Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 December 2019

“Patient Journeys”: improving care by patient involvement
- Matt Bolz-Johnson 1 ,
- Jelena Meek 2 &
- Nicoline Hoogerbrugge 2
European Journal of Human Genetics volume 28 , pages 141–143 ( 2020 ) Cite this article
25k Accesses
21 Citations
25 Altmetric
Metrics details
- Cancer genetics
- Cancer screening
- Cancer therapy
- Health policy
“I will not be ashamed to say ‘ I don’t know’ , nor will I fail to call in my colleagues…”. For centuries this quotation from the Hippocratic oath, has been taken by medical doctors. But what if there are no other healthcare professionals to call in, and the person with the most experience of the disease is sitting right in front of you: ‘ your patient ’.
This scenario is uncomfortably common for patients living with a rare disease when seeking out health care. They are fraught by many hurdles along their health care pathway. From diagnosis to treatment and follow-up, their healthcare pathway is defined by a fog of uncertainties, lack of effective treatments and a multitude of dead-ends. This is the prevailing situation for many because for rare diseases expertise is limited and knowledge is scarce. Currently different initiatives to involve patients in developing clinical guidelines have been taken [ 1 ], however there is no common method that successfully integrates their experience and needs of living with a rare disease into development of healthcare services.
Even though listening to the expertise of a single patient is valuable and important, this will not resolve the uncertainties most rare disease patients are currently facing. To improve care for rare diseases we must draw on all the available knowledge, both from professional experts and patients, in order to improve care for every single patient in the world.
Patient experience and satisfaction have been demonstrated to be the single most important aspect in assessing the quality of healthcare [ 2 ], and has even been shown to be a predictor of survival rates [ 3 ]. Studies have evidenced that patient involvement in the design, evaluation and designation of healthcare services, improves the relevance and quality of the services, as well as improves their ability to meet patient needs [ 4 , 5 , 6 ]. Essentially, to be able to involve patients, the hurdles in communication and initial preconceptions between medical doctors and their patients need to be resolved [ 7 ].
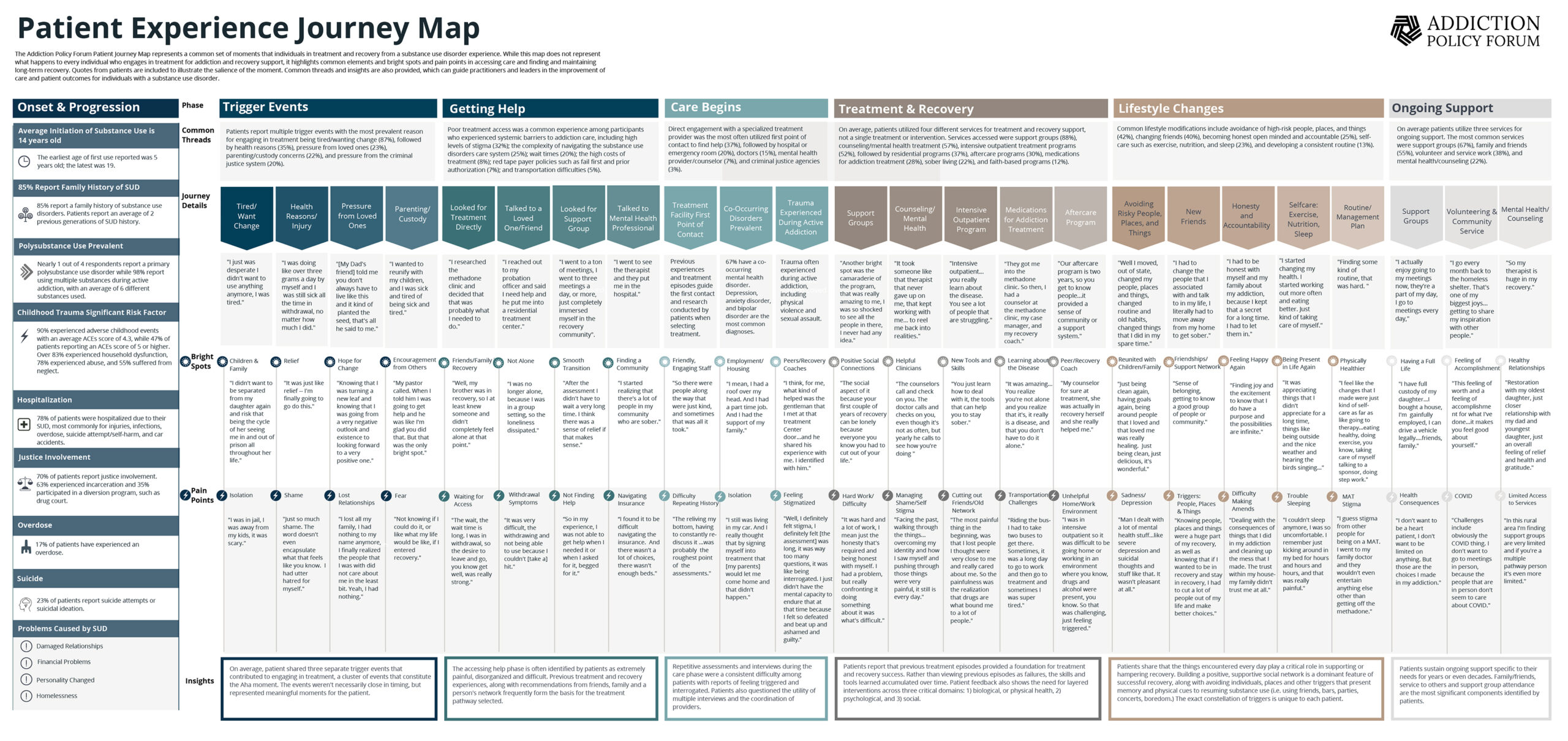
To tackle the current hurdles in complex or rare diseases, European Reference Networks (ERN) have been implemented since March 2017. The goal of these networks is to connect experts across Europe, harnessing their collective experience and expertise, facilitating the knowledge to travel instead of the patient. ERN GENTURIS is the Network leading on genetic tumour risk syndromes (genturis), which are inherited disorders which strongly predispose to the development of tumours [ 8 ]. They share similar challenges: delay in diagnosis, lack of cancer prevention for patients and healthy relatives, and therapeutic. To overcome the hurdles every patient faces, ERN GENTURIS ( www.genturis.eu ) has developed an innovative visual approach for patient input into the Network, to share their expertise and experience: “Patient Journeys” (Fig. 1 ).
