage, located a few sections below the chart. These descriptions offer more information about each unique combination of substances, which can be extremely helpful—potentially even life-saving—if you are considering using two or more drugs at the same time.

TripSit created a total of six categories that are used in the Guide to Drug Combinations chart. Each category assesses the safety level of a drug combination, as well as whether the combination will cause a synergistic effect. A combination that is potentially “synergistic” may result in an effect greater than the sum of its parts.
Low Risk and Synergy: This category describes substances that are unlikely to cause adverse or undesirable reactions aside from those that are ordinarily anticipated from using each substance individually. In addition, the substances are likely to have a synergistic effect when combined.
Low Risk and No Synergy: This combination is not likely to cause an adverse or undesirable reaction when used carefully. In addition, there is no synergistic effect—the effects are simply additive.
Low Risk and Decrease: A drug combination that falls into this category will have a low risk of causing an adverse or undesirable reaction, and each substance’s effects will be dampened, rather than amplified.
Caution: While not likely to be physically harmful, a drug combination in this category may produce undesirable effects like physical discomfort or overstimulation. Frequent or high-dosage use may result in physical health issues, and the potential for synergistic effect is possible—albeit unpredictable. As the category name suggests, users who wish to experiment with a drug combination in this category should proceed with caution.
Unsafe: When a drug combination is categorized as unsafe, there is a severe risk of physical harm to the user. These combinations should be approached with extreme caution, and it is best to avoid them entirely.
Dangerous: The final category includes drug combinations that are known to be extremely harmful both physically and psychologically. In fact, the reactions from experimenting with these combinations are wildly unpredictable and there is a realistic chance of death. These combinations should be avoided at all costs.

The concept of combining multiple psychoactive substances is appealing to some psychonauts, and this practice can provide both positive and negative outcomes. To prevent both psychological and physical issues from occurring, it is always best to learn as much about the potential effects a drug combination may produce before trying it. Psychedelic Times would like to thank TripSit for the hard work that went into putting together the Guide to Drug Combinations , and we hope that it will be used wisely by those choosing to experiment with various drug combinations.
Disclaimer: Psychedelic Times presents this information with the sole intention of providing harm reduction information, and does not advocate or promote the use of illegal psychoactive substances. We advise our readers to use extreme caution when deciding whether or not to combine multiple substances.
About The Author
David Wilder
David Wilder is a writer covering topics like psychedelics, spirituality, technology, and self-development for Psychedelic Times, MERRY JANE, Reality Sandwich, Kahpi, and his blog ThinkWilder.com. When he’s not glued to a computer screen, he can be found reading science-fiction, dancing to live music, and trying to keep the plants in his garden alive.
Related Posts

Cannabis Crunch — Despite Trump Administration, Legalization Still Plows Forward… & All The Other Weed Craziness In January
February 5, 2018

The Evidence for Ibogaine: What New Studies Tell Us About Ibogaine for Addiction Treatment
February 9, 2016

Kicking the Habit: Psilocybin Mushrooms Proven to Help Long-Term Smokers Quit
September 9, 2015

The Safety of Dabbing: An Honest Terpene Story
December 15, 2017
Leave a reply
Your email address will not be published. Required fields are marked *
Subscribe for updates
Join our mailing list to receive the latest news from the psychedelic world.
You have Successfully Subscribed!
Recent posts.

- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Resources | Drugs
Drug Interactions: What You Should Know
(PDF version - 68KB)
There are more opportunities today than ever before to learn about your health and to take better care of yourself. It is also more important than ever to know about the medicines you take. If you take several different medicines, see more than one doctor, or have certain health conditions, you and your doctors need to be aware of all the medicines you take. Doing so will help you to avoid potential problems such as drug interactions.
Drug interactions may make your drug less effective, cause unexpected side effects, or increase the action of a particular drug. Some drug interactions can even be harmful to you. Reading the label every time you use a nonprescription or prescription drug and taking the time to learn about drug interactions may be critical to your health. You can reduce the risk of potentially harmful drug interactions and side effects with a little bit of knowledge and common sense. Drug interactions fall into three broad categories:
- Drug-drug interactions occur when two or more drugs react with each other. This drug-drug interaction may cause you to experience an unexpected side effect. For example, mixing a drug you take to help you sleep (a sedative) and a drug you take for allergies (an antihistamine) can slow your reactions and make driving a car or operating machinery dangerous.
- Drug-food/beverage interactions result from drugs reacting with foods or beverages. For example, mixing alcohol with some drugs may cause you to feel tired or slow your reactions.
- Drug-condition interactions may occur when an existing medical condition makes certain drugs potentially harmful. For example, if you have high blood pressure you could experience an unwanted reaction if you take a nasal decongestant.
Drug Interactions and Over-the-Counter Medicines
Over-the-counter (OTC) drug labels contain information about ingredients, uses, warnings and directions that is important to read and understand. The label also includes important information about possible drug interactions. Further, drug labels may change as new information becomes known. That's why it's especially important to read the label every time you use a drug.
- the name and amount of each active ingredient
- the purpose of each active ingredient
The " Uses " section of the label:
- tells you what the drug is used for
- helps you find the best drug for your specific symptoms
- when to talk to a doctor or pharmacist before use
- the medical conditions that may make the drug less effective or not safe
- under what circumstances the drug should not be used
- when to stop taking the drug
- the length of time and the amount of the product that you may safely use
- any special instructions on how to use the product
- required information about certain ingredients, such as sodium content, for people with dietary restrictions or allergies
- the name of each inactive ingredient (such as colorings, binders, etc.)
- provides telephone numbers of a source to answer questions about the product
Learning More About Drug Interactions
Talk to your doctor or pharmacist about the drugs you take. When your doctor prescribes a new drug, discuss all OTC and prescription drugs, dietary supplements, vitamins, botanicals, minerals and herbals you take, as well as the foods you eat. Ask your pharmacist for the package insert for each prescription drug you take. The package insert provides more information about potential drug interactions.
Before taking a drug, ask your doctor or pharmacist the following questions:
- Can I take it with other drugs?
- Should I avoid certain foods, beverages or other products?
- What are possible drug interaction signs I should know about?
- How will the drug work in my body?
- Is there more information available about the drug or my condition (on the Internet or in
- health and medical literature)?
Know how to take drugs safely and responsibly. Remember, the drug label will tell you:
- what the drug is used for
- how to take the drug
- how to reduce the risk of drug interactions and unwanted side effects
If you still have questions after reading the drug product label, ask your doctor or pharmacist for more information
Examples of Drug Interaction Warnings
The following are examples of drug interaction warnings that you may see on certain OTC drug products. These examples do not include all of the warnings for the listed types of products and should not take the place of reading the actual product label.
Back to top
This information is brought to you by the Council on Family Health in cooperation with the National Consumers League and the U.S. Food and Drug Administration.
ResourcesForYou
- Educational Resources: Ensuring Safe Use of Medicine
- Avoiding Drug Interactions
- Grapefruit Juice and Medicine May Not Mix
Drug Interaction Checker
Check interactions with multiple drugs, vaccines, supplements, alcohol, food and diseases.

Not all drugs interact, and not every interaction means you must stop taking one of your medications. Always consult your healthcare provider about how drug interactions should be managed before making any changes to your current prescription.
Drug Interaction FAQs
What is a drug interaction.
There are 3 main types of drug interactions to watch for:
Drug-drug interactions: This is the most common type of drug interaction and involves one drug interacting with another. If you take many medicines, your chances for this type of interaction increases. For example, taking two medicines that cause drowsiness at the same time can increase this side effect.
Drug-food and drug-drink interactions: Food and drinks can change how medicines work or worsen side effects when they are combined. Examples include beverages like grapefruit juice and statins causing muscle pain, or alcohol and opioids leading to dangerously slowed breathing.
Drug-disease interactions: Your medical conditions can affect the way a drug works or lead to side effects. For example, taking a nasal decongestant like pseudoephedrine if you have high blood pressure may worsen your high blood pressure.
What are common signs and symptoms of a drug interaction?
The signs and symptoms of a drug interaction can vary widely. Some symptoms may be minor, while others can be serious or life-threatening.
Common signs or symptoms of a drug interaction may include:
- Nausea or vomiting
- Muscle aches or pains
- Increased bruising or bleeding
- Abnormal heart rate
- Anxiety or restlessness
- Your medicine may not be working as well
If you think you may be experiencing a symptom or side effect due to a drug interaction, contact your healthcare provider right away for advice.
How can I avoid drug interactions?
Because you may not know if your drugs have any interactions, it's important to check for them before you start treatment.
Here are some tips on how to avoid drug interactions:
- Let your healthcare provider know about all the prescription medicines you take, plus any over-the-counter (OTC) medicines, including vitamins, herbal or dietary supplements.
- It may be helpful to keep a list of medicines with you that you can show at the pharmacy and at medical appointments.
- Talk to your healthcare provider and pharmacist about your medicines. Learn why you are taking it, how often you take it, and if you should avoid taking it with other medicines, alcohol, foods or drinks.
- Ask your doctor or pharmacist to check your drugs for any important drug interactions. Learn how to recognize the effects of any drug interactions.
- In case of a drug interaction, learn when you should call your doctor or 911 for emergency help.
All medicines come with written instructions. Follow those directions closely. Over-the-counter medicines also contain a Drug Facts label that helps to explain the medicine. Read this information carefully. If you do not understand your directions, ask a healthcare professional for help.
Can I eat or drink grapefruit with my medicine?
More and more medicines have interactions with food and drinks. Grapefruit and other juices can interfere with some medicines. In many cases it will cause the levels of drugs to increase in the blood, which can cause side effects.
Drug interactions with grapefruit juice are important because they occur with common medicines, like statins used to help lower cholesterol, drugs that help lower blood pressure or even treatments that fight cancer.
Your prescription bottle or other written information will explain if you should avoid grapefruit juice with your medicine. Your pharmacist may attach a special sticker to your bottle, or it may be found in printed instructions they give to you. If you have questions about food or drink interactions with your medicines, your pharmacist is a great resource.
Continue reading: Common grapefruit drug interactions
Can I drink alcohol with my prescribed medications?
Many medicines can have an interaction with alcohol, like wine, beer or spirits. This might interfere with your successful treatment or cause dangerous side effects. Mixing drugs like opioid pain medicines, sleeping pills or anxiety treatments with alcohol can be unsafe or even deadly. Always check to see if your medicines interact with alcohol before you combine the two.
Alcohol is itself a drug and may cause central nervous system side effects, like drowsiness, dizziness or fainting. When you combine it with other drugs that have similar side effects, your breathing may slow to dangerous or deadly levels. You might become unsteady and at risk for a fall or broken bone. Extra drowsiness can make it very dangerous for you to drive or perform hazardous activities.
Be sure to check your prescription drugs, as well as your over-the-counter (OTC) medicines, herbals, and dietary supplements like vitamins and minerals for alcohol interactions. Some cough and cold medicines may also contain alcohol, so be sure to check the labels.
Continue reading: Drug and alcohol interactions - what to avoid
Can herbs and supplements interact with my drugs?
While herbs and dietary supplements can be purchased over-the-counter (OTC) and may be labeled "all-natural", this does not always mean they are safe. Many of these products, just like prescription drugs, may have serious drug interactions.
For example, St. John's Wort, CoenzymeQ10, and even melatonin can interact with medicines like antidepressants, blood thinners like warfarin or even alcohol. These interactions can be just as serious as prescription medicines.
Because there's not always formal studies, some drug interactions with herbal products may not be known. Also, remember that herbal supplements are not subject to FDA review and have not usually been tested in clinical studies to prove their effectiveness or safety.
Your pharmacist can give you a better idea of what drug interactions may occur with any herbal or herbal dietary supplements you may be taking. Advice from your health care provider is your best option in preventing serious health effects from any drug interaction.
How do I check for drug interactions?
Checking with your healthcare provider is key in helping to prevent drug interactions.
You can also use the Drugs.com Drug Interaction Checker to learn more. This tool explains what the interaction is, how it occurs, the level of importance and how to handle the drug interaction. It will also display any interactions between your chosen drugs, food, beverages, or a medical condition.
Keep an up-to-date list of your medications, over-the-counter products, vitamins, herbals, and medical conditions. Share this list with your doctor, pharmacist, and nurse at each visit so that they can also screen for possible drug interactions.
Information is available for you to read, too. Review the Medication Guide, prescription information, warning labels, and Drug Facts Label with each new prescription or over-the-counter product you use.
Information may change as new information is learned about medications, so it's important to review the information frequently. Ask your pharmacist if you need a copy of any of this information.
What should I do if I find a drug interaction?
If you find you are at risk for an interaction, call your doctor or pharmacist. They will know if the interaction is serious and can recommend the next best step.
Luckily, most drug interactions can be prevented because your healthcare provider and pharmacist will screen for these before you start your medicine.
Be sure to let your healthcare team know about all of the medicines you take, including prescription drugs, OTC medicines, vitamins, and herbal and dietary supplements. Be sure not to stop taking any medicines without your doctor's approval first.
Medically reviewed by Leigh Ann Anderson, PharmD . Last updated on Oct 16, 2023.
- My Med List
- Interaction checker
- Pill identifier
- Compare drugs
- Medical Q & A
- Latest drug news