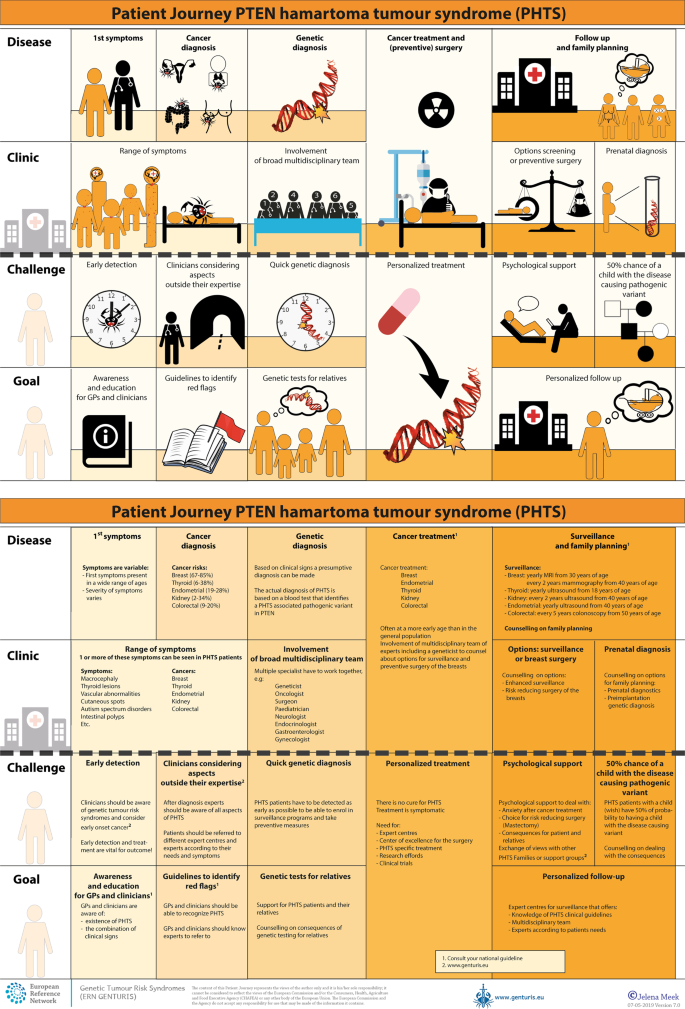
Example of a Patient Journey: PTEN Hamartoma Tumour Syndrome (also called Cowden Syndrome), including legend page ( www.genturis.eu )
The “Patient Journey” seeks to identify the needs that are common for all ‘ genturis syndromes ’, and those that are specific to individual syndromes. To achieve this, patient representatives completed a mapping exercise of the needs of each rare inherited syndrome they represent, across the different stages of the Patient Journey. The “Patient Journey” connects professional expert guidelines—with foreseen medical interventions, screening, treatment—with patient needs –both medical and psychological. Each “Patient Journey” is divided in several stages that are considered inherent to the specific disease. Each stage in the journey is referenced under three levels: clinical presentation, challenges and needs identified by patients, and their goal to improve care. The final Patient Journey is reviewed by both patients and professional experts. By visualizing this in a comprehensive manner, patients and their caregivers are able to discuss the individual needs of the patient, while keeping in mind the expertise of both professional and patient leads. Together they seek to achieve the same goal: improving care for every patient with a genetic tumour risk syndrome.
The Patient Journeys encourage experts to look into national guidelines. In addition, they identify a great need for evidence-based European guidelines, facilitating equal care to all rare patients. ERN GENTURIS has already developed Patient Journeys for the following rare diseases ( www.genturis.eu ):
PTEN hamartoma tumour syndrome (PHTS) (Fig. 1 )
Hereditary breast and ovarian cancer (HBOC)
Lynch syndrome
Neurofibromatosis Type 1
Neurofibromatosis Type 2
Schwannomatosis
A “Patient Journey” is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed information matrix. The journey shows in a comprehensive way the goals that are recognized by both patients and clinical experts. Therefore, it can be used by both these parties to explain the clinical pathway: professional experts can explain to newly identified patients how the clinical pathway generally looks like, whereas their patients can identify their specific needs within these pathways. Moreover, the Patient Journeys could serve as a guide for patients who may want to write, in collaboration with local clinicians, diaries of their journeys. Subsequently, these clinical diaries can be discussed with the clinician and patient representatives. Professionals coming across medical obstacles during the patient journey can contact professional experts in the ERN GENTURIS, while patients can contact the expert patient representatives from this ERN ( www.genturis.eu ). Finally, the “Patient Journeys” will be valuable in sharing knowledge with the clinical community as a whole.
Our aim is that medical doctors confronted with rare diseases, by using Patient Journeys, can also rely on the knowledge of the much broader community of expert professionals and expert patients.
Armstrong MJ, Mullins CD, Gronseth GS, Gagliardi AR. Recommendations for patient engagement in guideline development panels: a qualitative focus group study of guideline-naive patients. PloS ONE 2017;12:e0174329.
Article PubMed PubMed Central Google Scholar
Gupta D, Rodeghier M, Lis CG. Patient satisfaction with service quality as a predictor of survival outcomes in breast cancer. Supportive Care Cancer Off J Multinatl Assoc Supportive Care Cancer. 2014;22:129–34.
Google Scholar
Gupta D, Lis CG, Rodeghier M. Can patient experience with service quality predict survival in colorectal cancer? J Healthc Qual Off Publ Natl Assoc Healthc Qual. 2013;35:37–43.
Sharma AE, Knox M, Mleczko VL, Olayiwola JN. The impact of patient advisors on healthcare outcomes: a systematic review. BMC Health Serv Res. 2017;17:693.
Fonhus MS, Dalsbo TK, Johansen M, Fretheim A, Skirbekk H, Flottorp SA. Patient-mediated interventions to improve professional practice. Cochrane Database Syst Rev. 2018;9:Cd012472.
PubMed Google Scholar
Cornman DH, White CM. AHRQ methods for effective health care. Discerning the perception and impact of patients involved in evidence-based practice center key informant interviews. Rockville, MD: Agency for Healthcare Research and Quality (US); 2017.
Chalmers JD, Timothy A, Polverino E, Almagro M, Ruddy T, Powell P, et al. Patient participation in ERS guidelines and research projects: the EMBARC experience. Breathe (Sheff, Engl). 2017;13:194–207.
Article Google Scholar
Vos JR, Giepmans L, Rohl C, Geverink N, Hoogerbrugge N. Boosting care and knowledge about hereditary cancer: european reference network on genetic tumour risk syndromes. Fam Cancer 2019;18:281–4.
Article PubMed Google Scholar
Download references
Acknowledgements
This work is generated within the European Reference Network on Genetic Tumour Risk Syndromes – FPA No. 739547. The authors thank all ERN GENTURIS Members and patient representatives for their work on the Patient Journeys (see www.genturis.eu ).
Author information
Authors and affiliations.
SquareRootThinking and EURORDIS – Rare Diseases Europe, Paris, France
Matt Bolz-Johnson
Human Genetics, Radboud University Medical Center, Nijmegen, The Netherlands
Jelena Meek & Nicoline Hoogerbrugge
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nicoline Hoogerbrugge .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Bolz-Johnson, M., Meek, J. & Hoogerbrugge, N. “Patient Journeys”: improving care by patient involvement. Eur J Hum Genet 28 , 141–143 (2020). https://doi.org/10.1038/s41431-019-0555-6
Download citation
Received : 07 August 2019
Revised : 04 October 2019
Accepted : 01 November 2019
Published : 04 December 2019
Issue Date : February 2020
DOI : https://doi.org/10.1038/s41431-019-0555-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Care trajectories of surgically treated patients with a prolactinoma: why did they opt for surgery.