MARY CARPENTER, PharmD, HOLLY BERRY, PharmD, AND ALLEN L. PELLETIER, MD, Medical College of Georgia at Augusta University, Augusta, Georgia
Am Fam Physician. 2019;99(9):558-564
Related letter: Potential Drug Interactions in Patients Taking Oral Contraceptive Pills
Author disclosure: No relevant financial affiliations.
Drug interactions are common in the primary care setting and are usually predictable. Identifying the most important and clinically relevant drug interactions in primary care is essential to patient safety. Strategies for reducing the risk of drug-drug interactions include minimizing the number of drugs prescribed, re-evaluating therapy on a regular basis, considering nonpharmacologic options, monitoring for signs and symptoms of toxicity or effectiveness, adjusting dosages of medications when indicated, and adjusting administration times. Inhibition or induction of cytochrome P450 drug metabolizing isoenzymes is the most common mechanism by which clinically important drug interactions occur. The antimicrobials most likely to affect the international normalized ratio significantly in patients receiving warfarin are trimethoprim/sulfamethoxazole, metronidazole, and fluconazole. An empiric warfarin dosage reduction of 30% to 50% upon initiation of amiodarone therapy is recommended. In patients receiving amiodarone, limit dosages of simvastatin to 20 mg per day and lovastatin to 40 mg per day. Beta blockers should be tapered and discontinued several days before clonidine withdrawal to reduce the risk of rebound hypertension. Spironolactone dosages should be limited to 25 mg daily when coadministered with potassium supplements. Avoid prescribing opioid cough medicines for patients receiving benzodiazepines or other central nervous system depressants, including alcohol. Physicians should consider consultation with a clinical pharmacist when clinical circumstances require the use of drugs with interaction potential.
Drug interactions are estimated to cause approximately 2.8% of all hospitalizations annually in the United States, representing more than 245,000 hospitalizations, costing the health care system $1.3 billion. 1 Exact figures are unknown because few studies have highlighted the significance of drug interactions in primary care. Many interactions are theoretical or clinically trivial; however, some may have serious or life-threatening consequences. This review focuses on the most common drug interactions likely to be encountered in the primary care setting.
Physicians should be aware of common and serious drug interactions and prescribe to avoid these interactions where possible. Strategies for reducing the risk of drug-drug interactions include minimizing the number of drugs prescribed, re-evaluating therapy on a regular basis, considering nonpharmacologic options, monitoring for signs and symptoms of toxicity and/or effectiveness, adjusting dosages of medications when indicated, and adjusting administration times. 1 Physicians should monitor for early detection of adverse reactions and be aware of patient risk factors that increase the chance of an undesirable outcome.
Communication between primary care physicians and subspecialist physicians is critical to mutually understand the goals of drug therapy and to avoid or modify drug combinations that may put patients at risk. Patients should be educated about possible drug interactions when a reaction or potential adverse effect can be anticipated. Electronic drug information resources, as well as software that detects and alerts to a potential drug interaction (often built into electronic prescribing programs), lower the risk of some drug interactions but can cause alert fatigue. 2 Medication review and reconciliation by a pharmacist (especially during transitions of care) may reduce the risk of clinically significant drug interactions. 3 – 5 Physicians should consider consultation with a clinical pharmacist when clinical circumstances require the use of drugs with interaction potential.
Mechanisms of Drug-Drug Interactions
Drug-drug interactions can be pharmacodynamic or pharmacokinetic. Pharmacodynamic interactions occur when two drugs that are taken concomitantly have either additive or canceling effects on the body. Pharmacokinetic interactions occur when a drug affects the absorption, distribution, metabolism, or excretion characteristics of another drug. 6
Drug interactions based on altered metabolism are mostly attributable to effects on cytochrome P450 (CYP450) isozymes. Inhibition or induction of CYP450 drug metabolizing isozymes is the most common mechanism by which clinically important drug interactions occur. The most common isozyme is CYP3A4, followed by 2C19, 2C9, 1A2, 2E6, and 2D6. Drugs interacting with CYP450 isozymes can be classified as substrates, inducers, or inhibitors. Several drugs are substrates of transport-protein-complexes, such as P-glycoprotein (P-gp), which are expressed in hepatocytes and enterocytes, as well as in the epithelial cells of the renal tubules, the blood brain barrier, and the placenta. These transporters are subject to inhibition or induction that can elicit drug interactions. 6
Anticoagulation Interactions
Warfarin (Coumadin) inhibits vitamin K–dependent clotting factors and is metabolized by CYP450 isozymes. A wide range of drugs, including over-the-counter and herbal products, interact with warfarin. 7 Warfarin interactions can increase patients’ risk for major bleeding or thrombotic complications. Vitamin K ingestion modulates warfarin’s effects on coagulation, making a discussion of food-drug interactions with patients essential. Information for patients about warfarin interactions with foods and herbal products can be found at https://www.ihtc.org/warfarin-dietary-tips/ . 8 Drugs that affect vitamin K (directly or indirectly) or alter warfarin metabolism may have a significant effect on the international normalized ratio (INR). Drugs that affect other parts of the coagulation system (e.g., platelets) when used in conjunction with warfarin may also affect risk of bleeding or thrombosis. Awareness of these interactions is critical to safely managing patients receiving warfarin. Collaborative care with pharmacists in anticoagulation clinics has been demonstrated to improve patient safety and outcomes. 3
WARFARIN AND ANTIMICROBIALS
Antimicrobials can inhibit CYP450 isozymes, alter protein binding, and diminish absorption of vitamin K by altering the gut flora. 9 Protein-binding and metabolism alterations of warfarin are the mechanisms of interaction that pose clinical significance. The antimicrobials most likely to affect the INR significantly are trimethoprim/sulfamethoxazole, metronidazole (Flagyl), and fluconazole (Diflucan). Other antimicrobials such as ciprofloxacin, levofloxacin (Levaquin), azithromycin (Zithromax), and clarithromycin (Biaxin) may affect the INR; however, the effects are variable and tend to be patient specific. 9
Antimicrobial agents with a lower likelihood of affecting the INR include penicillin G benzathine, clindamycin, and first- and fourth-generation cephalosporins. 9
Empiric warfarin dosage adjustments should be considered with concomitant use of trimethoprim/sulfamethoxazole, rifampin, fluconazole, and/or metronidazole. 10 , 11 Considerable variability in patient-specific response occurs; knowledge of previous exposure and response should be considered. Regardless of the antimicrobial, the INR should be checked within three to five days of initiation and within three to five days after discontinuation of the antimicrobial. 12 Interactions and management strategies for the antimicrobials that consistently interact with warfarin are provided in Table 1 . 9 – 12
WARFARIN AND AMIODARONE
The interaction between warfarin and amiodarone is mediated by inhibition of CYP2C9, 1A2, and 3A4 enzymes, leading to increased warfarin concentrations and increased bleeding risk. 13 , 14 The effects of this interaction are typically seen within the first few days; however, amiodarone has a long half-life so several warfarin adjustments may be needed before the INR has completely stabilized. 15 An empiric warfarin dosage reduction of 30% to 50% upon initiation of amiodarone therapy is recommended, followed by several weeks of weekly monitoring of the INR to ensure warfarin dosing remains optimal.
WARFARIN AND STATINS
Fluvastatin (Lescol), lovastatin (Mevacor), rosuvastatin (Crestor), and simvastatin (Zocor) inhibit warfarin metabolism by the inhibition of CYP2C9, leading to increased warfarin concentrations and increased bleeding risk. 16 Atorvastatin (Lipitor) and pravastatin (Pravachol) appear to be safer alternatives. If these statins are not appropriate for treating a patient’s lipids, the patient’s INR should be monitored more frequently, and warfarin dosage adjustments should be performed accordingly. 17
WARFARIN AND NONSTEROIDAL ANTI-INFLAMMATORY DRUGS
Nonsteroidal anti-inflammatory drugs (NSAIDs) increase gastric irritation and erosion of the protective lining of the stomach, potentially leading to the formation of gastrointestinal ulcers, which could result in gastrointestinal bleeding. These effects in combination with the anticoagulant effect of warfarin increase the risk of bleeding without affecting the INR. 18 , 19 The cyclooxygenase-2 inhibitor, celecoxib (Celebrex), does not affect platelet function and is associated with less gastrointestinal erosion. Literature correlating gastrointestinal bleeding risk with celecoxib use is limited. Patients should be educated to report abdominal pain or signs and symptoms of gastrointestinal bleeding to their physician when taking warfarin concomitantly with any NSAID. 20 – 22
If concomitant therapy with warfarin and aspirin/dipyridamole (Aggrenox) is necessary, the dosage of aspirin/dipyridamole should be limited to 100 mg per day or less to minimize bleeding risk. 18 It is preferable to use alternatives to NSAIDs, such as acetaminophen, topical therapy, or judiciously prescribed opioid analgesics when indicated. Acetaminophen does not alter platelet function, but concomitant use may increase the pharmacodynamic effect of warfarin, increasing the INR. To be cautious, limit the acetaminophen dosage to 2 g per day for no more than seven days and complete more frequent INR testing. 18
DIRECT ORAL ANTICOAGULANT INTERACTIONS
Direct oral anticoagulant interactions inhibit factor Xa (rivaroxaban [Xarelto], apixaban [Eliquis], edoxaban [Savaysa]) or directly inhibit thrombin (dabigatran [Pradaxa]). 23 Direct oral anticoagulant interactions are attractive alternatives to warfarin for some indications because of their ease of administration, no requirement for INR monitoring, no interaction between vitamin K or food, and comparable effectiveness and safety profiles. 24 However, clinically significant interactions occur with drugs that share common metabolic pathways with direct oral anticoagulant interactions. 23 Drugs that inhibit both CYP3A4 and P-gp can pose the greatest interaction and increase bleeding risk with direct oral anticoagulant interactions. Drugs that may increase bleeding risk include ketoconazole, ritonavir (Norvir), fluconazole, and amiodarone. 23 , 25 Specific dosing adjustments for the various direct oral anticoagulant interactions are found in Table 2 . 26 – 29
Statin Interactions
Amiodarone inhibits CYP3A4, which may decrease metabolism of certain statin drugs and increase the risk of statin-related muscle toxicity. Predisposing risk factors for muscle toxicity include age (older than 65 years), obesity, and renal/hepatic impairment. 30 , 31 Fluvastatin and pravastatin are metabolized through alternative pathways that do not affect amiodarone metabolism and are recommended over simvastatin and atorvastatin. When alternative statins are not appropriate, limit dosages of simvastatin to 20 mg per day or lovastatin to 40 mg per day when used concomitantly with amiodarone. 31
AZOLE ANTIFUNGALS
Azole antifungals inhibit CYP3A4, which is necessary in the metabolism of simvastatin, lovastatin, and, to a lesser degree, atorvastatin. Azole antifungals also inhibit CYP2C9, which is responsible for the metabolism of fluvastatin. These interactions can lead to an increase in statin concentration, thus increasing the risk of muscle toxicity. 32 , 33 Atorvastatin undergoes less metabolism by CYP3A4, but some cases of myopathy with CYP3A4 inhibitors have been reported. 34 Management options include use of rosuvastatin or pravastatin, which are not metabolized by CYP3A4, or use of an alternative antifungal such as terbinafine (Lamisil). 35
CALCIUM CHANNEL BLOCKERS
The exact mechanism for the interaction between calcium channel blockers and statin drugs is unknown; however, inhibition of CYP3A4 metabolism may play a role. 36 These interactions and management strategies, including specific dosage recommendations with concomitant simvastatin, are found in Table 3 . 36 , 37
Phosphodiesterase-5 and Nitrates
Phosphodiesterase-5 inhibitors may markedly increase the hypotensive effects of nitrates. Both nitrates and phosphodiesterase-5 inhibitors exert their effects by potentiating the vasodilatory effects of cyclic guanosine monophosphate, which is believed to be responsible for the hypotensive effects when these agents are administered concomitantly.
Phosphodiesterase-5 inhibitors are contraindicated in patients already receiving nitrates. However, 2013 guidelines for management of ST-segment elevation myocardial infarction and unstable angina/non-ST-segment elevation myocardial infarction published by the American College of Cardiology Foundation and American Heart Association support the administration of nitrates when medically necessary at least 24 hours after sildenafil (Viagra) or vardenafil (Levitra) or 48 hours after tadalafil (Cialis). 38
Clonidine and Beta Blockers
Several reports describe an increased hypertensive response to the withdrawal of clonidine when a beta blocker is being used. 39 In the presence of a beta2-receptor blockade, the vasoconstrictor properties of the catecholamines are unopposed, resulting in the exaggerated hypertensive response within 24 to 72 hours after discontinuation of clonidine. 39 Beta blockers should be tapered and discontinued several days before clonidine withdrawal to reduce the risk of rebound hypertension. Recommendations call for decreasing the dosage of clonidine over several days before discontinuation. 40
Drugs with Chelation Risk
Chelation occurs when insoluble complexes are formed in the gut as a result of coadministration of multivalent cations and tetracycline drugs, fluoroquinolone antibiotics, or thyroid drugs. When these complexes form, the absorption of these drugs is reduced. 18 Managing dosing times for tetracycline antibiotics (administer two hours before or at least four hours after cation 41 ), fluoroquinolone antibiotics (administer two hours before or six hours after cation 42 ), and thyroid drugs (administer two hours before or six hours after cation 42 ) helps to minimize these drug interactions. Many cations are present in over-the-counter products ( Table 4 40 ) . It is important to inquire about the use of over-the-counter medications because patients may not initially report usage. 43
Potassium supplements coadministered with angiotensin-converting-enzyme inhibitors, angiotensin II receptor blockers, direct renin inhibitors, or potassium-sparing diuretics can increase the risk of hyperkalemia. This is considered a pharmacodynamic interaction, and the combination should be used with caution. If the combination is necessary, the spironolactone dosage should be limited to 25 mg daily when coadministered with potassium supplements. 44 – 46 Monitoring should be performed; if serum potassium levels increase to greater than 5.5 mEq per L (5 mmol per L) or renal function worsens, doses of these antihypertensive drugs should be held until the potassium level is less than 5 mEq per L (5 mmol per L) and the renal function normalizes for at least 72 hours. 45 , 46
Combination of Drugs That Prolong the QTc Interval
QT prolongation syndrome increases the risk of torsades de pointes, a life-threatening arrhythmia. Although torsades de pointes is rare, its severity warrants a discussion of risk factors and the likelihood of occurrence ( Table 5 ) . 47 Torsades de pointes is most likely to occur when two or more QT interval–prolonging drugs are administered to a patient who is already at high risk for arrhythmia. 47 , 48
Table 6 48 – 51 includes a list of drugs that may cause QT prolongation. Avoiding the combination of drugs from the highest or moderate risk group is advised, especially in patients with a significant history of cardiac events. If unavoidable, monitoring with electrocardiography soon after initiation and yearly thereafter while continuing concomitant therapy is advised. 49 , 51 The U.S. Food and Drug Administration guidance regarding QT prolongation defines increases greater than 20 msec as a substantial risk for developing torsades de pointes. 50
Combination of Central Nervous System Depressing Agents
Health care professionals should limit prescribing medications that can depress the central nervous system. These agents should be combined only if alternative treatment options are inadequate. If these medicines are prescribed together, limiting the dosages and duration of each medication is preferable. 52 Prescribing opioid cough medicines for patients receiving benzodiazepines or other central nervous system depressants, including alcohol, should also be avoided. 53 , 54 Patients and caregivers should be educated about signs of central nervous system depression, which include, but are not limited to, slowed or difficulty breathing and/or sedation. A list of drugs predisposing patients to central nervous system depression is provided in Table 7 . 50 , 52 , 53
This article updates a previous article by Ament, Bertolino, and Liszewski . 18
Data Sources: We searched PubMed and Web of Science between January 2017 and June 2018, using the search terms drug interaction(s), drug-drug interaction(s), and the MeSH headings drug interactions and food-drug interactions in combination with one or more of the following terms: warfarin, direct oral anticoagulants, novel oral anticoagulants, amiodarone, antimicrobials, antibiotics, statin(s), PDE-5, clonidine, chelator(s), hyperkalemia, QTc prolongation, central nervous system, CNS. The term primary care or the MeSH term primary health care was also employed. Additional resources were identified through Essential Evidence Plus. A literature search using the methods described was performed in June 2018 and January 2019 that limited publication dates between January 2015 through May 2018 and January 2015 through December 2018, respectively, to identify recent publications.
Nikolic B, Jankovic S, Stojanov O, Popovic J. Prevalence and predictors of potential drug-drug interactions. Cent Eur J Med. 2014;9(2):348-356.
Yeh ML, Chang YJ, Wang PY, Li YC, Hsu CY. Physicians’ responses to computerized drug-drug interaction alerts for outpatients. Comput Methods Programs Biomed. 2013;111(1):17-25.