- Victoria R. van Trigt
- Ingrid M. Zandbergen
- Nienke R. Biermasz
Pituitary (2023)
Designing rare disease care pathways in the Republic of Ireland: a co-operative model
- E. P. Treacy
Orphanet Journal of Rare Diseases (2022)
Rare disease education in Europe and beyond: time to act
- Birute Tumiene
- Harm Peters
- Gareth Baynam
Development of a patient journey map for people living with cervical dystonia
- Monika Benson
- Alberto Albanese
- Holm Graessner
Der klinische Versorgungspfad zur multiprofessionellen Versorgung seltener Erkrankungen in der Pädiatrie – Ergebnisse aus dem Projekt TRANSLATE-NAMSE
- Daniela Choukair
- Min Ae Lee-Kirsch
- Peter Burgard
Monatsschrift Kinderheilkunde (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Case studies
- Expert advice
Patient journey mapping: what it is, its benefits, and how to do it
We've all been patients at some point, but our journeys were not the same. Patient journey mapping holds the key to unraveling this mystery, providing a strategic lens into the diverse pathways individuals tread throughout their healthcare experiences.
In this article, we'll explore the pivotal role of patient journey mapping in the healthcare industry, uncovering its profound benefits for both providers and patients. From amplifying patient satisfaction to streamlining operational processes, the impact is transformative.
But how does one embark on this journey of understanding and improvement? We'll guide you through the essential steps and considerations, offering insights into the art of crafting a meaningful healthcare patient journey map.
Join us as we peel back the layers of patient experience journey mapping. This powerful tool not only illuminates the complexities of healthcare but also empowers providers to reshape and enhance the patient experience.
- 1.1 Difference from other customer journeys
- 2 Patient journey mapping benefits
- 3 Patient journey stages
- 4.1 Clinical journey maps
- 4.2 Service delivery maps
- 4.3 Digital journey maps
- 4.4 Chronic disease management maps
- 4.5 Emergency care journey maps
- 4.6 Pediatric patient journey maps
- 4.7 Palliative care maps
- 5 How to do patient journey mapping?
- 6.1 Patient-centered care
- 6.2 Streamlined access to care
- 6.3 Effective communication
- 6.4 Education and empowerment
- 6.5 Care coordination
- 6.6 Technology integration
- 6.7 Feedback and continuous improvement
- 6.8 Cultural competency
- 6.9 Emotional support
- 6.10 Efficient billing and financial assistance
- 7 Templates
- 8 Wrapping up
What is a patient journey?

A patient journey is the entire process a person goes through when seeking and receiving a healthcare service. It covers everything from first noticing symptoms or realizing the need for care and medical attention to finally resolving the health issue. The journey involves patient interactions with healthcare professionals, diagnostic procedures, treatment activities, and follow-up care.
Mapping and understanding the patient journey can help boost the quality of hospital care and improve patient satisfaction. By pinpointing challenges, patient communication gaps, and areas for enhancement, care providers can refine their services to better cater to patients' needs. It also contributes to promoting patient-centered care, shifting the focus beyond just treating diseases to considering the overall well-being and experience of the patient.
Difference from other customer journeys
While the concept of patient journey mapping is similar to customer journey mapping , there are unique aspects specific to the healthcare domain. This is how a patient journey differs from any other customer journey:
- Emotional intensity. Health-related experiences often involve heightened emotions, including fear, anxiety, uncertainty, a sense of losing control, and a dependence on others. The emotional aspect is more pronounced in patient journeys compared to customer journeys in most industries.
- Complexity and uncertainty. Healthcare journeys often involve multiple stakeholders, various diagnostic and treatment options, and inherent uncertainties. Navigating these complexities requires a different approach compared to more straightforward consumer experiences. Comparing buying eyeglasses online and visiting a doctor — both are experiences, but how different they are!
- Regulatory and ethical considerations. Healthcare is heavily regulated, and ethical considerations play a significant role there. Patient journeys must align with regulatory standards and ethical principles that other industries don’t have.

- Clinical decision points. Patient journeys involve critical clinical decision points, such as diagnosis and treatment choices. These decisions not only impact the patient's health but also influence the overall trajectory of the journey.
- Care continuum. Patient journeys often extend beyond a single episode of care. They may involve long-term management, follow-up appointments, and ongoing support, creating a continuous care continuum.
- Interdisciplinary collaboration. Healthcare is often delivered by a team of professionals from different disciplines. The patient journey may involve collaboration among physicians, nurses, specialists, and other healthcare providers.
Patient journey mapping benefits

Mapping a patient journey offers a range of benefits that contribute to improving the overall quality of healthcare delivery. Here are some key advantages:
- Visualization of the entire patient journey helps healthcare providers identify critical patient journey touchpoints that impact patient satisfaction and experience and require immediate attention. By paying more attention to these touchpoints, you ensure a more positive overall journey.
- Gaps in care and challenges are highlighted among healthcare professionals. Addressing these issues ensures a more seamless and collaborative approach to patient care.
- Pain points and barriers become evident, enabling healthcare providers to proactively address issues that may hinder effective care delivery.
- Understanding individual patient journeys allows for more personalized ongoing care plans. Tailoring interventions to specific needs and preferences improves patient engagement and outcomes.
- By mapping a patient journey, you can identify resource-intensive stages and areas where efficiency can be improved, enabling a healthcare organization to allocate resources more effectively.
- It's a great way to identify opportunities for smoother transitions between different stages of care, ensuring continuity and preventing gaps in treatment.
- It becomes clear where patient involvement in the decision-making process can contribute to their healthcare journey.
Example: Tom, recovering from surgery, feels more empowered as his healthcare team provides clear post-operative care instructions, making him an active participant in his recovery.
In summary, patient journey mapping provides a comprehensive framework for healthcare improvement, addressing specific challenges at each stage and leading to tangible enhancements in patient experience, communication, and overall care delivery.
Patient journey stages
Patient journeys can differ, and if we take a broad perspective, some key stages would include:
Awareness
This stage involves the patient recognizing symptoms and becoming aware of a potential health issue.
- Key considerations: Pay attention to how patients identify and interpret their symptoms, as well as the information sources they consult.
Example: John notices persistent joint pain and, through online research, suspects it might be arthritis. His journey begins with a heightened awareness of his symptoms.
Seeking information
Patients actively look for information to understand their symptoms, potential causes, and the importance of consulting a healthcare professional.
- Key considerations: Review the information sources patients use and how well they understand the need for professional medical advice.
- Example: Emily researches her persistent cough online, learning about various respiratory conditions and recognizing the importance of seeing a doctor for an accurate diagnosis.
First contact
This marks the initial interaction with the healthcare system, typically through scheduling an appointment with a primary care physician.
- Key considerations: Assess the ease of access to healthcare services and the patient's initial experience with medical professionals.
- Example: Alex schedules an appointment with his family doctor to discuss recent changes in his vision, initiating his journey within the healthcare system.
Diagnostic process
Patients undergo diagnostic tests to identify the root cause of their symptoms.
- Key considerations: Examine the efficiency of the diagnostic process and the clarity of communication about the tests.
- Example: Maria undergoes blood tests and imaging to determine the cause of her abdominal pain, marking the diagnostic phase of her journey.
Treatment planning
Patients receive a diagnosis, and healthcare providers collaborate on creating a personalized treatment plan.
- Key considerations: Evaluate how well the diagnosis is communicated and involve patients in treatment decisions.
- Example: Emily receives a diagnosis of rheumatoid arthritis. Her healthcare team takes the time to explain the condition, discusses various treatment options, and actively involves her in deciding on a comprehensive plan that combines medication, physical therapy, and lifestyle adjustments.
Treatment and clinical care service
Patients initiate the recommended treatment plan, experiencing the day-to-day challenges and improvements associated with their patient journey in a hospital.
- Key considerations: Monitor treatment adherence, side effects, and the patient's overall experience during this active phase.
- Example: Sarah starts chemotherapy for her cancer, navigating the treatment process with the support of her healthcare team.
Psychological support
Patients deal with the emotional toll of managing a health condition, including anxiety, frustration, or isolation.
- Key considerations: Acknowledge and address the emotional aspects of the journey, providing resources for mental health support.
- Example: James copes with the emotional challenges of managing chronic pain, seeking counseling to navigate the psychological impact.
Regular checkups
Patients undergo routine checkups to monitor their health status and adjust treatment plans as needed.
- Key considerations: Ensure consistent communication and scheduling of regular checkups to track progress and address any emerging issues.
- Example: Sarah, diagnosed with hypertension, attends regular checkups where the healthcare team monitors blood pressure, discusses lifestyle adjustments, and ensures medication efficacy. The routine checkups create a proactive approach to managing her condition.
Patients provide feedback on their experiences, allowing healthcare providers to refine and tailor their care.
- Key considerations: Establish mechanisms for patients to share feedback easily and transparently, encouraging an open dialogue.
- Example: John shares his experiences with a new treatment plan, providing feedback on its effectiveness, side effects, and overall impact on his daily life. This feedback loop allows the healthcare team to make timely adjustments and improve the patient's journey.
The stages may vary based on diverse scenarios and individual health circumstances. For instance, when a patient undergoes surgery or faces an acute medical event, the trajectory of their journey can diverge significantly from a more routine healthcare experience.
Factors such as the need for emergency care, hospitalization, and specialized interventions can introduce unique stages and considerations. Additionally, variations may arise due to the specific nature of medical conditions, treatments, and the individual preferences and needs of patients.
Recognizing this variability is crucial for comprehensive journey mapping, allowing for a more nuanced understanding of the patient experience across different healthcare contexts.
Types of healthcare journey maps

Healthcare journey maps can take various forms depending on their focus, purpose, and the specific aspects of the patient experience they aim to understand.
Here are a few types of healthcare journey maps:
Clinical journey maps
Focus: Emphasize the clinical aspects of a patient's experience, including diagnosis, treatment, and recovery.
Purpose: Help healthcare providers understand the medical processes and interventions involved in the patient's journey.
Example: A clinical journey map for a cancer patient would detail the steps from initial symptoms to diagnosis, treatment modalities, and post-treatment care.
Service delivery maps
Focus: Highlight the various touchpoints and services a patient encounters throughout their healthcare journey. Then, detail the back and front processes your team does or has to do during each stage.
Purpose: Enable healthcare organizations to assess the efficiency and effectiveness of service delivery.
Example: Mapping the service delivery for a patient undergoing surgery, including preoperative consultations, surgical procedures, and post-operative care.
Digital journey maps
Focus: Examine the patient's interaction with digital tools and technologies, such as online portals, mobile apps, and telehealth platforms.
Purpose: Help improve the digital aspects of patient engagement and communication.
Example: Mapping the patient's journey when using a telehealth platform for virtual consultations, prescription refills, and accessing medical records.

Chronic disease management maps
Focus: Explore the long-term journey of patients managing chronic conditions.
Purpose: Aid in understanding the challenges and opportunities for supporting patients in their ongoing self-management.
Example: A journey map for a diabetes patient would encompass regular monitoring, medication management, lifestyle adjustments, and periodic checkups.
Emergency care journey maps
Focus: Examine the patient’s experience during emergencies, from the onset of symptoms to emergency room admission and follow-up care.
Purpose: Help optimize response times, communication, and the overall emergency care process.
Example: Mapping the journey of a patient experiencing chest pain, from the initial call to emergency services to the triage process and subsequent cardiac care.
Pediatric patient journey maps
Focus: Tailored specifically for the unique needs and considerations of pediatric patients and their families.
Purpose: Address the emotional and practical aspects of pediatric healthcare experiences.
Example: Such a map is good for a child undergoing surgery to consider the role of parents, age-appropriate communication, and post-operative care.
Palliative care maps
Focus: Center on the patient's journey when facing serious illness, with a focus on providing comfort and support.
Purpose: Enhance the quality of life for patients and their families during end-of-life care.
Example: This kind of journey map suits a patient receiving palliative care when considering symptom management, emotional support, and coordination of services.
The mentioned types of maps cover different patient scenarios and clinical cases. There can also be "AS-IS" and "TO-BE" maps, reflecting the current state of the journey and the desired one, respectively.
All these types of healthcare journey maps offer a nuanced understanding of the diverse aspects of patient experiences, allowing healthcare providers and organizations to tailor their services to meet the unique needs of different patient populations.
How to do patient journey mapping?

Mapping a patient's journey is a thorough process that needs careful planning, teamwork, and analysis. Here's a guide on how to do it:
- Define the objectives
Clearly articulate the goals of the patient journey mapping exercise. Determine what aspects of the patient experience you want to understand and improve. All involved parties should be aware of these goals and agree with them.
- Assemble a cross-functional team
Form a team that includes representatives from various departments, including healthcare providers, administrative staff, patient advocates, and anyone involved in the patient experience.
- Do research
Conduct thorough research to gather quantitative and qualitative data related to the patient experience. This may involve analyzing patient records, studying existing feedback, diving into analytics and market research, and reviewing relevant literature on best practices in healthcare.
- Select a patient segment
Identify a specific patient segment or persona to focus on. This could be based on demographics, health conditions, or specific healthcare services.
Tip: You can leverage your segments or patient personas to craft an empathy map , which is particularly valuable in healthcare.
- Conduct stakeholder interviews
Interview stakeholders, including healthcare professionals and administrative staff. Gather insights into their perspectives on the patient journey, pain points, and opportunities for improvement.
- Define the stages
Outline the patient journey by mapping out each stage and interaction with the healthcare system. This can include pre-visit, during a visit, and post-visit experiences.
Tip: To speed up the process, run a journey mapping workshop with your team. It will help with the next step, too.
- Create the patient journey map
Develop a visual representation of the patient journey. This can be a timeline or infographic that illustrates each stage, touchpoint, and the emotional experience of the patient.