Ansell J, Hirsh J, Dalen J, et al. Managing oral anticoagulant therapy. Chest. 2001;119(1 suppl):22S-38S.
Mekonnen AB, McLachlan AJ, Brien JA. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: a systematic review and meta-analysis. BMJ Open. 2016;6(2):e010003.
Manzoor BS, Cheng WH, Lee JC, Uppuluri EM, Nutescu EA. Quality of pharmacist-managed anticoagulation therapy in long-term ambulatory settings: a systematic review. Ann Pharmacother. 2017;51(12):1122-1137.
Tannenbaum C, Sheehan NL. Understanding and preventing drug-drug and drug-gene interactions. Expert Rev Clin Pharmacol. 2014;7(4):533-544.
Bungard TJ, Yakiwchuk E, Foisy M, Brocklebank C. Drug interactions involving warfarin: practice tool and practical management tips. Can Pharm J. 2011;144(1):21-25:e9.
Indiana Hemophilia & Thrombosis Center, Inc. Warfarin dietary tips. https://www.ihtc.org/warfarin-dietary-tips/ . Accessed February 6, 2019.
Lane MA, Zeringue A, McDonald JR. Serious bleeding events due to warfarin and antibiotic co-prescription in a cohort of veterans. Am J Med. 2014;127(7):657-663:e2.
Holt RK, Anderson EA, Cantrell MA, Shaw RF, Egge JA. Preemptive dose reduction of warfarin in patients initiating metronidazole. Drug Metabol Drug Interact. 2010;25(1-4):35-39.
Ahmed A, Stephens JC, Kaus CA, Fay WP. Impact of preemptive warfarin dose reduction on anticoagulation after initiation of trimethoprimsulfamethoxazole or levofloxacin. J Thromb Thrombolysis. 2008;26(1):44-48.
Therapeutic Research Center. Antimicrobial drug interactions with warfarin. PL Detail-Document #280806: Pharmacist’s letter/prescriber’s letter, August 2012. http://prescribersletter.therapeuticresearch.com/pl/ArticlePDF.aspx?cs=&s=PRL&DocumentFileID=0&DetailID=280823&SegmentID=0 . Accessed September 25, 2018.
Hamer A, Peter T, Mandel WJ, Scheinman MM, Weiss D. The potentiation of warfarin anticoagulation by amiodarone. Circulation. 1982;65(5):1025-1029.
Kerin NZ, Blevins RD, Goldman L, Faitel K, Rubenfire M. The incidence, magnitude, and time course of the amiodarone-warfarin interaction. Arch Intern Med. 1988;148(8):1779-1781.
Sanoski CA, Bauman JL. Clinical observations with the amiodarone/warfarin interaction: dosing relationships with long-term therapy. Chest. 2002;121(1):19-23.
Sconce EA, Khan TI, Daly AK, Wynne HA, Kamali F. The impact of simvastatin on warfarin disposition and dose requirements. J Thromb Hae-most. 2006;4(6):1422-1424.
Simonson SG, Martin PD, Mitchell PD, et al. Effect of rosuvastatin on warfarin pharmacodynamics and pharmacokinetics. J Clin Pharmacol. 2005;45(8):927-934.
Ament PW, Bertolino JG, Liszewski JL. Clinically significant drug interactions. Am Fam Physician. 2000;61(6):1745-1754.
Brouwers JR, de Smet PA. Pharmacokinetic-pharmacodynamic drug interactions with nonsteroidal anti-inflammatory drugs. Clin Pharmacokinet. 1994;27(6):462-485.
Schwartz JI, Agrawal NG, Hartford AH, et al. The effect of etoricoxib on the pharmacodynamics and pharmacokinetics of warfarin. J Clin Pharmacol. 2007;47(5):620-627.
Karim A, Tolbert D, Piergies A, et al. Celecoxib does not significantly alter the pharmacokinetics or hypoprothrombinemic effect of warfarin in healthy subjects. J Clin Pharmacol. 2000;40(6):655-663.
Battistella M, Mamdami MM, Juurlink DN, et al. Risk of upper gastrointestinal hemorrhage in warfarin users treated with nonselective NSAIDs or COX-2 inhibitors. Arch Intern Med. 2005;165(2):189-192.
Voukalis C, Lip GY, Shantsila E. Drug-drug interactions of non-vitamin K oral anticoagulants. Expert Opin Drug Metab Toxicol. 2016;12(12):1445-1461.
Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation. Lancet. 2014;383(9921):955-962.
Chang SH, Chou IJ, Yeh YH, et al. Association between use of nonvitamin K oral anticoagulants with and without concurrent medications and risk of major bleeding in nonvalvular atrial fibrillation. JAMA. 2017;318(13):1250-1259.
Xarelto (rivaroxaban) [prescribing information]. Titusville, N.J.: Janssen Pharmaceuticals, Inc. Updated August 2018. http://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/XARELTO-pi.pdf . Accessed January 28, 2019.
Eliquis (apixaban) [prescribing information]. Princeton, N.J.: Bristol-Myers Squibb Company; New York, NY: Pfizer Inc. Updated June 2018. https://packageinserts.bms.com/pi/pi_eliquis.pdf . Accessed January 28, 2019.
Pradaxa (dabigatran etexilate) [prescribing information]. Ridgefield, Conn.: Boehringer Ingelheim Pharmaceuticals, Inc. Updated March 2018. https://docs.boehringer-ingelheim.com/Prescribing%20Information/PIs/Pradaxa/Pradaxa.pdf . Accessed January 28, 2019.
Härtter S, Sennewald R, Nehmiz G, Reilly P. Oral bioavailability of dabigatran etexilate (Pradaxa(®)) after co-medication with verapamil in healthy subjects. Br J Clin Pharmacol. 2013;75(4):1053-1062.
Cordarone (amiodarone) [prescribing information]. Philadelphia, Pa.: Wyeth Pharmaceuticals, Inc. Updated April 2017. http://labeling.pfizer.com/showlabeling.aspx?id=93 . Accessed January 28, 2019.
Becquemont L, Neuvonen M, Verstuyft C, et al. Amiodarone interacts with simvastatin but not with pravastatin disposition kinetics. Clin Pharmacol Ther. 2007;81(5):679-684.
Findling O, Meier N, Sellner J, Nedeltchev K, Arnold M. Clinical reasoning: rhabdomyolysis after combined treatment with simvastatin and fluconazole. Neurology. 2008;71(15):e34-e37.
Lescol (fluvastatin) [prescribing information]. East Hanover, N.J.: Novartis Pharmaceuticals Corporation. Updated August 2017. https://www.pharma.us.novartis.com/sites/www.pharma.us.novartis.com/files/Lescol.pdf . Accessed January 28, 2019.
Kahri J, Valkonen M, Bäcklund T, Vuoristo M, Kivistö KT. Rhabdomyolysis in a patient receiving atorvastatin and fluconazole. Eur J Clin Pharmacol. 2005;60(12):905-907.
Kantola T, Backman JT, Niemi M, Kivistö KT, Neuvonen PJ. Effect of fluconazole on plasma fluvastatin and pravastatin concentrations. Eur J Clin Pharmacol. 2000;56(3):225-229.
Jacobson TA. Comparative pharmacokinetic interaction profiles of pravastatin, simvastatin, and atorvastatin when coadministered with cytochrome P450 inhibitors. Am J Cardiol. 2004;94(9):1140-1146.
Zocor (simvastatin) [prescribing information]. Whitehouse Station, N.J: Merck & Co., Inc. Updated February 2018. https://www.merck.com/product/usa/pi_circulars/z/zocor/zocor_pi.pdf . Accessed January 28, 2019.
O’Gara PT, Kushner FG, Ascheim DD, et al.; American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol. 2013;61(4):e78-e140.
Bailey RR, Neale TJ. Rapid clonidine withdrawal with blood pressure overshoot exaggerated by beta-blockade. Br Med J. 1976;1(6015):942-943.
Catapres-TTS (clonidine) [prescribing information]. Ridgefield, Conn.: Boehringer Ingelheim Pharmaceuticals, Inc. Updated August 2016. https://docs.boehringer-ingelheim.com/Prescribing%20Information/PIs/Catapres%20Tabs/CatapresTabs.pdf . Accessed January 28, 2019.
Healy DP, Dansereau RJ, Dunn AB, et al. Reduced tetracycline bioavailability caused by magnesium aluminum silicate in liquid formulations of bismuth subsalicylate. Ann Pharmacother. 1997;31(12):1460-1464.
Hansten PD, Horn JR. Top 100 Drug Interactions 2018: A Guide to Patient Management. 2018 ed. Freeland, Wash.: H&H Publications; 2017:vii-177.
Qato DM, Alexander GC, Conti RM, et al. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 2008;300(24):2867-2878.
Blaustein DA, Babu K, Reddy A, Schwenk MH, Avram MM. Estimation of glomerular filtration rate to prevent life-threatening hyperkalemia due to combined therapy with spironolactone and angiotensin-converting enzyme inhibition or angiotensin receptor blockade. Am J Cardiol. 2002;90(6):662-663.
Schepkens H, Vanholder R, Billiouw JM, Lameire N. Life-threatening hyperkalemia during combined therapy with angiotensin-converting enzyme inhibitors and spironolactone: an analysis of 25 cases. Am J Med. 2001;110(6):438-441.
Aldactone (spironolactone) [prescribing information]. New York, NY: Pfizer Inc. Updated April 2018. http://labeling.pfizer.com/ShowLabeling.aspx?id=520 . Accessed January 28, 2019.
Letsas KP, Efremidis M, Kounas SP, et al. Clinical characteristics of patients with drug-induced QT interval prolongation and torsade de pointes. Clin Res Cardiol. 2009;98(4):208-212.
Yap YG, Camm AJ. Drug induced QT prolongation and torsades de pointes. Heart. 2003;89(11):1363-1372.
Chadwick B, Waller DG, Edwards JG. Potentially hazardous drug interactions with psychotropics. Adv Psychiatr Treat. 2005;11(6):440-449.
U.S. Department of Health and Human Services, U.S. Food and Drug Administration, Center for Drug Evaluation and Research, and Center for Biologics Evaluation and Research. Guidance for Industry. E14 Clinical Evaluation of QT/QTc Interval Prolongation and Proarrhythmic Potential for Non-Antiarrhythmic Drugs; 2017. https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM073161.pdf . Accessed October 30, 2018.
Owens RC, Ambrose PG. Torsades de pointes associated with fluoroquinolones. Pharmacotherapy. 2002;22(5):663-668 , discussion 668-672.
Park TW, Saitz R, Ganoczy D, et al. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: case-cohort study. BMJ. 2015;350:h2698.
U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA warns about serious risks and death when combining opioid pain or cough medicines with benzodiazepines; requires its strongest warning; August 31, 2016. Updated Spetember 20, 2017. http://www.fda.gov/Drugs/Drugsafety/ucm518473.htm . Accessed March 15, 2019.
Wiese K, Ellingrod VL. Avoiding common drug-drug interactions. Curr Psychiatr. 2015;14(7):21-32.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2019 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
2C-B: Effects, Dosage, & Safety
The middle ground between MDMA & LSD.
Trip Sitter Safe 2C-B Guidelines
What’s the dose of 2c-b, what does 2c-b feel like, does 2c-b have medical value, can 2c-b cause a bad trip, does 2c-b cause a hangover, how long does 2c-b last, how is 2c-b used, other members of the 2c- family, 2c-b vs. lsd, 2c-b vs. mescaline, 2c-b vs. mdma, 2c-b adulteration, 2c-b & drug interactions, 2c-b side-effects, is 2c-b addictive, is 2c-b legal, how 2c-b works, 1. how do i test the purity of 2c-b, 2. will 2c-b show up on a drug test, 3. is 2c-b dangerous, 4. can i microdose 2c-b, subscribe to get a weekly dose of psychedelics in your inbox.
Everybody has heard of MDMA (ecstasy) and LSD (lysergic acid diethylamide) — they’ve become staples in the world of mind-altering substances.
But there’s another popular psychoactive substance that’s been residing in the shadows since the 1980s. This substance is called 2C-B.
The effects of 2C-B are often described as being a mid-point between the empathogenic effects of MDMA and the hallucinogenic effects of LSD.
So what exactly is 2CB? Is it safe?
In this article, we’ll cover everything you need to know about 2C-B — including how it works, what it feels like, and how to use it safely.
What is 2C-B?
2C-B (4-bromo-2,5-dimethoxyphenethylamine) is a synthetic psychedelic substance derived from mescaline. It was invented in 1974 by a man named Alexander Shulgin — the godfather of MDMA and creator of the entire 2C- family of substances.
Shulgin invented well over 200 psychoactive compounds in his research lab dubbed “The Farm.”
Shulgin considered 2C-B to be one of his greatest creations. In one of his books — PiHKAL (phenethylamines I Have Known And Loved) — he listed 2C-B among his “magic half dozen”.
The other five include mescaline, DOM, 2C-E, 2C-I, 2C-T2 , and 2C-T7 .
The effects of 2C-B have been described as a combination between LSD and MDMA — but this is a simplification. In reality, the 2C-B experience is entirely unique.
The qualities of 2C-B made it popular as a sex-enhancement drug in the 80s. The German pharmaceutical company Drittewelle started producing the drug under the name “Nexus.” It was sold in sex shops as a way to boost libido, sexual connection and increase stamina and energy. 2C-B is still considered by many to be the best psychedelic to use during sex of all time.
In Shulgin’s own words , “[2C-B] is, in my opinion, one of the most graceful, erotic, sensual, introspective compounds I have ever invented.”
2C-B reached mainstream popularity sometime after 1985 when MDMA was officially banned. It was used as a legal alternative to MDMA. 2C-B and the rest of the 2C- family were later banned in 1995.
2C-B: Specs & Technical Details
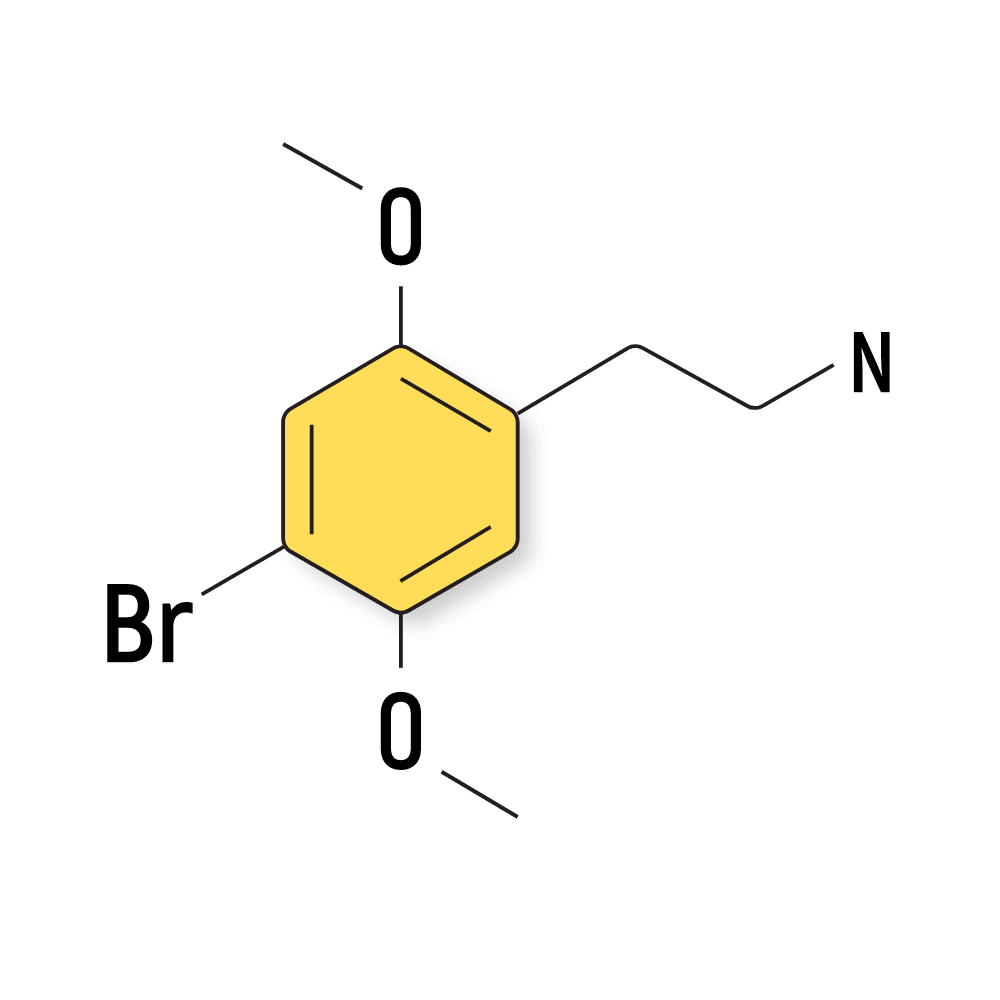
- 🐍 I understand why psychedelics should be treated with respect
- ⚖️ I’m familiar with the laws surrounding psychedelics in my country & state
- 🍄 I’m familiar and confident in the dose I’m taking (dose range for 2C-B is 5-20 mg)
- 🧪 I’ve tested a sample of the substance I’m using with a drug testing kit
- 💊 I’m not mixing any medications or other substances with 2C-B
- 🏔 I’m in a safe & comfortable environment with people I trust
- 🐺 One of the members of my group is responsible and sober (AKA a trip sitter )
- 📆 I have nothing important scheduled for after the trip
- 🧠 I’m in a sound & healthy state of mind
- 🌶 I’m aware of the increased risk of heatstroke & dehydration with this compound
- 📚 I’m familiar with the four pillars of responsible psychedelic use — set, setting, sitter, & substance .
- ⏳ Know the timeline — the effects of 2C-B can last between 4 and 8 hours
- 🙅♀️ Know when to avoid stimulants — don’t take 2C-B if you have underlying heart, neurological, or psychiatric disorders
The dosage range for 2C-B is between 5 mg and 35 mg. Most tablets or capsules contain 5 mg of 2C-B each.
Lower doses of around 5 mg have effects most similar to MDMA or Adderall, while the higher doses (more than 15 mg) offer formidable hallucinogenic effects comparable to LSD, psilocybin, or mescaline.
The dosage range of 2C-B includes:
- 1 mg — Microdose
- 5 mg — Threshold dose (stimulant-like effects)
- 5–20 mg — Standard psychoactive dose (hallucinogenic & stimulant effects)
- 20–35 mg — High psychedelic dose (strong hallucinogenic & stimulant action)
- 35–60 mg — Heroic dose (unpredictable effects, not recommended)
2C-B has a high level of safety. Shulgin, the inventor of the drug, reportedly took 100 mg by accident. This is a dose nearly three times what’s considered a high dose for the substance. He didn’t suffer any severe side effects from the experience.
With that said, higher doses can be intense. Most people who use more than 35 or 40 mg of the drug report intense, often scary, or confronting hallucinations.
The higher the dose, the stronger the visuals. Some could even describe the visuals at higher doses to be “cartoon-like” — which is similar to the visuals experienced with higher doses of mescaline.
The effects of 2C-B could be described as a combination of MDMA and LSD.
While there’s truth to this, it’s not perfectly accurate. 2C-B has empathogenic effects like MDMA and hallucinogenic effects like LSD — but the experience is unique in and of itself. The overall effects of 2C-B share much more resemblance to mescaline.
As part of our ongoing experience surveys, we ask our readers to share their experiences to better understand the effects and common dosages of substances.
Most of the responses we’ve received throughout our 2C-B survey had a positive sentiment. Many people taking part in our surveys and in the psychedelic community at large consider 2C-B to be their favorite psychedelic.
Commonly 2C-B Experiences Include:
- Increased energy (92%)
- A greater sense of empathy with others (86%)
- Introspection (80%)
- Visual hallucinations (78%)
- Sexual arousal (78%)
- Laughter (76%)
- Auditory hallucinations (67%)
- Ego death or dissolution (65%)
2C-B is most often used in place of MDMA at concerts, parties, or music festivals. The stimulating and euphoric effects make people feel more social and engaged, it creates a strong sense of empathy and connectedness with other people, and it won’t inhibit your ability to sleep at the end of the night.
Here’s what you can expect to feel while taking 2C-B:
Introspection
Users often report feelings of introspection, ego-dissolution , and a stronger sense of empathy and connection with others. It’s not uncommon for people using 2C-B to come to some sort of “realization” about their life. This realization may remain after the trip, but it may also be forgotten.
In a clinical setting, 2C-B is thought to connect the user with former emotions and repressed memories.
Hallucinations
2C-B is a hallucinogen through and through. In smaller doses these effects are limited, but higher doses of 2C-B produce intense changes in sensory perception . This includes sight, sound, and touch.
The visuals of 2C-B remind me of the videogame Borderlands — where some details pop much more than others and make the world look almost as though it was traced over with a pencil
Sometimes 2C-B can feel a little bit “speedy” or “tweaky” — especially in the higher doses.
2C-B is also used for its sexual-enhancement purposes as a way to explore a deeper connection between partners and enhance libido and physical stamina.
- Disorientation
Reports from people who took part in our survey that used very high doses (40 mg or higher) or mixed 2C-B with other psychedelics like LSD or psilocybin often mention the experience to be “disorientating” (37%).
2C-B isn’t used medically because of its current standing as a Schedule I substance in the United States. It’s classified under equivalent filings in other countries, such as the United Kingdom, Canada, Australia, Germany, and Europe.
The drug’s creator, Alexander Shulgin, suggested 2C-B was a good follow-up treatment in psychotherapy after MDMA. He suggested 2C-B as a way to open up the emotional, intuitive and archetypal area of your psyche to help solve the problems uncovered during the MDMA session.
More research is needed before we can make any reasonable assumptions about the potential for using 2C-B in psychotherapy.
Yes, 2C-B is a strong psychedelic — especially in higher doses. However, when used within the standard psychoactive range (5–15 mg), 2C-B is unlikely to lead to what can be considered a “bad trip.”
The higher you go over the 15 mg dose, the more likely you are to experience challenging or uncomfortable experiences. The hallucinations on 2C-B can escalate very quickly at higher doses.
Sometimes, bad trips are the result of adulterants (ingredients you weren’t expecting to be in there). Samples of 2C-B have been shown to contain substances such as methamphetamines, MDA, PMA, PMMA, NBOMe , or various opiates.
You should also always test a sample of your 2C-B using a reagent test liquid before you use it. It’s impossible to know what’s in a pill or powder without testing.
Testing 2C-B is very easy to do, it’s cheap, and it only requires you to sacrifice trace amounts of your tablet or powder — only a sample the size of a grain of sand is necessary to run the safety tests that could save your life.
One of the biggest benefits of using 2C-B over MDMA is the lack of a hangover the following morning.
Of our respondents, only 7% reported any negative impact the following morning after using doses lower than 35 mg of 2C-B. A big reason for this comes down to the fact that 2C-B rarely interferes with sleep. Getting a good night of rest after using 2C-B is one of the best ways to avoid hangovers.