- Identify pain points and opportunities
Analyze the collected data to pinpoint pain points, areas of friction, and opportunities for improvement. Consider emotional, logistical, and clinical aspects of the patient experience.

- Review and validate
Consider collaborative journey mapping . Share the draft patient journey map with stakeholders, including frontline staff and patients, to validate its accuracy. Incorporate feedback to ensure a comprehensive and realistic representation.
- Develop actionable plans
Generate specific, actionable plans based on the identified pain points and opportunities. Each initiative should be feasible, considering resources and organizational constraints.
- Prioritize and implement changes
Prioritize the recommendations based on impact and feasibility. Begin implementing changes that address the identified issues, whether they involve process improvements, staff training, or technology enhancements.
- Monitor and iterate
Continuously monitor the impact of implemented changes. Gather feedback from both staff and patients to understand the effectiveness of the improvements. Iterate on the patient journey map and make recommendations as needed.
- Measure your success
You can also establish KPIs to measure the success of any improvements made based on the patient journey mapping insights. These could include patient satisfaction scores, reduced wait times, or improved communication metrics.
- Document insights (optional)
And keep a record of the lessons learned during the patient journey mapping process. This documentation can inform future initiatives and contribute to ongoing efforts to enhance the patient experience.
- Promote a culture of continuous improvement
Foster a culture within the organization that values continuous improvement in patient care. Encourage ongoing feedback and regularly revisit your journey map to ensure its relevance over time.
By following these steps, healthcare organizations can gain valuable insights into the patient experience, leading to targeted improvements that enhance healthcare quality and patient satisfaction.
How to improve the patient journey?

Striving for a seamless patient journey involves enhancing the overall experience that individuals have when seeking and receiving healthcare services. Here are some strategies to consider:
Patient-centered care
- Prioritize patient needs and preferences.
- Emphasize education and empower patients to actively participate in their healthcare journey.
- Foster open communication and active listening.
Streamlined access to care
- Reduce wait times for appointments and procedures.
- Implement online scheduling and appointment reminders.
- Provide options for virtual consultations when appropriate.
Effective communication
- Ensure clear and understandable communication with patients.
- Provide information about treatment plans, medications, and follow-up care.
- Confirm that patients are well-informed about the potential risks and benefits of treatment options.
Education and empowerment
- Offer educational resources to help patients understand their conditions and treatment options.
- Encourage patients to actively participate in their health management.
- Provide tools for self-monitoring and self-management when possible.
Care coordination
- Improve collaboration and communication among healthcare providers to strengthen care coordination, ensuring a more cohesive and seamless experience for patients throughout their healthcare journey.
- Define and implement standardized protocols for communication and handovers between care teams, reducing the risk of errors and ensuring continuity of care.
- Implement remote monitoring technologies to track patients' health remotely, enabling timely interventions and reducing the need for frequent in-person visits.
Technology integration
- Adopt electronic health records (EHRs) for efficient information sharing.
- Use telemedicine to enhance accessibility and convenience.
- Implement mobile health apps for appointment reminders, medication management, and health tracking.
Feedback and continuous improvement
- Conduct regular surveys to gather specific insights into patient satisfaction, allowing for a more nuanced understanding of their experiences.
- Establish easily accessible channels for patients to provide real-time feedback, ensuring that their voices are heard promptly.
- Respond promptly to patient feedback, address concerns, and communicate any changes or resolutions, fostering a sense of responsiveness and accountability.
Cultural competency
- Train healthcare staff to be culturally competent and sensitive to diverse patient needs.
- Promote diversity in healthcare staff to reflect the communities served, fostering a more inclusive and culturally sensitive environment.
- Recognize and celebrate cultural awareness events within the healthcare setting, fostering an inclusive atmosphere that appreciates the richness of diverse traditions.
Emotional support
- Address the emotional and psychological aspects of healthcare.
- Provide resources for mental health and emotional well-being.
- Consider support groups or counseling services.
Efficient billing and financial assistance
- Simplify billing processes and provide clear information about costs.
- Offer financial assistance programs for patients in need.
- Communicate transparently about insurance coverage and out-of-pocket expenses.
Staff training:
- Train healthcare staff in patient-centered communication and empathy.
- Ensure staff is knowledgeable about the resources available to patients.
- Foster a culture of empathy and compassion in the healthcare environment.
By focusing on these aspects, healthcare providers can contribute to a more positive and effective patient journey. Regularly reassessing and adapting strategies based on feedback and evolving healthcare trends is crucial for ongoing improvement.
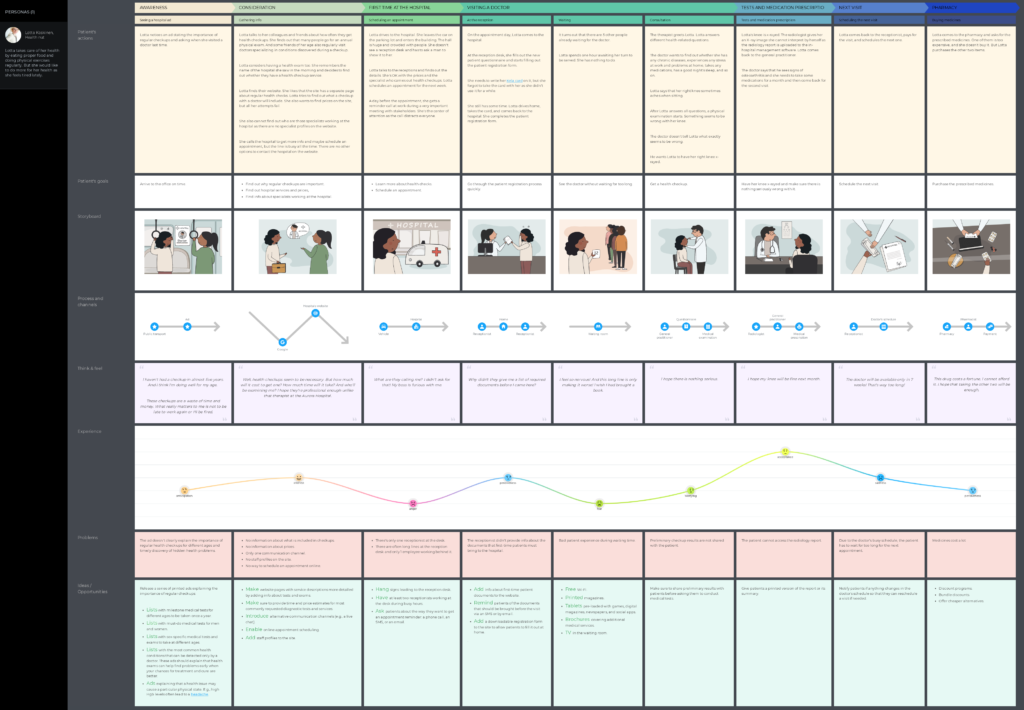
UXPressia already has some healthcare journey map examples:
- Surgical patient journey
This map focuses on the healthcare journey of a patient persona, Robin, from the moment when the patient understands that something is wrong to the recovery period. This journey is long and very detailed.
- Non-surgical patient journey
This map visualizes the journey of a patient, Lotta, who decides to undergo a checkup at a hospital. She schedules a visit, gets a consultation, takes some tests, and starts taking some medicine prescribed by her doctor.
More healthcare and well-being templates are available in our library.
Wrapping up
In wrapping up, think of patient journey mapping as a powerful tool reshaping the healthcare landscape, with the patient's experience taking center stage. It's like creating a roadmap that intricately traces every step of a patient's interaction within the healthcare system.
This deliberate mapping isn't just a plan; it's a compass guiding healthcare organizations toward key points where they can enhance patient satisfaction, simplify access to care, and cultivate a more compassionate and patient-focused healthcare environment. Investing in patient journey mapping is more than a strategy—it's a dedication to raising the bar in care quality, amplifying the patient's voice, and ensuring that every leg of the healthcare journey is characterized by empathy, understanding, and an unwavering pursuit of excellence in patient experience.
Related posts
Rate this post

Search form

The Patient Journey: A Conceptual Framework for Engaging Patients
News | By JLauren | November 30, 2017
Healthcare systems are facing a rapidly growing and almost overwhelming list of outcome measures to meet regulatory, accreditation, and compliance standards.
Current outcome measures, such as pressure injury prevention, surgical complications, and colonoscopy follow-up screening, include elements of patient “compliance” for the healthcare system and provider to be successful. Hospitals struggle with reducing unplanned 30-day readmissions for conditions such as heart failure, pneumonia, and hip/knee replacement when challenged by external variables. These variables include patient lifestyle, access to transportation to rehab or follow-up appointments, and finances to cover prescribed medication costs. In parallel, healthcare systems are seeing more financial incentives to ensure that patients comply with treatment plans post-discharge in an effort to meet outcome standards. [1]
Shared decision-making and early patient engagement are critical
Additional motivators exist for healthcare providers to engage in a shared decision-making (SDM) model. The Centers for Medicare & Medicaid Services and the Agency for Healthcare Research and Quality (AHRQ) [2] both promote the adoption of an SDM model throughout healthcare. This is not a new concept; it is formalizing the structure of effective provider-patient communication. Evidence shows that, in absence of a formal structure, healthcare providers find it difficult to integrate SDM into their routine workflows.
There is also evidence of the importance of engaging patients early in their healthcare journey to identify values and preferences, as this can increase compliance with the plan of care and treatment. [3] Patient activation occurs at the beginning of the patient’s journey. A recent University of Oregon study showed higher-activated patients experienced several benefits compared to patients who were less activated. [4]
Higher-activated patients were:
- More than nine times more likely to feel their treatment plans reflected their values
- Four and a half times more likely to cope with side effects
- Three times more likely to initiate a healthier diet
Delivering education when the patient is ready to learn
Engaging a patient early in the care process with information about testing, diagnosis, treatment, recovery, aftercare, financial considerations, and self-care may present the patient with an extremely overwhelming amount of information that is likely to hit the recycle bin. Instead, Elsevier leverages the patient journey, delivering education when a person is most ready to learn about their phase in the journey. There are many publications that describe the patient journey for specific disease conditions and how the patient moves throughout the continuum of care after entering the healthcare system; however, there is very little written about the journey from the patient’s perspective. A provider may see the patient once symptoms occur or a routine annual test uncovers an abnormal lab value, but after a diagnosis is confirmed, the patient will move somewhat linearly through the journey from diagnosis to treatment, then to recovery or management.
- Prevention and wellness
- Recovery or management and self-care
Prevention and wellness also run throughout the patient’s journey as well as before any diagnosis of an acute or chronic medical condition. Further, if there is an exacerbation of a medical condition, such as COPD or heart failure, this requires additional testing with which the patient must become familiar; sometimes the testing will lead to a new diagnosis, such as ketoacidosis in a diabetic patient. At each phase of the patient journey, new information, learning, and engagement opportunities are evident.
It is critical to deliver the right information at the right time: namely, when the patient is ready to learn about each phase of the disease or condition. Delivering all of the information the patient needs at the end of the acute hospital stay is less than optimal for effective adult learning. As discharge approaches, the patient is preoccupied with getting home from the hospital, making sure his or her pets are taken care of, and wondering how much of the stay will be covered by insurance; asking the patient to also focus on managing insulin for the first time is a tall order. Leveraging tools like the patient portal, outpatient educators, and bridge clinics to deliver the right information at the right time—when the patient is ready to learn—will optimize patient learning.
Engaging the patient early in the diagnosis, delivering the right information at the right time throughout the patient’s journey, and engaging in shared decision-making, particularly with care and treatment options, is a strong approach to ensure that patients increase their activation and ultimately achieve better outcomes.
Dr. Julibeth Lauren, PhD, APRN, ACNS-BC, vice president and editor-in-chief, Elsevier Patient Engagement
Share this:
Tagged under:, most popular, researcher: paxlovid is 'game changer' in treatment of covid-19.
Recent research on Paxlovid shows there is "solid data on its effectiveness," a co-author of the study told HealthLeaders. ...
Bon Secours Mercy Health Invests in Local Supplier of PPE
A new personal protective equipment manufacturing company is set to open in Cincinnati next year. ...
Get the latest on healthcare leadership in your inbox.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Process mapping the...
Process mapping the patient journey: an introduction
- Related content
- Peer review
- Timothy M Trebble , consultant gastroenterologist 1 ,
- Navjyot Hansi , CMT 2 1 ,
- Theresa Hydes , CMT 1 1 ,
- Melissa A Smith , specialist registrar 2 ,
- Marc Baker , senior faculty member 3
- 1 Department of Gastroenterology, Portsmouth Hospitals Trust, Portsmouth PO6 3LY
- 2 Department of Gastroenterology, Guy’s and St Thomas’ NHS Foundation Trust, London
- 3 Lean Enterprise Academy, Ross-on-Wye, Hertfordshire
- Correspondence to: T M Trebble tim.trebble{at}porthosp.nhs.uk
- Accepted 15 July 2010
Process mapping enables the reconfiguring of the patient journey from the patient’s perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital.
Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the patient’s perspective to identify problems and suggest improvements. 1 2 We outline the steps involved in mapping the patient’s journey, as we believe that a basic understanding of this versatile and simple technique, and when and how to use it, is valuable to clinicians who are developing clinical services.
What information does process mapping provide and what is it used for?
Process mapping allows us to “see” and understand the patient’s experience 3 by separating the management of a specific condition or treatment into a series of consecutive events or steps (activities, interventions, or staff interactions, for example). The sequence of these steps between two points (from admission to the accident and emergency department to discharge from the ward) can be viewed as a patient pathway or process of care. 4
Improving the patient pathway involves the coordination of multidisciplinary practice, aiming to maximise clinical efficacy and efficiency by eliminating ineffective and unnecessary care. 5 The data provided by process mapping can be used to redesign the patient pathway 4 6 to improve the quality or efficiency of clinical management and to alter the focus of care towards activities most valued by the patient.