With that said, hangovers are still possible — and are especially common with the higher doses. Of the survey respondents that too more than 35 mg of 2C-B, nearly 28% of them had a hangover the following morning.
The best way to avoid a 2C-B hangover is to drink plenty of water throughout the experience and ensure you’re getting a full 8 hours of sleep afterward. Taking some electrolytes or magnesium before you go to bed can go a long way as well.
2C-B usually lasts between 4 and 8 hours.
The effects usually begin to appear within about 45 minutes to an hour after taking it and peak around the 2-hour mark.
Peak effects last between 1 and 2 hours before tapering off. The comedown on 2C-B is very slow and gradual — which is considered one of the advantages of this substance. Most amphetamines or other stimulants tend to produce a rapid comedown — which can make users feel depressed. 2C-B is much more gradual and gentle.
2C-B comes as either a white crystalline powder or pressed tablets.
Tablets contain either 5, 10, 20, or 25 mg of 2C-B each — so a normal dose can range anywhere from 1–7 tablets. Always check the dose of your tablet before you take it.
The powder is usually used in a “parachute” — which involves weighing the dose of powder on a small scale and wrapping it up into a rolling paper. This is then taken just like you would a capsule, by essentially swallowing it whole.
Other people prefer to fill their own capsules using the raw powder or snorting it (insufflation). Be very careful when snorting any substance. The effects will be much stronger and appear much more quickly. Take a lower dose than you normally would and give it time to take effect. It’s easy to take too much using this method.
In general, we advise against snorting any substance. It’s far too easy to take too much, and it can be extremely damaging to the nasal cavity.
Additionally, always weigh your dose using a small scale if you’re taking the raw powder. Never attempt to eyeball your dose of 2C-B of any powdered drugs. Scales are cheap (less than $20) and could mean the difference between having a positive experience and ending up in a hospital.
2C-B can also be vaporized — but this isn’t a common way of using it, and the long-term health effects of taking 2C-B this way aren’t well understood. Many compounds will change when heated like this, and the byproducts of vaporized 2C-B are not well understood.
It’s best to stick to the tried and tested oral route when taking 2C-B.
2C-B is just one of many substances in its family. Most of them were invented around the same time by Alexander Shulgin and documented in one of his books PiHKAL .
All 2C- substances contain methoxy groups on the 2 and 5 positions of a benzene ring of its chemical structure. They each have a unique chemical group attached to the 4th position on the benzene ring, which is what differentiates them in terms of their chemical structure and effect profile.
When various government regulators started banning 2C-B, they did so by banning the entire 2C-x family — as defined by the chemical structure above.
The most notable members of the 2C- family include:
- 2C-B — this is by far the most popular member of the family.
- 2C-C — this 2c compound differentiates itself through its relaxing, even mild sedative action and powerful visuals.
- 2C-E — this 2C compound is milder than 2C-B, has a slightly higher likelihood of side effects, and lasts about 3 hours longer.
- 2C-I — these substances tend to produce effects similar to LSD but less introspective. The most common is 2C-I-NBOMe, which has been proven to be dangerous & should be avoided
- 2C-P — a strong, but mellow psychedelic with empathogen underpinnings.
- 2C-T — there are several iterations of this compound, including 2C-T-2, 2C-T-3, 2C-T-4, 2C-T-7, & 2C-T-16. The most popular, by far, is 2CT-7.
List of all 2C-Substances
How strong is 2c-b vs. other psychedelics.
The intensity of effects from 2CB increases steadily along with the dose.
Lower doses (5 mg) resemble Adderall or MDMA and don’t produce strong visuals.
The higher the dose, the more psychedelic it gets. The 35 mg dose is a potent psychedelic — and very high doses (50 mg or more) are profoundly psychedelic and have even been known to induce out-of-body experiences.
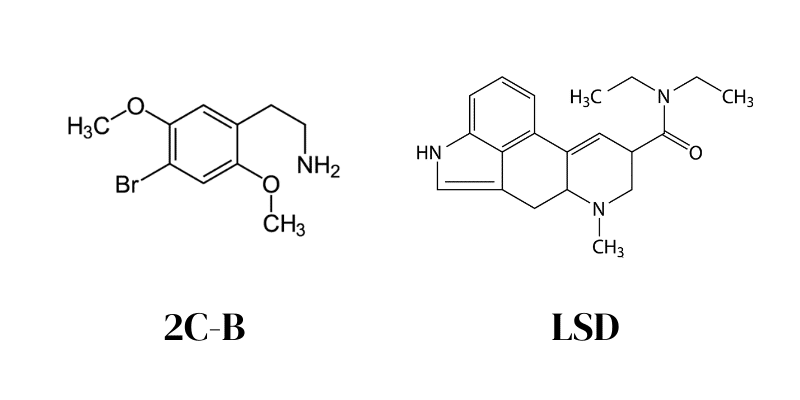
2C-B is often compared to LSD because the visual effects of these two drugs are very similar. Users experience light trails, geometric patterns, and objects that appear to merge together.
The intensity of the trip is very similar for these two drugs, but 2C-B is generally much more euphoric. Some people argue the euphoria induced by 2C-B isn’t “earned.” This means you don’t actually have to do anything to feel the euphoria; it’s merely a byproduct of the substance itself.
With LSD, the euphoria needs to be earned through experience and mindset. It doesn’t have an inherent euphoric quality to it, so those without the right mindset may not feel any euphoria whatsoever.
In terms of dose, LSD is many times more potent than 2C-B. The psychoactive dose of LSD is measured in sub-milligram doses, while the threshold dose for 2C-B is around 5 mg.
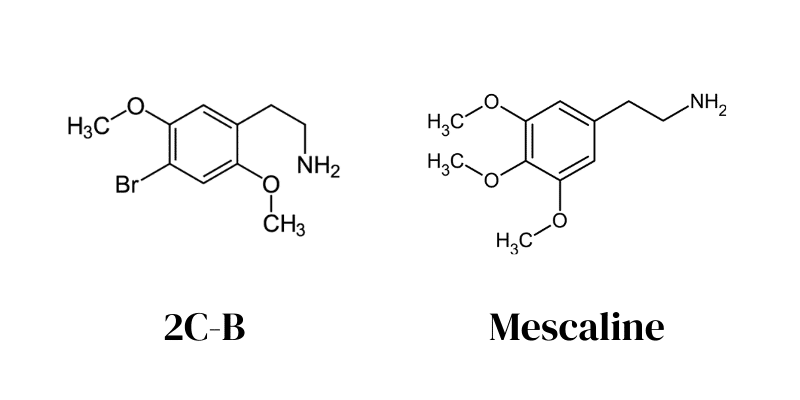
Most people suggest the effects of 2C-B are a combination of LSD and MDMA. However, it’s more accurate to suggest the effects of 2C-B resemble mescaline — which is actually the molecule used as inspiration for creating the entire 2C class of drugs, to begin with.
2C-B is more stimulating than mescaline and has much less “headspace.” Headspace refers to the introspective and existential thoughts that accompany the psychedelic experience.
Both 2C-B and mescaline are thought of as being “gentle” when compared to other psychedelics and the visuals are very similar between the two.
In lower doses, their visuals are very “flowy”, while higher doses are much more “cartoon-like.”
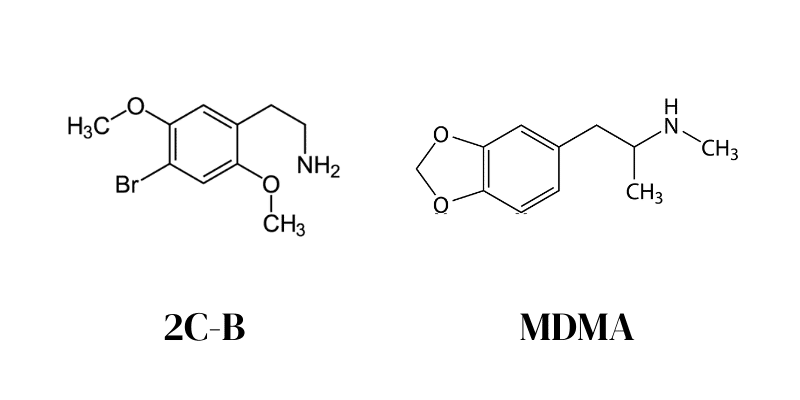
2C-B is often used as an alternative to MDMA (ecstasy) at concerts, music festivals, or parties. Lower doses of 2C-B are the most similar to MDMA for creating a greater sense of connectedness with the people around you. Both substances produce a feeling of euphoria, can enhance the enjoyment of music, and stimulate the sensual feedback from touch.
The more 2C-B you take, the further the experience diverges from MDMA. High doses are very psychedelic and can make being at public events very uncomfortable — unlike MDMA.
One of the main benefits of 2C-B over MDMA is that users usually don’t experience difficulty falling asleep after the experience.
Is 2C-B Safe?
There are no reported overdose deaths from people who took 2C-B. Additionally, the few clinical trials that are available involving 2C-B have all reported the drug had little to no side effects and that the drug had a high level of safety.
Anecdotal reports on sites like Reddit, as well as through our own surveys, suggest some people prefer to take large doses of the drug (over 50 mg) — without experiencing any severe side effects.
The lethal dose of 2C-B has never been found.
Some users, including Shulgin, have reported taking as much as 100 mg of 2C-B without serious side effects. However, these doses are rarely enjoyable and can even be quite scary.
2C-B has been around since the 1970s, and while it didn’t really become popular until the 90s, it still has over 30 years of mainstream use behind it. If 2C-B was inherently dangerous, it would be crystal clear by now.
With that said, there is a serious lack of research available on the safety of 2C-B. There are virtually no toxicology studies available. Due to the heavily restricted status of this substance, it’s unlikely we’re going to see this research anytime in the near future.
This isn’t the case with other 2C substances — such as 2C-E and 2C-I — which have proven themselves dangerous over the years.
With that said, 2C-B isn’t without its risks.
The main risk of this compound is adulteration (mixing or swapping other substances into 2C-B tablets or powder).
It’s not uncommon for someone to order 2C-B online only to receive something completely different in the mail. You can never trust what’s inside your pills or powders unless you test it first. And even with testing, you can’t be 100% sure it’s free from harmful chemicals.
→ Learn how to test a sample of 2C-B for adulterants
Certain drugs or medications may also interact negatively with 2C-B.
This substance is largely metabolized by an enzyme called monoamine oxidase (MAO) [ 2 ]. It’s the main enzyme responsible for breaking down neurotransmitters, including dopamine, serotonin, and norepinephrine. People taking MAO inhibitor medications (a type of antidepressant) may have a hard time metabolizing 2C-B — which could lead to side effects.
2C-B is also likely to interact negatively with other stimulating substances, such as amphetamines (Adderall), MDMA, MDA, cocaine, caffeine, and nicotine. Combining these substances could lead to side effects and harm involved with increased heart rate and blood pressure, changes in breathing patterns, jitteriness and muscle tension, dehydration, headaches, blood sugar regulation, and anxiety or panic.
Mixing 2CB with other psychedelics like LSD, mescaline, or magic mushrooms can lead to much stronger hallucinations. This can cause intense fear, panic, or anxiety.
It’s wise to avoid any other substances while taking 2C-B to avoid negative interactions. This includes alcohol, cigarettes, and prescription medications.
People taking heart medications, immune system regulators, antibiotics, or ADHD medications should avoid 2C-B altogether.
- Fear, panic, or anxiety
- Nausea & vomiting
- Digestive discomfort
- Rapid heart rate
- High blood pressure
2C-B is not inherently addictive — however, people can form addictions to any mind-altering substance, including 2C-B.
There really isn’t such a thing as a “good drug” or a “bad drug.” Substances like 2C-B are just molecules that exist in the world around us. It’s our relationship to them and the way we use them that can be described as “healthy” or “unhealthy.”
An unhealthy relationship with a substance like 2C-B would involve regular, repeated use of the substance either out of compulsion or to find a release from reality.
This is essentially what addiction is. They’re using a substance to escape the way they feel or to escape a reality they deem “undesirable.”
2C-B makes us happy, carefree, relaxed, social, and euphoric. It changes our perspective of the world and allows us to forget our biggest fears and stressors.
While this can be extremely beneficial for helping someone acknowledge the source of their problems internally and acts as a reminder that life, in its essence, is good — it can also become a crutch for people with more of a nihilistic or doomer perspective on life.
Compulsive use of any substance would be an example of having an unhealthy relationship with the substance. It’s what defines addiction.
Psychedelics like 2C-B should be used for personal growth and healing — not to escape reality.
2C-B & Physical Addiction: Dependence & Tolerance
There are two types of addiction — behavioral addiction and physical addiction.
As described above, behavioral addiction is the type of addiction we can have for the way a substance or activity makes us feel. Our body isn’t dependent on the substance, but we still seek it out in order to feel a certain way. We can also become behaviorally addicted to gambling, sex, masturbation, or shopping.
Physical addiction is differentiated from behavioral addiction in that there is a physical change to the body’s homeostatic default settings in response to the drug. When we take a substance repeatedly, the body makes changes to adapt to the presence of the substance. This is called dependence because we depend on having the drug in our system to maintain balance. As soon as the drug wears off, we’re no longer in balance — causing side effects referred to as withdrawal.
2C-B can eventually lead to physical addiction if used repetitively over long periods of time.
All 2C substances are illegal globally. The entire family of research chemicals was originally banned in the United States in 1995. 2C-B was specifically added to the UN Convention of Psychotropic Substances in 2001 . This led to the banning of this substance in all UN-member countries.
In the US, 2C-B is listed as a Schedule I drug — along with heroin, LSD, and cocaine.
It’s classified as a Schedule III substance in Canada, which means it’s only available for research purposes.
In the United Kingdom, 2C-B is a Class A drug — which implies the drug poses a significant danger to public health and brings the most severe punishments to those caught in possession of the drug.
Related: What is psychedelic-assisted psychotherapy?
There isn’t much research available on 2C-B, but we do have a general understanding of how it works.
Most psychedelics work by activating the 5-HT2A serotonin receptors. This is the primary mechanism of action employed by substances, including LSD, DMT, and psilocybin.
2C-B and related phenethylamines like mescaline have a much weaker action on this receptor. This suggests there are other mechanisms involved with the drug’s hallucinogenic effects. Some studies even suggest 2C-B may act as an inhibitor of the 5-HT2A receptor [ 3 ].
Some studies suggest 2C-B activates another serotonin receptor called 5-HT2C — which also produces hallucinogenic effects [ 4 ].
Other serotonin receptors may also be involved, such as the 5-HT1A receptors, which could be involved in the emotional changes induced by 2C-B [ 5 ]. This substance is reported to influence the emotional response through both top-down and bottom-up cognitive processes.
Compared to other 2C-x drugs, 2C-B is the second most potent agonist of serotonin receptors only to 2C-I. 2C-D and 2C-H have a much lower affinity for these receptors.
2C-B has also been shown to have some action at the alpha-adrenergic receptors [3]. This is likely one of the main mechanisms involved with the substance’s stimulating effects.
Research on 2C-B is seriously lacking. Despite how popular this substance is, there are no clinical trials or even toxicology studies to date. The only data we have available comes from anecdotal reports, observational studies, and in vitro research. If you want to contribute your experience to improve our understanding of 2C-B or other psychedelics, consider filling out one or more of our psychedelic surveys and sharing your experience.
Frequently Asked Questions About 2C-B
Everybody should test their drugs before using them to avoid mistakenly consuming toxic alternatives.
The best way to test a sample of 2C-B is to use a reagent test kit. Only a small sample of the drug is needed to run the test (the size of a grain of sand).
Regent tests won’t tell you the purity of a substance. They can only tell you whether or not a sample contains a certain substance or not.
The best reagent to use is the Marquis reagent. It will turn a yellowish-green color in the presence of 2C-B. The reagent will turn purple if the sample contains MDMA, and NBOMe substances will turn red.
Most drug tests won’t detect 2C-B. Only specialized drug tests using mass spectrometry or gas chromatography will be able to differentiate 2C-B in a blood or urine sample.
There have been reports of 2C-B triggering a false-positive on amphetamine tests, but this is very rare.
With that said, if you’re expecting a drug test for any reason, it would be wise to avoid 2C-B.
All psychoactive drugs have an inherent level of risk associated with their use. 2C-B has stimulating effects that could be dangerous for people with heart disease or who are taking heart medications.
The hallucinogenic effects of 2C-B could bring an increased level of risk to people with psychiatric disorders.
2C-B has never been associated with any overdoses or deaths, but there’s been one case of reported psychosis after using 2C-B [ 7 ].
Microdosing is the process of taking very small, sub-perceptual doses of a substance. They’re used to increase focus and concentration, improve empathy and connectedness with others, and help achieve a higher level of productivity.
Some users have reported taking microdoses of 2C-B similarly to other psychedelics like magic mushrooms or LSD. It’s been reported to increase tactile awareness, increase the clarity of thought, and boost mental energy and stamina.
It’s not clear whether or not microdoses of 2C-B are safe long term.
Final Thoughts: What Is 2C-B?
2C-B is one of the most popular psychoactive substances globally — despite there being virtually no research available on its safety or effect profiles in the medical literature.
It’s often used as an alternative to MDMA at lower doses and an alternative to LSD in high doses.
Compared to other psychedelics, 2C-B is considered gentle — which effects described as being a combination of MDMA and LSD. A better comparison is mescaline — which is the molecule Alexander Shulgin used to derive the 2C class of drugs, to begin with.
We’re running a continual survey on the use of 2C-B to better understand the effects and use patterns surrounding this unique psychedelic substance.
If you’ve tried 2C-B and want to contribute to this research, you can anonymously enter details of your experience through this 6-minute 2C-B survey . We greatly appreciate your participation!
- Carmo, H., Hengstler, J. G., De Boer, D., Ringel, M., Remião, F., Carvalho, F., … & de Lourdes Bastos, M. (2005). Metabolic pathways of 4-bromo-2, 5-dimethoxyphenethylamine (2C-B): analysis of phase I metabolism with hepatocytes of six species, including human. Toxicology, 206(1), 75-89.
- González, D., Torrens, M., & Farré, M. (2015). Acute effects of the novel psychoactive drug 2C-B on emotions. BioMed research international, 2015.
- Villalobos, C. A., Bull, P., Sáez, P., Cassels, B. K., & Huidobro‐Toro, J. P. (2004). 4‐Bromo‐2, 5‐dimethoxyphenethylamine (2C‐B) and structurally related phenylethylamines are potent 5‐HT2A receptor antagonists in Xenopus laevis oocytes. British journal of pharmacology, 141(7), 1167-1174.
- Rickli, A., Luethi, D., Reinisch, J., Buchy, D., Hoener, M. C., & Liechti, M. E. (2015). Receptor interaction profiles of novel N-2-methoxybenzyl (NBOMe) derivatives of 2, 5-dimethoxy-substituted phenethylamines (2C drugs). Neuropharmacology, 99, 546-553.
- Papaseit, E., Farré, M., Pérez-Mañá, C., Torrens, M., Ventura, M., Pujadas, M., … & González, D. (2018). Acute pharmacological effects of 2C-B in humans: an observational study. Frontiers in pharmacology, 9, 206.
- Huang, H. H., & Bai, Y. M. (2011). Persistent psychosis after ingestion of a single tablet of’2C-B’. Progress in neuro-psychopharmacology & biological psychiatry, 35(1), 293-294.
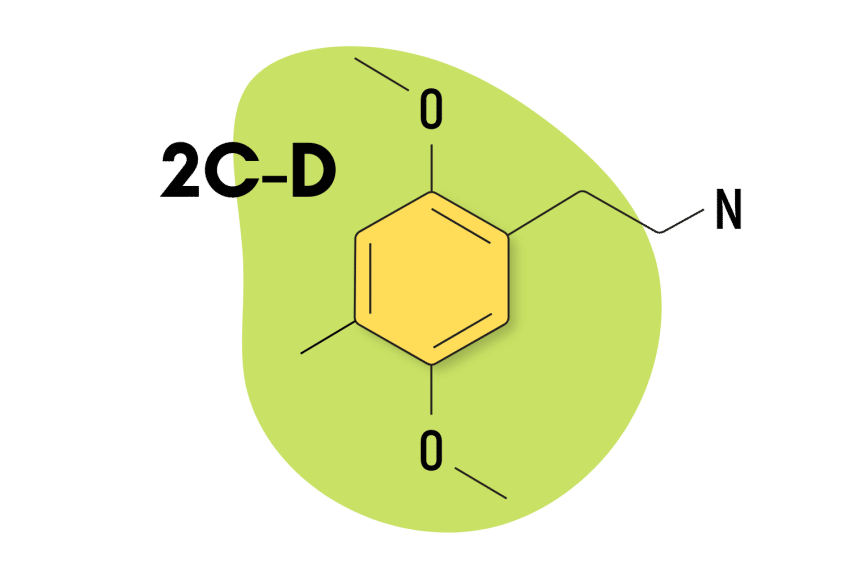
2C-D: The Intersect Between DOM & 2C-B
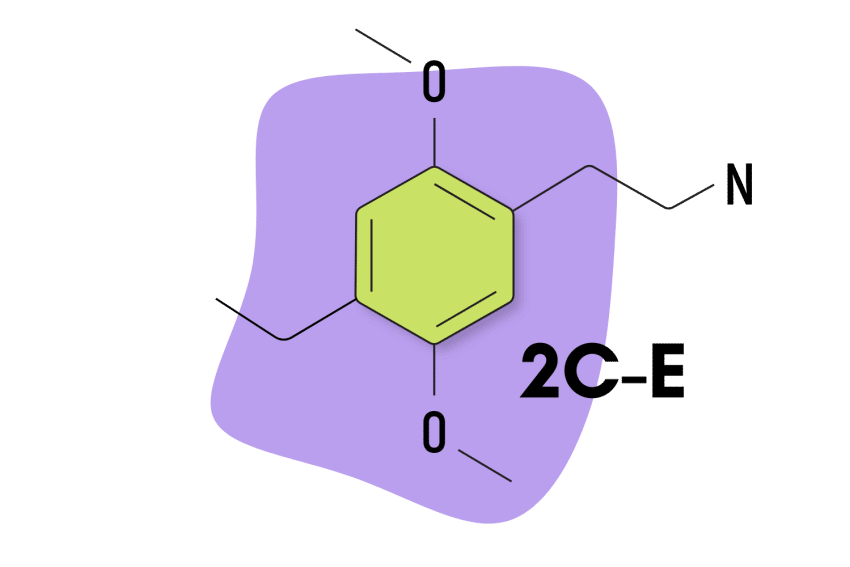
2C-E: Psychedelic Information & Safety
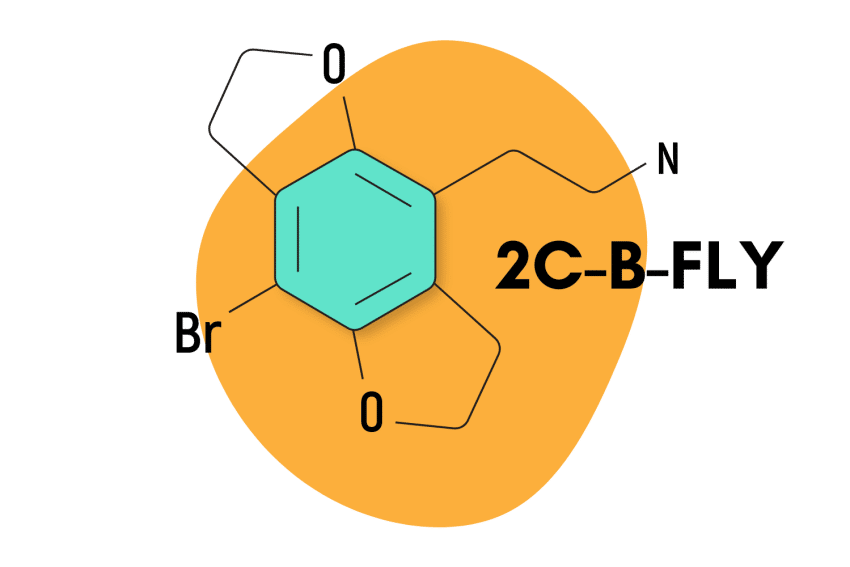
2C-B-FLY: Is It The Best Psychedelic For Arousal & Sexual Intimacy?

What Is Nexus Flipping?
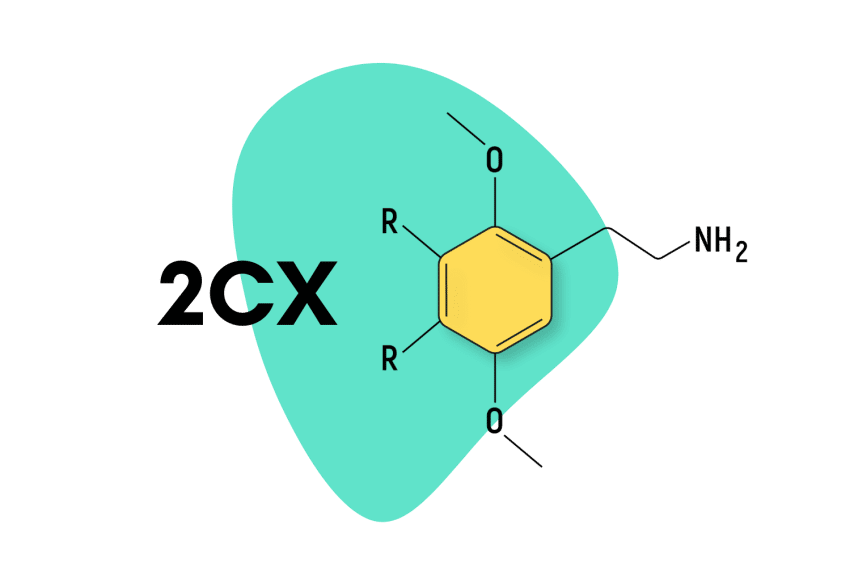
2C Psychedelics

Alexander Shulgin: The Godfather of Psychedelics

Ann Shulgin: The “Queen Of Psychedelics”
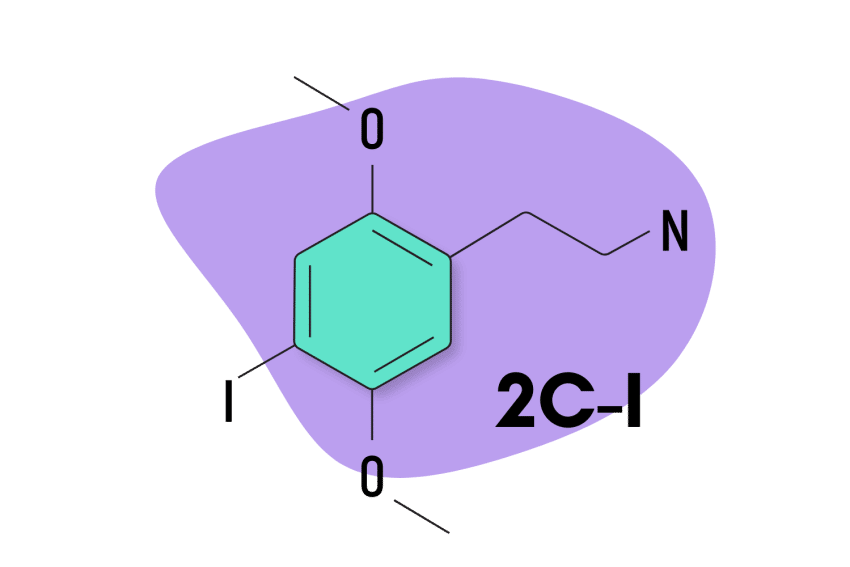
2C-I: An Obscure, But Powerful Research Chemical
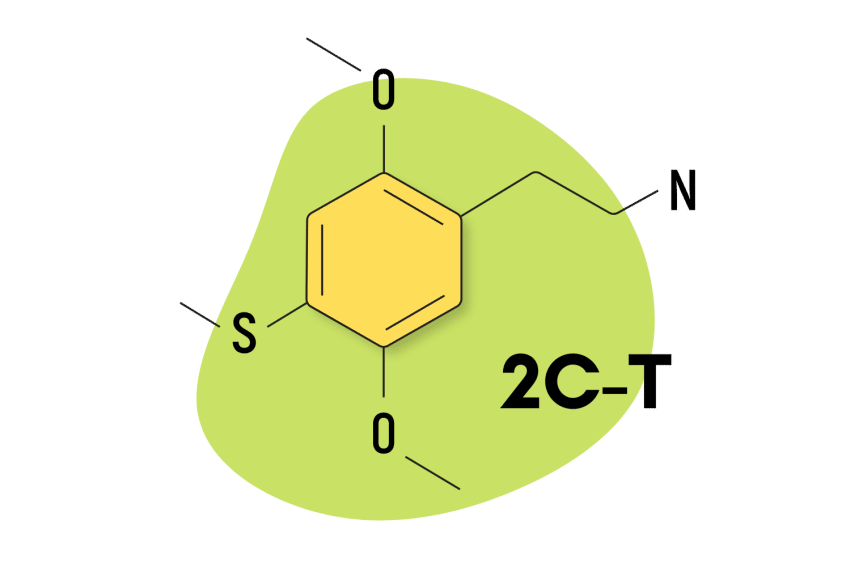
2C-T: A Tactile Psychedelic
Trip Uses, Dosage, Side Effects, Food Interaction and all others data.
Trip is chemically a novel substituted benzimidazole derivative, which suppresses the final step in gastric acid production by forming a covalent bond to two sites of H+/K+ATPase enzyme system at the secretory surface of the gastric parietal cell. This leads to inhibition of both basal and stimulated gastric effect that persists longer than 24 hours.
Trip is quantitatively absorbed and its bioavailability does not change upon multiple dosing. Trip is extensively metabolized in the liver. Almost 80% of an oral dose is excreted as metabolites in urine; the remainder is found in feces.
This drug acts to decrease gastric acid secretion, which reduces stomach acidity. Trip administration leads to long-lasting inhibition of gastric acid secretion.
General Effects
Trip has been shown to reduce acid reflux-related symptoms, heal inflammation of the esophagus, and improve patient quality of life more effectively than histamine-2 receptor antagonists (H2 blockers). This drug has an excellent safety profile and a low incidence of drug interactions. It can be used safely in various high-risk patient populations, including the elderly and those with renal failure or moderate hepatic dysfunction.
Table Of contents
- Side Effect
- Precautions
- Interactions
- Uses during Pregnancy
- Uses during Breastfeeding
- Accute Overdose
Food Interaction
Volume of distribution.
- Interaction With other Medicine
- Contradiction
Trip is used where suppression of acid secretion is of therapeutic benefit. Trip Is registered in the foltawing indications:
- Peptic ulcer diseases (PUD)
- Gastro-esophageal reflux diseases
- Treatment of ulcer resistant to M2 blocker
- Treatment of ulcer induced by NSAIDs
- Gl bleeding from stress or acid peptic diseases
- Eradication of Helicobacter pylori
- Zollinger-Ellison syndrome
- Prophylaxis for acid aspiration syndrome during induction of anesthesia
Trip is also used to associated treatment for these conditions: Erosive Esophagitis , GERD With Erosive Esophagitis , Gastro-esophageal Reflux Disease (GERD) , Healing , Heartburn , Helicobacter Pylori Infection , Stress Ulcers , Zollinger-Ellison Syndrome , Conditions where a reduction of gastric acid secretion is required , Pathological hypersecretory conditions
How Trip works
Hydrochloric acid (HCl) secretion into the gastric lumen is a process regulated mainly by the H(+)/K(+)-ATPase of the proton pump, expressed in high quantities by the parietal cells of the stomach. ATPase is an enzyme on the parietal cell membrane that facilitates hydrogen and potassium exchange through the cell, which normally results in the extrusion of potassium and formation of HCl (gastric acid).
Proton pump inhibitors such as pantoprazole are substituted benzimidazole derivatives, weak bases, which accumulate in the acidic space of the parietal cell before being converted in the canaliculi (small canal) of the gastric parietal cell, an acidic environment, to active sulfenamide derivatives. This active form then makes disulfide bonds with important cysteines on the gastric acid pump, inhibiting its function. Specifically, pantoprazole binds to the sulfhydryl group of H+, K+-ATPase, which is an enzyme implicated in accelerating the final step in the acid secretion pathway. The enzyme is inactivated, inhibiting gastric acid secretion. The inhibition of gastric acid secretion is stronger with proton pump inhibitors such as pantoprazole and lasts longer than with the H(2) antagonists.
Trip dosage
The usual recommended adult oral dose is 40 mg given once daily, preferably in the morning with or without food. The duration of therapy is ranging from 2-8 weeks.
- Duodenal ulcers: Trip 40 mg tablet once daily for 2-4 weeks.
- Gastric ulcer: Trip 40 mg tablet once daily for 4-8 weeks.
- Reflux esophagitis: Trip 40 mg tablet once daily for 4-8 weeks.
- Ulcers induced by NSAIDs: Trip 40 mg tablet once daily.
- Maintenance therapy: Maintenance therapy should involve the lowest effective dose of the drug. Trip both 20 mg & 40 mg doses are safe and effective in maintaining patients with healed reflux esophagitis and PUD in remission.
IV Injection:
- Duodenal ulcer and gastric ulcer : 40 mg once daily for 7-10 days
- Gastroesophageal reflux disease associated with a history of erosive esophagitis : 40 mg once daily for 7-10 days
- Prevention of rebleeding in peptic ulcer : IV 80 mg, followed by 8 mg/hour infusion for 72 hours
- Prophylaxis of acid aspiration : 80 mg IV every 12 h for 24 h, followed by 40mg every 12 h
- Long-term management of Zollinger-Ellison Syndrome and other pathological hypersecretory conditions : 80 mg IV every 12 hours, may increase to 80 mg every 8 hours if needed, may titrate to higher doses depending on acid output.
DIRECTION FOR USE OF IV INJECTION : Trip lyophilized powder and 0.9% Sodium Chloride Injection is for intravenous administration only and must not be given by any other route. Trip IV injection should be given as a slow intravenous injection. The solution for IV injection is obtained by adding 10 ml 0.9% Sodium Chloride Injection to the vial containing powder. After reconstitution the injection should be given slowly over a period of at least 2 to 5 minutes. Use only freshly prepared solution. The reconstituted solution may be stored at room temperature (up to 30° C) for a maximum 4 hours.
DIRECTION FOR USE OF IV INFUSION : Trip IV infusion should be given as an intravenous infusion over a period of approximately 15 minutes. Trip IV infusion should be reconstituted with 10 ml of 0.9% Sodium Chloride Injection and further diluted (admixed) with 0.9% Sodium Chloride Injection or 5% Dextrose or Lactated Ringer's Injection to a final volume of 100 ml. The reconstituted solution may be stored at room temperature (up to 30° C) for a maximum 4 hours prior to further dilution. The admixed solution may be stored at room temperature (up to 30° C) and must be used within 24 hours from the time of initial reconstitution.
Side Effects
No potentially life-threatening effects have been reported with Trip. Symptomatic adverse effects include headache and diarrhoea are two common reported adverse effects. Peripheral edema has been occasionally reported in female patients. Other side effects may include abdominal pain, dizziness, nausea, epigastric discomfort, flatulence, skin rash, pruritus etc.
Rat Oral LD 50 747 mg/kg
Tumorigenicity
Because of the chronic nature of GERD, there may be a potential for long-term administration of pantoprazole. In long-term rodent studies, pantoprazole was carcinogenic and its administration lead to rare types of gastrointestinal tumors. The relevance of these findings to tumor development in humans is unknown at this time.
Teratogenic Effects
This drug falls under pregnancy category B category. Reproduction studies have been performed in rats at oral doses up to 88 times the recommended human dose (RHD), as well as in rabbits at oral doses up to 16 times the RHD, and have shown no evidence of impaired fertility or harm to the fetus caused by pantoprazole. No adequate and well-controlled studies in pregnant women have been completed. Because animal reproduction studies are not always predictive of human response, this drug should only be used during pregnancy if clearly required.
Nursing Mothers
Trip and its metabolites have been found to be excreted in the milk of rats. Trip excretion in human milk has been found in a study performed with a single nursing mother after one 40 mg oral dose. The clinical relevance of this finding is not known, however, it is advisable to take note of this finding when considering pantoprazole use during nursing. Many drugs excreted in human breastmilk have a risk for serious adverse effects in nursing infants.
Patients should be cautioned that Trip tablet should not be split, crushed or chewed. The tablet should be swallowed whole, with or without food in the stomach. Concomitant administration of antacid does not affect the absorption of Trip.
Interaction
There is no interaction with concomitantly administered antacids. No dosage adjustment is needed with combination use of the following drugs: Theophylline, Caffeine, Diazepam, Digoxin, Ethanol, Metoprolol, Nifedipine or Warfarin.
- Take with or without food. The absorption is unaffected by food.
Trip Drug Interaction
Moderate: atorvastatin , clopidogrel , levothyroxineMinor: aspirin , aspirin , duloxetine , cyanocobalaminUnknown: rosuvastatin , apixaban , omega-3 polyunsaturated fatty acids , pregabalin , metoprolol , metoprolol , albuterol , budesonide / formoterol , acetaminophen , ascorbic acid , cholecalciferol , alprazolam , cetirizine
Trip Disease Interaction
Major: C. diffModerate: liver disease , bone fractures , hypomagnesemia
The apparent volume of distribution of pantoprazole is approximately 11.0-23.6 L, distributing mainly in the extracellular fluid.
Elimination Route
Trip is absorbed after oral administration as an enteric-coated tablet with maximum plasma concentrations attained within 2 – 3 hours and a bioavailability of 77% that does not change with multiple dosing . Following an oral dose of 40mg, the Cmax is approximately 2.5 μg/mL with a tmax of 2 to 3 hours. The AUC is approximately 5 μg.h/mL. There is no food effect on AUC (bioavailability) and Cmax.
Delayed-release tablets are prepared as enteric-coated tablets so that absorption of pantoprazole begins only after the tablet leaves the stomach.
About 1 hour
Adults : With intravenous administration of pantoprazole to extensive metabolizers, total clearance is 7.6-14.0 L/h. In a population pharmacokinetic analysis, the total clearance increased with increasing body weight in a non-linear fashion.
Children : clearance values in the children 1 to 5 years old with endoscopically proven GERD had a median value of 2.4 L/h.
After a single oral or intravenous (IV) dose of 14C-labeled pantoprazole to healthy, normal metabolizing subjects, about 71% of the dose was excreted in the urine, with 18% excreted in the feces by biliary excretion. There was no kidney excretion of unchanged pantoprazole.
Pregnancy & Breastfeeding use
There are no adequate or well-controlled studies in pregnant women. Trip should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
It is not known whether Trip is excreted in human breast milk. Trip should be used during lactation only if the potential benefit justifies the potential risk.
Contraindication
It is contraindicated in patients with known hypersensitivity to Trip.
Acute Overdose
There are no known symptoms of overdosage in humans. Since Trip is highly protein bound, it is not readily dialyzable. Apart from symptomatic and supportive management, no specific therapy is recommended.
Storage Condition
Store in a cool, dry place and away from light. Keep out of the reach of children.
Innovators Monograph
You find simplified version here Trip
Trip contains Pantoprazole see full prescribing information from innovator Trip Monograph , Trip MSDS , Trip FDA label
What is Trip used for?
Trip is used to treat damage from gastroesophageal reflux disease (GERD), a condition in which backward flow of acid from the stomach causes heartburn and possible injury of the esophagus (the tube between the throat and stomach) in adults and children 5 years of age and older.
How does Trip work?
Trip is a type of medicine called a proton pump inhibitor (PPI). Proton pumps are tiny substances in the lining of the stomach that help it make acid to digest your food. Trip prevents proton pumps from working properly. This reduces the amount of acid the stomach makes.
When will I feel better after taking Trip?
You should start to feel better within 2 to 3 days. It may take up to 4 weeks for Trip to work properly so you may still have some symptoms during this time. If you bought Trip without a prescription, and feel no better after 2 weeks, tell your doctor. They may want to do tests or change you to a different medicine.
Is it safe to take Trip for a long time?
If you take Trip for more than 3 months, the levels of magnesium in your blood may fall. This can make you feel tired, confused and dizzy and cause muscle twitches, shakiness and an irregular heartbeat. If you get any of these symptoms, tell your doctor. Taking Trip for more than a year may increase your chances of certain side effects, including:
- bone fractures
- gut infections
- vitamin B12 deficiency - symptoms include feeling very tired, a sore and red tongue, mouth ulcers, and pins and needles
If you take Trip for longer than 1 year your doctor will regularly check your health to see if you should carry on taking it.
What are the side effects of taking Trip?
Taking Trip long-term may cause you to develop stomach growths called fundic gland polyps. Talk with your doctor about this risk. Common side effects of Trip include
- injection site reactions (redness, pain, swelling),
- abdominal or stomach pain,
- joint pain,
- weight changes,
- drowsiness,
- tired feeling, or
- sleep problems (insomnia).
Does Trip work immediately?
Trip takes approximately two and a half hours to begin working, so it won't be effective for current symptoms. However, patients who need immediate relief from their acid reflux symptoms can combine pantoprazole with fast-acting Tums or Maalox to reduce the amount of acid.
Is drinking water good for acid reflux?
Frequently consuming water can make the digestion process better and curb GERD symptoms.
How safe is Trip?
PPI have minimal side effects and few slight drug interactions and are considered safe for long term treatment. Trip is significantly effective both for acute and long-term treatment with excellent control of relapse and symptoms. It is well tolerated even for long-term therapy and its tolerability is optimal.
Does Trip work better than omeprazole?
Generally, pantoprazole and omeprazole are equally effective. Studies comparing pantoprazole and omeprazole have found pantoprazole as effective as omeprazole in treating GERD as well as treating stomach ulcers.
How long does it take for Trip to leave the body?
Trip is extensively metabolized in the liver through the cytochrome P-450 system, predominantly by CYP2C19 demethylation with subsequent sulfation and has a serum elimination half-life of about 1.1 hours.
What are the side effects of stopping Trip?
Most patients have difficulty discontinuing their PPI's because the amount of acid in their digestive system surges when they stop taking the drug, and they're often left with symptoms like excruciating stomach pain and increased heartburn.
How long after taking Trip can I eat?
Trip oral granules should be taken 30 minutes before a meal.
How long does it take for stomach acid to return to normal?
For most people acid levels return to normal within one to two weeks.
Is Trip safe in pregnancy?
Usually, Trip is safe to take during pregnancy.
Is Trip safe during breastfeeding?
Usually, Trip is safe to take during breastfeeding.
Are there other medicines like Trip?
There are 4 other medicines that are similar to Pantoprazole. They are:
- lansoprazole
- esomeprazole
- rabeprazole
Can I take Trip with an antacid?
You can take Trip with an antacid (for example, Gaviscon) if you need to, but leave a gap of 2 hours between them.
Will Trip affect my fertility?
There's no clear evidence to suggest that taking Trip will reduce fertility in either men or women. But speak to a pharmacist or your doctor if you're trying to get pregnant. They may want to review your treatment.
Will Trip affect my contraception?
Trip does not affect any type of regular contraception, including the combined pill. But if Trip makes you sick (vomit), your contraceptive pills may not protect you from pregnancy. If this happens, follow the instructions in the leaflet that comes with your contraceptive pills.

Dr. Tanvir Rahman
Psychiatrist

Dr. Zahidul Islam
Child Specialist

Dr. Md. Mostofa Alam Bony
Medicine Specialist

Dr. Khondoker Monirul Alam
Gastroenterologist

Dr. Sultana Ashrafi Ahmed
Kidney Specialist

Dr. Md. Najmul Karim
Hematologist

Dr. Redwana Hossain

Dr. Md Waliur Rahman
Related Content
StarsInsider
How dangerous are interactions between herbal medicines and prescribed drugs?
Posted: November 14, 2023 | Last updated: November 14, 2023

While many herbal medicines have been subject to research to ascertain their benefits, dangers, and medicinal effects (or lack thereof), the way these interact with prescription drugs is not as well researched. There is, however, some clinical evidence (some stronger than others) that allows us to get a glimpse into how some herbal medicines may interact with prescribed drugs.
In this gallery, you'll find a list of popular herbal medicines and their potential interactions with prescribed drugs. Click on for a real lesson!
You may also like: These stunning images weren't made with Photoshop

There is still a lack of solid research around interactions between herbal medicines and prescribed drugs. While a few clinical studies and trials have been conducted, it should be noted that some recommended actions are also based on case reports (concerning individual patients) and even theoretical concerns.
Follow us and access great exclusive content every day

Andrographis
Andrographis ( Andrographis paniculata ) is contraindicated for patients taking immunosuppressant medication, as it may reduce their effectiveness. A clinical study has also found that it may potentiate the effects of midazolam.
You may also like: Big stars in bad horror movies

Ashwagandha
There is a theoretical concern that taking this herbal medicine may potentiate the effects of thyroxine.

Cayenne (chili pepper)
A clinical study has found that cayenne (capsium spp) may increase absorption and levels of theophylline.
You may also like: Meet the most beautiful royal women

Celery seed
Two case reports have shown that celery seeds may reduce serum levels of thyroxine.

Chamomile ( matricaria recutit ) may potentiate the effects of warfarin and cause bleeding.
You may also like: 30 beautiful and single Hollywood celebrities

Cranberry ( vaccinium macrocarpon ) may decrease levels of immunosuppressants in the blood.

Echinacea may decrease the effectiveness of immunosuppressive medication. The herb may also interact with antiretroviral drugs.
You may also like: Why you have nightmares (and what you can do about it)

Evening primrose oil
Evening primrose oil ( oenothera biennis ) may potentiate the effects of antiplatelet and anticoagulant drugs. But according to clinical evidence, there is a low level of risk. In addition, a case report has shown a reduction in serum levels of lithium.

Garlic ( allium sativum ) can interact with paracetamol and decrease blood concentrations of warfarin. It can also cause hypoglycemia when taken with chlorpropamide. Garlic may also decrease the blood levels of HIV protease inhibitors.
You may also like: Wedding dress trends for 2018

Ginger ( zingiber officinale ) may increase the effectiveness of phenprocoumon and therefore increase the risk of bleeding when taken with warfarin. It may also interact with nifedipine, producing a synergistic antiplatelet effect.

Ginkgo ( ginkgo biloba ) interactions include antiplatelet and anticoagulant drugs such as warfarin (it can cause bleeding). It can raise blood pressure when combined with thiazide diuretic, and can lead to coma when taken with trazodone.
You may also like: The coldest places in America

Other interactions include antipsychotic medication, antiretroviral drugs, benzodiazepines, hypoglycemic drugs, nifedipine, tadalafil, and talinolol. Many of these, however, have a low level of risk.

The use of green tea ( camellia sinensis ) is contraindicated for patients taking isoniazid, as it may affect the liver. It may also reduce the bioavailability of sunitinib, and decrease the effectiveness of ziprasidone.
You may also like: The theories behind the ever-mysterious death of Edgar Allan Poe

Clinical studies have found that hawthorn may increase the effectiveness of digoxin.

Two case reports have shown that horsetail ( equisetum arvense ) may cause a virological breakthrough when taken with antiretroviral drugs.
You may also like: Celebrity siblings that fame forgot

Kava ( piper methysticum ) can interact with Parkinson medications, particularly levodopa (or L-Dopa). It can also interact with alprazolam and lead to a semicomatose state.

Korean ginseng
Ginseng ( panax ginseng ) can lower blood concentrations of warfarin, and induce mania if used with phenelzine. It may decrease the effectiveness of antihypertensive medications, including nifedipine.
You may also like: Tips for impeccable hair without leaving the comfort of home

Ginseng may also cause side effects such as headaches, sleeplessness, and tremors when taken with MAO inhibitors. Ginseng may also interact with hypoglycemic drugs, including insulin, and potentiate hypoglycemic activity of these drugs.

Licorice ( glycyrrhiza glabra ) may decrease the effectiveness of antihypertensive medications (excluding diuretics).
You may also like: Unprofessional stars involved in spats at work

Licorice may also cause hypokalemia when taken with cilostazol, according to a case report. In high doses, licorice can actually cause pseudoaldosteronism and high blood pressure.

Milk thistle
A clinical study has found that milk thistle increases the levels of domperidone and its potential toxic side effects. Hepatically-impaired patients may want to avoid taking it with immunosuppressives such as sirolimus, as it may reduce drug clearance. Milk thistle may also increase blood levels of ornidazole and talinolol.
You may also like: Having a bad day? These photos will help!

Rhodiola ( rhodiola rosea ) may interact with SSRIs, affecting serotonin levels.

A case report showed that sage may potentiate the adverse effects of methadone.
You may also like: The most horrific science experiments of all time

Schisandra ( schisandra chinensis ) may increase drug concentrations of immunosuppressives.

St. John's wort
Research has shown that St. John’s wort can reduce blood levels of benzodiazepines, calcium channel antagonists, cancer chemotherapeutic drugs, clozapine, immunosuppressives, cyclosporin, amitriptyline, digoxin, indinavir, warfarin, phenprocoumon, and theophylline. This flowering plant also interacts with oral contraceptives.
You may also like: Australia’s secret swimming spots

Turmeric ( curcuma longa ) may potentiate the effects of antiplatelet and anticoagulant drugs. Turmeric may also increase drug levels of tacrolimus and talinolol. There is a case report of acute liver injury related to long-term use of the herb in combination with etoricoxib.