Process mapping has shown clinical benefit across a variety of specialties, multidisciplinary teams, and healthcare systems. 7 8 9 The NHS Institute for Innovation and Improvement proposes a range of practical benefits using this approach (box 1). 6
Box 1 Benefits of process mapping 6
A starting point for an improvement project specific for your own place of work
Creating a culture of ownership, responsibility and accountability for your team
Illustrates a patient pathway or process, understanding it from a patient’s perspective
An aid to plan changes more effectively
Collecting ideas, often from staff who understand the system but who rarely contribute to change
An interactive event that engages staff
An end product (a process map) that is easy to understand and highly visual
Several management systems are available to support process mapping and pathway redesign. 10 11 A common technique, derived originally from the Japanese car maker Toyota, is known as lean thinking transformation. 3 12 This considers each step in a patient pathway in terms of the relative contribution towards the patient’s outcome, taken from the patient’s perspective: it improves the patient’s health, wellbeing, and experience (value adding) or it does not (non-value or “waste”) (box 2). 14 15 16
Box 2 The eight types of waste in health care 13
Defects —Drug prescription errors; incomplete surgical equipment
Overproduction —Inappropriate scheduling
Transportation —Distance between related departments
Waiting —By patients or staff
Inventory —Excess stores, that expire
Motion —Poor ergonomics
Overprocessing —A sledgehammer to crack a nut
Human potential —Not making the most of staff skills
Process mapping can be used to identify and characterise value and non-value steps in the patient pathway (also known as value stream mapping). Using lean thinking transformation to redesign the pathway aims to enhance the contribution of value steps and remove non-value steps. 17 In most processes, non-value steps account for nine times more effort than steps that add value. 18
Reviewing the patient journey is always beneficial, and therefore a process mapping exercise can be undertaken at any time. However, common indications include a need to improve patients’ satisfaction or quality or financial aspects of a particular clinical service.
How to organise a process mapping exercise
Process mapping requires a planned approach, as even apparently straightforward patient journeys can be complex, with many interdependent steps. 4 A process mapping exercise should be an enjoyable and creative experience for staff. In common with other audit techniques, it must avoid being confrontational or judgmental or used to “name, shame, and blame.” 8 19
Preparation and planning
A good first step is to form a team of four or five key staff, ideally including a member with previous experience of lean thinking transformation. The group should decide on a plan for the project and its scope; this can be visualised by using a flow diagram (fig 1 ⇓ ). Producing a rough initial draft of the patient journey can be useful for providing an overview of the exercise.
Fig 1 Steps involved in a process mapping exercise
- Download figure
- Open in new tab
- Download powerpoint
The medical literature or questionnaire studies of patients’ expectations and outcomes should be reviewed to identify value adding steps involved in the management of the clinical condition or intervention from the patient’s perspective. 1 3
Data collection
Data collection should include information on each step under routine clinical circumstances in the usual clinical environment. Information is needed on waiting episodes and bottlenecks (any step within the patient pathway that slows the overall rate of a patient’s progress, normally through reduced capacity or availability 20 ). Using estimates of minimum and maximum time for each step reduces the influence of day to day variations that may skew the data. Limiting the number of steps (to below 60) aids subsequent analysis.
The techniques used for data collection (table 1 ⇓ ) each have advantages and disadvantages; a combination of approaches can be applied, contributing different qualitative or quantitative information. The commonly used technique of walking the patient journey includes interviews with patients and staff and direct observation of the patient journey and clinical environment. It allows the investigator to “see” the patient journey at first hand. Involving junior (or student) doctors or nurses as interviewers may increase the openness of opinions from staff, and time needed for data collection can be reduced by allotting members of the team to investigate different stages in the patient’s journey.
Data collection in process mapping
- View inline
Mapping the information
The process map should comprehensively represent the patient journey. It is common practice to draw the map by hand onto paper (often several metres long), either directly or on repositionable notes (fig 2 ⇓ ).
Fig 2 Section of a current state map of the endoscopy patient journey
Information relating to the steps or representing movement of information (request forms, results, etc) can be added. It is useful to obtain any missing information at this stage, either from staff within the meeting or by revisiting the clinical environment.
Analysing the data and problem solving
The map can be analysed by using a series of simple questions (box 3). The additional information can be added to the process map for visual representation. This can be helped by producing a workflow diagram—a map of the clinical environment, including information on patient, staff, and information movement (fig 3 ⇓ ). 18
Box 3 How to analyse a process map 6
How many steps are involved?
How many staff-staff interactions (handoffs)?
What is the time for each step and between each step?
What is the total time between start and finish (lead time)?
When does a patient join a queue, and is it a regular occurrence?
How many non-value steps are there?
What do patients complain about?
What are the problems for staff?
Fig 3 Workflow diagram of current state endoscopy pathway
Redesigning the patient journey
Lean thinking transformation involves redesigning the patient journey. 21 22 This will eliminate, combine and simplify non-value steps, 23 limit the impact of rate limiting steps (such as bottlenecks), and emphasise the value adding steps, making the process more patient-centred. 6 It is often useful to trial the new pathway and review its effect on patient management and satisfaction before attempting more sustained implementation.
Worked example: How to undertake a process mapping exercise
South Coast NHS Trust, a large district general hospital, plans to improve patient access to local services by offering unsedated endoscopy in two peripheral units. A consultant gastroenterologist has been asked to lead a process mapping exercise of the current patient journey to develop a fast track, high quality patient pathway.
In the absence of local data, he reviews the published literature and identifies key factors to the patient experience that include levels of discomfort during the procedure, time to discuss the findings with the endoscopist, and time spent waiting. 24 25 26 27 He recruits a team: an experienced performance manager, a sister from the endoscopy department, and two junior doctors.
The team drafts a map of the current endoscopy journey, using repositionable notes on the wall. This allows team members to identify the start (admission to the unit) and completion (discharge) points and the locations thought to be involved in the patient journey.
They decide to use a “walk the journey” format, interviewing staff in their clinical environments and allowing direct observation of the patient’s management.
The junior doctors visit the endoscopy unit over two days, building up rapport with the staff to ensure that they feel comfortable with being observed and interviewed (on a semistructured but informal basis). On each day they start at the point of admission at the reception office and follow the patient journey to completion.
They observe the process from staff and patient’s perspectives, sitting in on the booking process and the endoscopy procedure. They identify the sequence of steps and assess each for its duration (minimum and maximum times) and the factors that influence this. For some of the steps, they use a digital watch and notepad to check and record times. They also note staff-patient and staff-staff interactions and their function, and the recording and movement of relevant information.
Details for each step are entered into a simple table (table 2 ⇓ ), with relevant notes and symbols for bottlenecks and patients’ waits.
Patient journey for non-sedated upper gastrointestinal endoscopy
When data collection is complete, the doctor organises a meeting with the team. The individual steps of the patient journey are mapped on a single long section of paper with coloured temporary markers (fig 2 ⇑ ); additional information is added in different colours. A workflow diagram is drawn to show the physical route of the patient journey (fig 3 ⇑ ).