There is theoretical concern, but not much clinical evidence to support it, that valerian ( valeriana officinalis ) potentiates the effects of CNS depressants or alcohol.
You may also like: Banned baby names in Australia

Willow bark
A clinical study has found that willow bark may potentiate the effects of warfarin.
Sources: (Standard Process) (PubMed) (International Society of Pharmacovigilance)
More for You
Democrat Judge Exempts NRA Members From New Gun Rule
Repel Fleas From Your Home With An Ingredient From Your Kitchen
Arby’s Is Giving Away Free Sandwiches All Month Long
The 43 Best Shows to Stream on Netflix Right Now
13 Things You Should Never Keep in Your Wallet
The Best Bar in the World Only has 15 Seats, 1 Bartender, and a Narnia Vibe
The Best Way To Keep Bananas From Turning Brown Too Fast
Karine Jean-Pierre Slams Peter Doocy For 'Disingenuous' Question
Nate Berkus' Unique Kitchen Cabinet Choice Is The New 2024 Trendsetter
Solo Leveling Episode 12 Is A Cliched Finale
The first interracial kiss aired on TV more than 50 years ago—and more shows that broke racial barriers
The 25 Best Long-Lasting Perfumes You Won't Need to Reapply
10 Hiding Spots Burglars Always Look First
Virtual colonoscopy lets you skip the scope. Here’s what to know about the colorectal cancer screening Mark Cuban says saves time and money
McDonald’s brings beloved breakfast sandwich back to select locations
Here’s How Much I Made at My First Job at Amazon — and What I Make Now
NCAA women's basketball Final Four power rankings: Who is the best team left in the tournament?
19 Easy Ways to Fall Back Asleep After Waking Up in the Middle of the Night
Renewed and Canceled TV Shows 2024 Guide
11 weird laws you never knew existed – see how many you’ve broken
- Safety Guidelines for Hallucinogens - Research Excerpts
“Human hallucinogen research: guidelines for safety”
Annotated by TripSafe for faster reading
Johnson, M., Richards, W., & Griffiths, R. (2008). Human hallucinogen research: Guidelines for safety. Journal of Psychopharmacology, 22(6), 603–620. doi:10. 1177 ⁄ 0269881108093587
The full paper is online here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3056407/
These excerpts are designed to include pretty much everything that could be relevant to a non-clinical guide or participant, with headers/signposts to make reading easier. I find that reading scientific papers can be much slower than reading text with smaller sections and more headings.
Persisting adverse reactions are rare when research is conducted along these guidelines. Incautious research may jeopardize participant safety and future research. However, carefully conducted research may inform the treatment of psychiatric disorders, and may lead to advances in basic science.
Ayahuasca religious freedom act USA
Because the United States Supreme Court has recently ruled in favour of the União do Vegetal (UDV; a syncretic Brazilian church that uses ayahuasca in the context of religious ceremonies) in their claim that the UDV’s use of ayahuasca is protected under the Religious Freedom Restoration Act (Gonzales v. O Centro Espirita Beneficiente União do Vegetal, 2006), ayahuasca use within this church setting may receive increased scientific investigation within the USA.
Why say hallucinogen vs psychedelic
We use the word ‘hallucinogen’ herein to refer to the classical hallucinogens, sometimes called ‘psychedelics’, ‘psychotomimetics’ or ‘entheogens’ (Grinspoon and Bakalar, 1979; Ruck, et al., 1979; Ott, 1996; Metzner, 2004). Admittedly, the term ‘hallucinogen’ is not ideal for these substances, because perceptual changes are only one domain of their effects, and the typical perceptual changes engendered by hallucinogens at typical doses rarely include frank hallucinations (Grinspoon and Bakalar, 1979; Nichols, 2004; O’Brien, 2006). However, we use this term because it is the most widely used in the scientific literature. Although the term ‘psychedelic’ is widely used, it has the disadvantage of carrying considerable cultural connotation (i.e. its use as a descriptor of a style of music or art associated with Western counter-culture of the 1960s). The terms ‘psychotomimetic’ (emphasizing model psychosis) and ‘entheogen’ (emphasizing mystical-type experiences, i.e. phenomenologically indistinguishable from classically described mystical experiences) highlight only a single aspect (which may not occur reliably) of the much broader range of hallucinogen effects.
Purpose of the paper
The purpose of this paper is to provide guidance in the safe administration of high doses of hallucinogens (e.g. ≥25mg psilocybin or 200 μg LSD).
Lower doses
Some aspects of these recommendations may also apply to studies employing lower doses, although, as with other drug classes, the likelihood of potential adverse effects will be related to dose.
History of hallucinogen use by indigenous cultures
Hallucinogens have been used by indigenous cultures for millennia (Schultes, 1969; Lowy, 1971; Schultes, et al., 2001). Remarkably, apparently without exception, such cultures view hallucinogenic plants and fungi as being of divine origin (Schultes, et al., 2001). Given this orientation, it is not surprising that their ingestion is often tightly restricted, with use controlled by ceremonial guidelines, including taboos against improper use (Schultes, et al., 2001; Weil, 2004). Indeed, some of the safeguards developed for clinical hallucinogen research and expressed in the guidelines presented herein are similar to important aspects of hallucinogen use by indigenous cultures. These common themes are structured use (expressed as ritual in indigenous use), restrictions on use including the need for guidance and appreciation of hallucinogens’ powerful psychological effects (expressed as reverence in indigenous use).
Be careful of backlash
The growing controversy and sensationalism resulted in increasing restrictions on access to hallucinogens throughout the 1960s (ultimately resulting in the placement of the most popular hallucinogens into Schedule I of the 1970 Controlled Substances Act in the United States), creating substantially greater regulatory barriers for researchers to conduct human trials. The negative publicity also resulted in withdrawal of federal research funds, which had previously supported much of the human research, and in the professional marginalization of clinical investigators interested in pursuing research with hallucinogens.
Physiological safety
Hallucinogens generally possess relatively low physiological toxicity, and have not been shown to result in organ damage or neuropsychological deficits (Strassman, 1984; Gable, 1993, 2004; Halpern and Pope, 1999; Hasler, et al., 2004; Nichols, 2004; Halpern, et al., 2005). Nonhuman animal studies have shown MDMA (structurally similar to some classical hallucinogens, but with a substantially different pharmacological mechanism of action) to have neurotoxic effects at high doses, although MDMA has been judged to be safe for human administration in the context of several therapeutic and basic human research studies. In contrast, there is no evidence of such potential neurotoxic effects with the prototypical classical hallucinogens (i.e. LSD, mescaline and psilocybin).
In a survey of investigators who had administered LSD or mescaline, Cohen (1960) reported that only a single case of a psychotic reaction lasting more than 48 h occurred in 1200 experimental (non-patient) research participants (a rate of 0.8 per 1000). Notably, the individual was an identical twin of a schizophrenic patient and thus would have been excluded under the proposed guidelines. The volunteer selection guidelines, addressed in a later section, will be the key factor in minimizing the risk of prolonged psychosis in human hallucinogen research studies.
Guidelines for safety
Although particular aspects of the proposed guidelines may be debatable, it is hoped that this paper will encourage such discussion while conveying the general themes and major domains of concern in human hallucinogen research. The proposed guidelines may serve as a helpful starting point for investigators planning to conduct human hallucinogen research.
Selection of volunteers
Generally healthy
In our studies at Johns Hopkins, participants must be in good general health as assessed by detailed medical history, physical examination, 12-lead ECG, blood chemistry profile, haematology and urinalysis. Pregnant women or those not practicing effective means of birth control are excluded.
Blood pressure
Relevant to general medical screening, classical hallucinogens moderately increase pulse and both systolic and diastolic blood pressure (Isbell, 1959; Wolbach, et al., 1962b; Strassman and Qualls, 1994; Gouzoulis-Mayfrank, et al., 1999; Passie, et al., 2000; Griffiths, et al., 2006). Therefore in our studies of psilocybin to date, volunteers have been excluded if resting blood pressure exceeded 140 systolic and 90 diastolic (mmHg), averaged across four assessments on at least two separate days.
Medication exclusions
Specifically, chronic administration of tricyclic antidepressants and lithium (Bonson and Murphy, 1996), and acute administration of serotonin reuptake inhibitors (Fiorella, et al., 1996) and the antipsychotic medication haloperidol (Vollenweider, et al., 1998) have been shown to potentiate hallucinogen effects, and therefore participants’ use of these represents a safety concern. Chronic administration of serotonin reuptake inhibitors (Stolz, et al., 1983; Strassman, 1992; Bonson, et al., 1996) and monoamine oxidase inhibitors (Bonson and Murphy, 1996) have been shown to decrease sensitivity to hallucinogens, and therefore participants’ use of these represents a scientific concern. It should also be noted that administration of ayahuasca (which contains monoamine oxidase inhibitors in addition to DMT) to individuals taking serotonin reuptake inhibitors may lead to a severe serotonin syndrome reaction (Callaway and Grob, 1998).
Supplement exclusions
We also advise investigators to include questions concerning over-the-counter dietary supplements in addition to prescription medications when probing medication history, and to exclude those taking potentially problematic substances (e.g. 5-hydroxytryptophan and St John’s Wort may affect serotonergic function, and, therefore, it is appropriate to exclude individuals currently or recently taking these products).
Psychiatric screening
Thorough psychiatric interviews (e.g. SCID; First, et al., 2001) should be conducted to identify contraindicated psychological functioning or history. In our research, individuals are excluded who have a current or past history of meeting DSM-IV criteria for schizophrenia or other psychotic disorders (unless substance-induced or due to a medical condition), or bipolar I or II disorder, which are the most important conditions to exclude for ensuring safety. We also exclude those with a first or second-degree relative with these disorders.
Rigidity and emotional lability (Emotional lability is a disorder characterized by involuntary emotional displays of mood that are overly frequent and excessive, often the result of various neuropathologies) personality traits
Other investigators have also excluded individuals scoring high on the personality traits of rigidity and emotional lability on the grounds that these have been significantly associated with negative experiences during hallucinogen action and during non-pharmacologically induced altered states of consciousness (Dittrich, 1993; Hasler, et al., 2004).
More psychiatric disorders
This strategy is warranted because the effects of hallucinogens may potentially interact with various psychiatric disorders. Furthermore, including volunteers with psychiatric disorders may increase the chances that symptoms from such disorders may inadvertently be misattributed to hallucinogen action. For example, our recent studies with healthy volunteers have excluded volunteers with a current or a recent past history (e.g. within the last 5 years) of alcohol or drug dependence (excluding caffeine and nicotine) or major depression, and volunteers with current obsessive-compulsive disorder, dysthymic disorder, panic disorder, dissociative disorder, anorexia nervosa or bulimia nervosa.
Study personnel / trip sitters
Importance of good sitters / monitors
It is difficult to overemphasize the importance of the interpersonal atmosphere created by study staff in influencing a volunteer’s response to a hallucinogen. Most critically, this applies to the interpersonal environment created by the actual session monitors (Leary, et al., 1964; Masters and Houston, 1966).
Qualities of good sitters / monitors
The monitors should be knowledgeable about the medical and psychological markers of potential adverse reactions to the drug. Furthermore, monitors should have significant human relation skills and be familiar with descriptions of altered states of consciousness induced by hallucinogens. Personal experience with techniques such as meditation, yoga or breathing exercises may also prove to be helpful in facilitating empathy for volunteers who experience altered states of consciousness during hallucinogen action. The lead monitor for each participant in the Johns Hopkins studies to date has been a clinical psychologist or a clinical social worker. However, we believe that clinical sensitivity (e.g. empathy, respect) is likely more important than formal degrees when considering monitor qualifications.
Two monitors is best
We recommend the presence of at least two monitors during hallucinogen administration sessions so that the volunteer will never be alone should one monitor need to briefly leave the session room (e.g. to the restroom). For each participant in the Johns Hopkins studies, we have specified a primary monitor (who takes the lead in participant interactions) and an assistant monitor, with differing required levels of involvement for the two monitors during volunteer preparation (see Preparation of volunteers section below).
Monitor gender
In prior research into potential treatment applications of hallucinogens, the presence of both genders in the monitoring team has been recommended (Grof and Halifax, 1977; Grof, 1980; Kurland, 1985). Having both genders present may foster feelings of security. In the Johns Hopkins studies, we have followed this recommendation when possible, but also have conducted sessions in which the primary and assistant monitors were of the same gender as the volunteer. We would counsel against both members of the monitoring team being the opposite gender of a volunteer, unless there is a staff member of volunteer’s gender who has established some rapport with the volunteer in advance, and who can quickly be summoned to assist should support be needed in the restroom.
Importance of all people around
all individuals at the study site having contact with the volunteer on or before the session day may influence a volunteer’s reaction to a hallucinogen. Pre-session negative mood consisting of anxiety or depression has been shown to significantly predict anxious or other negative experiences during the session (Metzner, et al., 1965).
Good qualities of people
friendly, welcoming and compassionate The staff member should maintain a positive social rapport with the volunteer to reduce the likelihood of adverse psychological reactions during the session and to gain accurate information on the volunteer’s condition so that other study staff may be notified if there is any potential reason to postpone or cancel the session
Physical environment
Pleasing environment
First, an aesthetically pleasing environment may decrease the probability of acute psychological distress. The Johns Hopkins hallucinogen research projects use a living room-like setting (Figure 1). The furniture is comfortable and is atypical for a research laboratory or medical office setting. An overly ‘clinical’ environment with an ‘antiseptic’ look (e.g. white walls, extraneous medical equipment, personnel in white lab coats) may increase anxious reactions.
The living room-like session room used in the Johns Hopkins hallucinogen research studies. Aesthetically pleasing environments such as this, free of extraneous medical or research equipment, in combination with careful volunteer screening, volunteer preparation and interpersonal support from two or more trained monitors, may help to minimize the probability of acute psychological distress during hallucinogen studies. For studies that investigate potential therapeutic effects or the phenomenology of introspective hallucinogen experiences, the use of eyeshades and headphones (through which supportive music is played) may contribute to safety by reducing the distractions of environmental stimuli and social pressures to verbally interact with research personnel.
Safety of environment
The environment should be designed keeping in mind the perceptual changes and disorientation that can occur under the influence of hallucinogens. Thus, any potentially dangerous objects (e.g. furniture with sharp corners; glass lamps) should be avoided. If there is a window in the room, the investigators need to be confident that the volunteer could not exit the window if in a delusional state.
Additionally, the session room should not have a telephone, and the participant should surrender her or his cellular telephone before the session.
Preparation of volunteers
Volunteer consent
volunteer preparation at the earliest stages must include a thorough review of the consent form, which should include in plain language the range of experiences that may result from hallucinogen administration, including changes in perception, sense of time and space, and emotion (possibly including anxiety, fear, panic and paranoia). Relative to other drug classes, the subjective effects of hallucinogens are likely more difficult to describe to a naïve volunteer; therefore, additional time may be necessary to fully discuss these potential effects with volunteers. The consent form should also include the approximate timecourse of the drug, the state of knowledge concerning its toxicity profile, and its status as an experimental drug. In addition, the consent form should state that there is a relatively small risk of adverse effects that last for hours to days after the hallucinogen session. These include mood disorders (such as depression), psychotic disorders and anxiety disorders. It should also state that there are rare reports in which hallucinogen exposure appears to cause, accelerate or precipitate the onset of significant or lasting psychiatric illnesses such as psychoses and intermittent or persisting visual perceptual abnormalities (‘flashbacks’, HPPD).
Building rapport and trust
The next step in volunteer preparation is to conduct a series of meetings between the monitors and volunteer to build rapport and trust. The relationship between the monitors and the volunteers should be well established by the time of the first session (Masters and Houston, 1966). In the Johns Hopkins studies, there are at least eight contact hours over the course of at least four meetings, usually over a 1-month period. One of these preparatory meetings should be conducted in the room in which the hallucinogen is to be administered, to familiarize the participant with the physical environment. The primary monitor meets with the volunteer during all of these meetings, while the assistant monitor is required to be present on at least one occasion. It is important that the assistant monitor, in addition to the primary monitor, has developed a trusting relationship with the volunteer because this assistant monitor will be the only person in the session room with the volunteer if the primary monitor needs to leave briefly.
Content of preparatory meetings
During these preparatory meetings, the monitors discuss meaningful aspects of the volunteer’s life. The main purpose of the participant–monitor meetings is to develop rapport and trust, which we believe helps minimize the risk of fear or anxiety reactions during the hallucinogen session. This typically includes discussions of the volunteer’s childhood, romantic life, current relationships with family and friends, and the volunteer’s philosophical and/or spiritual beliefs. Reviewing personal history and feelings may be important for two reasons. First, this discussion helps establish a significant level of trust. The interaction should convey that all aspects of the person are welcome, from the petty to the noble, from embarrassments to achievements and from sorrow to joy. By the time of the hallucinogen session day, the volunteer will ideally feel completely comfortable with the monitors, reducing the likelihood of paranoia (e.g. feeling that the monitors are trying to control her or his mind, or have deceived the volunteer about the nature of the study). Second, related personal material may ‘emerge’ under the effects of the hallucinogen. That is, the volunteer may experience intense thoughts, feelings and visions related to his or her personal history or world-view. Knowing about the volunteer’s life will allow the monitors to better understand her or his session experience and help the monitors in providing interpersonal support should strong emotions arise. If it is felt that sufficient rapport and trust have not developed during these monitor meetings, then either additional contact hours should be provided, or the volunteer’s participation should be cancelled. A high dose of a hallucinogen should not be administered to a volunteer if sufficient trust has not been established.
Preparing volunteers on bodily effects
The preparation of the volunteer should involve a detailed discussion of the possible range of experiences that may be encountered after hallucinogen administration. This includes the typical onset and duration of the drug(s) under investigation. Preparation involves discussion of the various potential physical sensations, such as nausea or heightened awareness of physiological processes, such as breathing and heartbeat. Volunteers are encouraged to trust that their bodies will continue to function properly regardless of such sensations, and that these bodily processes will continue without the volunteers’ volitional control.
Preparing volunteers on psychological effects
The major categories of potential psychological experiences during hallucinogen action should be discussed with the participant. The range of subjective experience under hallucinogens can be remarkably broad (Blewett and Chwelos, 1959; Richards, 1980; Masters and Houston, 1966; Strassman, 2001; Nichols, 2004; Stolaroff, 2004). This range of experiences includes perceptual changes, such as visual illusions, intensification of colours, proprioceptive changes (e.g. one’s body may feel gigantic or tiny), and synesthesia (e.g. seeing sounds or hearing colours). Another type of possible experience is the alteration of emotions, such that emotions of either a positive or negative nature may be greatly intensified, yielding experiences that may range from euphoria to despair. Another category of possible effects involves changes in the sense of time and space. At the extremes, time and/or space may be experienced as infinite or nonexistent. Other experiences may include thoughts, feelings or insights concerning one’s personal history (e.g. revisiting childhood memories) or current life circumstances (e.g. relations with loved ones), highly symbolic experiences (e.g. involving religious symbols, animals, etc.), and experiences described by some to be of a mystical or spiritual nature. Importantly, it should be emphasized that these experiences may consist of much more than the participant subjectively observing internal and external events. Rather, the effects may involve a profound change in one’s sense of self, such that one feels as if he or she is merging into the surrounding environment or the entire universe (Schultes, et al., 2001). The individual may temporarily experience a complete loss of subjective self-identity, a phenomenon sometimes referred to as ‘ego loss’ or ‘ego death’ (e.g. Leary, et al., 1964; Grof and Halifax, 1977; Grof, 1980). a detailed discussion concerning the range of possible hallucinogen effects will enhance safety by psychologically preparing the participant for the unique and often intense effects of a hallucinogen
Informing volunteers how to handle difficult experiences
The volunteers should be given guidance on how to handle difficult hallucinogen experiences. Whether the disturbance consists of frightening illusions or internal imagery, difficult thoughts and feelings about some past or present personal issue, or anxiety related to a radical change in sense of self (e.g. temporary loss of self-identity), the volunteer is encouraged to mentally surrender to the experience, trusting that her or his usual state of consciousness will return when the drug effects resolve (Blewett and Chwelos, 1959; Masters and Houston, 1966; McCabe, 1977). For example, if the participant experiences disturbing internal imagery of a demon or monster, he or she is encouraged to mentally approach the figure and interact with it (e.g. imagine asking the figure why it has appeared), rather than attempt to flee from the disturbing imagery. The participant should be alerted that sometimes people experience extremely convincing sensations of dissolving, melting, exploding and so forth, and that the best way to deal with all such situations is to surrender to the experience, subjectively allowing oneself to dissolve, melt or explode. Similar advice applies to physical symptoms such as nausea; for example, participants may be encouraged to ‘dive in’ to their stomachs, which may alleviate the nausea, as it has been suggested anecdotally that nausea and other somatic discomforts may in part be of a psychosomatic nature (Blewett and Chwelos, 1959; Masters and Houston, 1966).
Not encouraging them to read about typical experiences
In the Johns Hopkins studies, we have not encouraged participants to read the diverse and widely varying published accounts of hallucinogen effects as part of their preparation, because this may introduce compelling idiosyncratic expectations.
During the session / trip
Furthermore, medication for the treatment of acute hypertension (e.g. intravenous labetalol) should be immediately available in the event that blood pressure exceeds predetermined safety parameters.
Restroom visits
If the volunteer needs to walk to complete study tasks or to go to the rest room, the monitors should stand close by to assist by gently holding an arm or shoulder. Even with high doses of hallucinogens, individuals do not typically show substantial motor impairment, and will likely be able to ambulate without considerable difficulty (with the exception of hallucinogens such as parenteral DMT with abrupt effects and short duration of action). However, perceptual and proprioceptive effects may make walking disorienting, which is why gentle guidance may be helpful. Either the restroom door needs to have no lock, or study staff should have a key readily available if needed.
Don’t leave them alone
One of the monitors should always be present in the session room with the participant.
Don’t have other people interact with them
Because the session monitors will have developed rapport and trust with the participant, they should be the only people to interact with the volunteer during the course of hallucinogen action, barring any non-routine event (e.g. fire alarm, medical intervention by a specialist). Individuals who are anticipated to have contact with the volunteer during the course of hallucinogen action (e.g. nurse, physician) should have at least met with the volunteer once prior to session to develop some degree of rapport and trust.
If they try and leave
Any attempt by a disoriented volunteer to leave the session area would be met with compassionate but firm direction to return to the session room. Interestingly, the volunteer who fled Strassman’s (2001) study site on psilocybin was a carefully screened, experienced LSD user. Therefore, it is imperative for safety reasons that the study site environment, session procedures and participant preparation all minimize the chance of a volunteer leaving the study site.
Unexpected scenario
On the single occasion at Johns Hopkins in which a fire alarm sounded during a session, the two study monitors closely escorted the volunteer outside, making sure to minimize contact with other individuals. The three of them walked to a nearby quiet area with an attractive landscape and enjoyed the scenery until the volunteer and monitors could return to the building. The monitors encouraged the participant to view the occasion as an opportunity to enjoy the natural world outdoors (something normally unavailable during sessions), rather than as an impediment to having a successful session. If any non-routine events occur, the monitors should maintain contact with the volunteer throughout.
If they become anxious
If participants become anxious during the course of hallucinogen action, it is now widely recognized that the appropriate first response is to provide strong personal support and reassurance (O’Brien, 2006). This primarily includes interacting with the volunteer in a comforting and reassuring manner. If the volunteer is behaving anxiously and a negative psychological reaction seems to be escalating, the monitors should convey a solid sense of security and calm, while empathizing with what may be an incredibly intense and unpleasant experience. Attempts to ‘talk down’ the participant (i.e. the use of reality-defining techniques to distract the participant from or attenuate the altered state of consciousness) may be counterproductive and aggravate a difficult reaction (McCabe, 1977). Instead, participants should be reminded to surrender to the experience. Appropriate forms of reassurance may include a supportive touch to the arm or shoulder with verbal reminders that the participant is in a research study, has taken the hallucinogen, and that he or she will return to normal consciousness in ‘a few minutes’ or ‘a few hours’ (or whatever the appropriate estimate may be, depending on the specific drug under study and when it was administered). During an intense hallucinogen-occasioned experience when verbal interactions may be of limited help, a powerful form of reassurance (sometimes called ‘interpersonal grounding’) is simply holding the hand of the participant (McCabe, 1977). Many volunteers report that during such experiences, a reassuring hand provides an incredible sense of stability and connection. Monitors should demonstrate this practice during preparation to normalize hand holding during sessions.
Will this be enough to deal with difficult experiences?
If volunteers have been appropriately screened and the guidelines herein followed, reassurance should be sufficient to diffuse acute psychological distress in the vast majority of cases. For example, in recent studies in our laboratory, in which we have administered high doses of psilocybin to 54 volunteers, reassurance has been sufficient to handle all cases of acute psychological distress that have arisen.
If distress can’t be managed with reassurance alone: 10mg Valium (diazepam), Xanax is less preferable as it takes longer to onset [1] , but if used 0.5mg Xanax is equivalent in effect to 10mg Valium [2]
For cases in which acute psychological distress is insufficiently managed with reassurance alone, treatment with a benzodiazepine anxiolytic is the pharmacological intervention of choice (Abraham and Aldridge, 1993; Frecska and Luna, 2006; O’Brien, 2006). In these cases, we recommend a 10 mg oral dose of diazepam (Grinspoon and Bakalar, 1979), although oral doses of 15–30 mg per hour or every few hours as needed have been recommended for pharmacological treatment of ‘bad trips’ that do not respond to reassurance in emergency department settings (Ungerleider and Frank, 1976). Because of its high lipid solubility, diazepam has a more rapid onset, a shorter time until peak plasma concentration and a shorter duration of therapeutic action than many other benzodiazepines including lorazepam, despite the fact that lorazepam has a shorter elimination half-life (Greenblatt and Shader, 1985; Funderburk, etal., 1988). Although the intravenous route may be considered, the oral route is preferable because intravenous injection procedures may further exacerbate the participant’s anxiety.
Anti-psychotics
Moreover, antipsychotic medications (e.g. risperidone, olanzapine) should be available in the event that an adverse reaction escalates to unmanageable psychosis. However, experienced clinicians have suggested that although antipsychotic medications may reduce psychotic behaviour through sedation, their use may be problematic because the effects may be abrupt, unpleasant and intense and their use may result in subsequent psychological problems (McCabe, 1977; Grinspoon and Bakalar, 1979; Grof, 1980). Furthermore, pretreatment with the antipsychotic haloperidol has been shown to exacerbate the psychosis-like effects of psilocybin (Vollenweider, et al., 1998), suggesting that haloperidol should not be used as a rescue medication. Although not approved for use in the USA, ketanserin (a 5-HT2A antagonist) pretreatment has been shown to attenuate psilocybin effects (Vollenweider, et al., 1998), suggesting possible use as a rescue medication for hallucinogen administration.
Emergency room
Bringing the participant to the emergency department represents an ultimate ‘last resort’ in the treatment of a very difficult (i.e. psychotic) reaction. However, medical evaluation by well-meaning emergency department personnel, who are inexperienced with hallucinogen effects can readily escalate and prolong an adverse reaction. Therefore, all possible efforts should be made to treat a difficult experience in the session context, even if pharmacological intervention is required.
Checking-in
In studies such as ours, in which participants are encouraged to focus their attention inward by wearing eyeshades and listening to music through headphones, our advice is for monitors to occasionally probe the volunteer’s psychological well-being (e.g. ask the volunteer, ‘Would you like to describe where you find yourself?’) to ensure that the volunteer is not experiencing significant anxiety and is in need of support.
Q to figure out: What defines occasionally?
Eyeshades and headphones
the employment of eyeshades and headphones (through which supportive music is played) may contribute to safety by reducing the distractions of environmental stimuli and social pressures to verbally interact with research personnel. This may be especially important for volunteers who are experiencing the effects of a hallucinogen for the first time. Typically, we have kept eyeshades and headphones in place for most of the session. In the latter hours of the session some time is spent with the volunteer sitting on the couch, interacting without eyeshades and headphones, although music may still be played through speakers to provide nonverbal structure and continuity.
Discussing while tripping?
As a whole, we encourage our participants to ‘collect experiences’ to discuss after the drug effects have abated, and discourage attempts to analyse material or communicate excessively while the atypical states of consciousness are still occurring.
No driving for the remainder of the day
Ability to contact the monitor
We have also given the participant the primary monitor’s pager number to call if he or she feels the need for support that evening. Of the 54 volunteers tested at a high psilocybin dose to date, no one has paged the monitor, although volunteers do seem to appreciate this opportunity for additional support.
Post-session
After the session, safety monitoring should continue in the form of one or more post-session meetings (typically the next day) between the primary monitor and participant to ensure psychological stability and provide an opportunity for the volunteer to discuss thoughts or feelings from the session.
A person to discuss with
As with any acute, intense positive or negative emotional experience, participants often feel the need for, and seem to benefit from, additional time for reflecting on the novel thoughts and feelings that may have arisen in the session. Given the potentially intense and unusual psychological nature of hallucinogen effects, the volunteer may have difficulty discussing the experience with others in her or his life. Because the monitors were present during the session when the hallucinogen effects were experienced and have knowledge of a broad range of reported phenomena during drug action, the volunteer may feel more comfortable discussing her or his experience with the monitors than with others.
Acknowledgements
Support for preparation of this manuscript was provided by grants from NIH (R01 DA03889), the Council on Spiritual Practices and the Heffter Research Institute. We thank George Greer, MD, Charles Grob, MD, Robert Jesse, Annie Umbricht, MD and Franz Vollenweider, MD for helpful comments on previous versions of this manuscript. We also thank the staff of the Johns Hopkins psilocybin research studies, whose insights have contributed to these guidelines, including Mary P. Cosimano, MSW and Brian D. Richards, Psy.D. for their roles in screening volunteers and monitoring sessions, and Lawrence P. Carter, PhD, Ryan K. Lanier, PhD, Benjamin McKay, Chad J. Reissig, PhD, and Ryan G. Vandrey, PhD for their assistance in monitoring sessions.
- 15 More Pages
- Psychedelic Psychotherapy: A Strong Endorsement
- The Best Books About Psychedelic Therapy
- Are dabs bad for you?
- How Long Do Shrooms Last?
- Psychedelic Addiction: Treatment
- Study suggests psychedelic drugs increase people's sense of connectedness - to the self, others, and the world
- First Time LSD User? Read this.
- How to Have a Good Shroom Trip
- LSD Test Kits
- How to avoid a bad trip
- An Acid Trip: What is an acid/LSD trip like?
- How long does it take for acid to kick in?
- LSD vs Acid
- What is LSD?
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License .
Have more questions, or want more resources and info? Visit /r/PsychedelicTherapy or /r/Psychedelics .

COMMENTS
👨🌾 Psychedelic Trip Sitter Guide 👨🌾 How to help someone having a bad trip on LSD/shrooms. Please note: It is a criminal offense in the United States and in many other countries, punishable by imprisonment and/or fines, to manufacture, possess, or supply many drugs including most psychedelics, except in connection with ...
cocaine & 2c-x. Status: Caution. Note: The anxiogenic and focusing effects of stimulants increase the chance of unpleasant thought loops. The combination is generally unnecessary because of the stimulating effects of psychedelics. Combination of the stimulating effects may be uncomfortable.
Choose substances: 2C-T-x 2C-x 5-MeO-xxT Alcohol Amphetamines Benzodiazepines Caffeine Cannabis Cocaine DMT DOx DXM GHB/GBL Ketamine LSD MAOIs MDMA MXE Mescaline Mushrooms NBOMes Nitrous Opioids SSRIs Tramadol
To the best of our knowledge, this may be the most comprehensive analysis and review to date on the chemico-biological interactions of these medicines in each of their respective drug classes. We explore the mechanisms by which antidepressants can reduce or amplify the potency of a psychedelic trip and the safety-first steps you can take to ...
Dangerous - These combinations are considered extremely harmful and should always be avoided. Reactions to these drugs taken in combination are highly unpredictable and have a potential to cause death. Instructional Guide, Drug InteractionsTrip BrownSeptember 25, 2018drug combinations, drug interactions, poly pharmy.
Welcome to Trip Sitter We advocate for the safe and responsible use of psychedelics. We believe psychedelics are a valuable tool for self-growth, mind expansion, and mental health — when used responsibly. Education is a key aspect of using these substances effectively. Our guides are designed to provide accurate, up to date information on the use
Research into drug interactions with psilocybin is sparse yet paints an interesting picture of its mechanism. ... ethanol, or antidepressants. Online communities have encouraged using olanzapine as a "trip terminator ... Abagyan R, Thomas K (2021) Concomitant drugs associated with increased mortality for MDMA users reported in a drug safety ...
LSD is generally safe, but very high doses can cause unpleasant side-effects. Darrin Jenkins/Alamy Stock Photo Trip killers. More recently, though, some psychedelic users have been turning to ...
Use WebMD's Drug Interaction Checker tool to find and identify potentially harmful and unsafe combinations of prescription medications by entering two or more drugs in question.
The potential for drug interactions with psilocybin is an important consideration, especially when combined with medications that also affect the serotonin system, such as SSRIs, SNRIs, TCAs, MAOIs, mirtazapine, trazodone, lithium, buspirone, atypical antipsychotics, and others. Some interactions may increase the risk of toxidromes like ...
The Guide to Drug Combinations chart is fairly easy to read. First, simply identify the first substance you would like to reference on the chart's X axis. Next, locate the second substance on the Y axis. The area in the center of the chart where the first substance's column meets the second substance's row will display the anticipated ...
A list of supplements that may help reduce acute anxiety, and therefore help prevent a bad trip on LSD or shrooms. 1. CBD. "Pretreatment with CBD significantly reduced anxiety, cognitive impairment and discomfort in their speech performance, and significantly decreased alert in their anticipatory speech." 1. How to take:
Drug-food/beverage interactions result from drugs reacting with foods or beverages. For example, mixing alcohol with some drugs may cause you to feel tired or slow your reactions. Drug-condition ...
Drug Interaction Checker. Check interactions with multiple drugs, vaccines, supplements, alcohol, food and diseases. Type a drug name in the box above to get started. Not all drugs interact, and not every interaction means you must stop taking one of your medications. Always consult your healthcare provider about how drug interactions should be ...
Pharmacodynamic interactions occur when two drugs that are taken concomitantly have either additive or canceling effects on the body. Pharmacokinetic interactions occur when a drug affects the ...
2C-B & Drug Interactions. Certain drugs or medications may also interact negatively with 2C-B. This substance is largely metabolized by an enzyme called monoamine oxidase (MAO) . It's the main enzyme responsible for breaking down neurotransmitters, including dopamine, serotonin, and norepinephrine.
Summary. A drug interaction happens when a substance affects how a drug behaves in the body. Some substances that can cause interactions include other drugs, supplements, food, and alcohol. Drug ...
Find patient medical information for Triponel (trip-PE-DM) oral on WebMD including its uses, side effects and safety, interactions, pictures, warnings and user ratings.
With acid, start first with 30-40 micrograms. 10 8. You may then increase to a maximum of 60-80 (67) micrograms, then a maximum of 120-140 (133) micrograms, and then a maximum of 170-240 (200) micrograms. 10 8. If you're particularly eager, you can skip the smallest dose and jump to ~67 micrograms first.
Trip has been shown to reduce acid reflux-related symptoms, heal inflammation of the esophagus, and improve patient quality of life more effectively than histamine-2 receptor antagonists (H2 blockers). This drug has an excellent safety profile and a low incidence of drug interactions.
There is still a lack of solid research around interactions between herbal medicines and prescribed drugs. While a few clinical studies and trials have been conducted, it should be noted that some ...
The consent form should also include the approximate timecourse of the drug, the state of knowledge concerning its toxicity profile, and its status as an experimental drug. In addition, the consent form should state that there is a relatively small risk of adverse effects that last for hours to days after the hallucinogen session.
March 20, 2024. 0. The US Food and Drug Administration (FDA) has approved aprocitentan (Tryvio) to lower blood pressure, in combination with other antihypertensive agents, in adults with treatment ...