The performance manager calculates that the total patient journey takes a minimum of 50 minutes to a maximum of 345 minutes. This variation mainly reflects waiting times before a number of bottleneck steps.
Only five steps (14 to 17 and 22, table 2 ⇑ ) are considered both to add value and needed on the day of the procedure (providing patient information and consent can be obtained before the patient attends the department). These represent from 13 to 47 minutes. At its least efficient, therefore, only 4% of the patient journey (13 of 345 minutes) is spent in activities that contribute directly towards the patient’s outcome.
The team redesigns the patient journey (fig 4 ⇓ ) to increase time spent on value adding aspects but reduce waiting times, bottlenecks, and travelling distances. For example, time for discussing the results of the procedure is increased but the location is moved from the end of the journey (a bottleneck) to shortly after the procedure in the anteroom, reducing the patient’s waiting time and staff’s travelling distances.
Fig 4 Workflow diagram of future state endoscopy pathway
Implementing changes and sustaining improvements
The endoscopy staff are consulted on the new patient pathway, which is then piloted. After successful review two months later, including a patient satisfaction questionnaire, the new patient pathway is formally adopted in the peripheral units.
Further reading
Practical applications.
NHS Institute for Innovation and Improvement ( https://www.institute.nhs.uk )—comprehensive online resource providing practical guidance on process mapping and service improvement
Lean Enterprise Academy ( http://www.leanuk.org )—independent body dedicated to lean thinking in industry and healthcare, through training and academic discussion; its publication, Making Hospitals Work 23 is a practical guide to lean transformation in the hospital environment
Manufacturing Institute ( http://www.manufacturinginstitute.co.uk )—undertakes courses on process mapping and lean thinking transformation within health care and industrial practice
Theoretical basis
Bircheno J. The new lean toolbox . 4th ed. Buckingham: PICSIE Books, 2008
Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 [online publication 29 April]
Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998; 7 (suppl):S30-6
Graban M. Lean hospitals, improving quality, patient safety and employee satisfaction . New York: Taylor & Francis, 2009
Womack JP, Jones DT. Lean thinking . 2nd ed. London: Simon & Schuster, 2003
Cite this as: BMJ 2010;341:c4078
Contributors: TMT designed the protocol and drafted the manuscript; TMT, MB, JH, and TH collected and analysed the data; all authors critically reviewed and contributed towards revision and production of the manuscript. TMT is guarantor.
Competing interests: MB is a senior faculty member carrying out research for the Lean Enterprise Academy and undertakes paid consultancies both individually and from Lean Enterprise Academy, and training fees for providing lean thinking in healthcare.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Kollberg B, Dahlgaard JJ, Brehmer P. Measuring lean initiatives in health care services: issues and findings. Int J Productivity Perform Manage 2007 ; 56 : 7 -24. OpenUrl CrossRef
- ↵ Bevan H, Lendon R. Improving performance by improving processes and systems. In: Walburg J, Bevan H, Wilderspin J, Lemmens K, eds. Performance management in health care. Abingdon: Routeledge, 2006:75-85.
- ↵ Kim CS, Spahlinger DA, Kin JM, Billi JE. Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med 2006 ; 1 : 191 -9. OpenUrl CrossRef PubMed
- ↵ Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998 ; 7 (suppl): S30 -6. OpenUrl
- ↵ Peterson KM, Kane DP. Beyond disease management: population-based health management. Disease management. Chicago: American Hospital Publishing, 1996.
- ↵ NHS Modernisation Agency. Process mapping, analysis and redesign. London: Department of Health, 2005;1-40.
- ↵ Taylor AJ, Randall C. Process mapping: enhancing the implementation of the Liverpool care pathway. Int J Palliat Nurs 2007 ; 13 : 163 -7. OpenUrl PubMed
- ↵ Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust 2008 ; 188 (suppl 6): S14 -7. OpenUrl PubMed Web of Science
- ↵ King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas 2006 ; 18 : 391 -7. OpenUrl CrossRef PubMed
- ↵ Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 ; published online 29 April.
- ↵ Rath F. Tools for developing a quality management program: proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis). Int J Radiat Oncol Biol Phys 2008 ; 71 (suppl): S187 -90. OpenUrl PubMed Web of Science
- ↵ Womack JP, Jones DT. Lean thinking. 2nd ed. London: Simon & Schuster, 2003.
- ↵ Graban M. Value and waste. In: Lean hospitals. New York: Taylor & Francis, 2009;35-56.
- ↵ Westwood N, James-Moore M, Cooke M. Going lean in the NHS. London: NHS Institute for Innovation and Improvement, 2007.
- ↵ Liker JK. The heart of the Toyota production system: eliminating waste. The Toyota way. New York: McGraw-Hill, 2004;27-34.
- ↵ Womack JP, Jones DT. Introduction: Lean thinking versus Muda. In: Lean thinking. 2nd ed. London: Simon & Schuster, 2003:15-28.
- ↵ George ML, Rowlands D, Price M, Maxey J. Value stream mapping and process flow tools. Lean six sigma pocket toolbook. New York: McGraw Hill, 2005:33-54.
- ↵ Fillingham D. Can lean save lives. Leadership Health Serv 2007 ; 20 : 231 -41. OpenUrl CrossRef
- ↵ Benjamin A. Audit: how to do it in practice. BMJ 2008 ; 336 : 1241 -5. OpenUrl FREE Full Text
- ↵ Vissers J. Unit Logistics. In: Vissers J, Beech R, eds. Health operations management patient flow logistics in health care. Oxford: Routledge, 2005:51-69.
- ↵ Graban M. Overview of lean for hospital. Lean hospitals. New York: Taylor & Francis, 2009;19-33.
- ↵ Eaton M. The key lean concepts. Lean for practitioners. Penryn, Cornwall: Academy Press, 2008:13-28.
- ↵ Baker M, Taylor I, Mitchell A. Analysing the situation: learning to think differently. In: Making hospitals work. Ross-on-Wye: Lean Enterprise Academy, 2009:51-70.
- ↵ Ko HH, Zhang H, Telford JJ, Enns R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc 2009 ; 69 : 883 -91. OpenUrl CrossRef PubMed Web of Science
- ↵ Del Rio AS, Baudet JS, Fernandez OA, Morales I, Socas MR. Evaluation of patient satisfaction in gastrointestinal endoscopy. Eur J Gastroenterol Hepatol 2007 ; 19 : 896 -900. OpenUrl CrossRef PubMed Web of Science
- ↵ Seip B, Huppertz-Hauss G, Sauar J, Bretthauer M, Hoff G. Patients’ satisfaction: an important factor in quality control of gastroscopies. Scand J Gastroenterol 2008 ; 43 : 1004 -11. OpenUrl CrossRef PubMed Web of Science
- ↵ Yanai H, Schushan-Eisen I, Neuman S, Novis B. Patient satisfaction with endoscopy measurement and assessment. Dig Dis 2008 ; 26 : 75 -9. OpenUrl CrossRef PubMed Web of Science
Patient journey 101: Definition, benefits, and strategies
Last updated
22 August 2023
Reviewed by
Melissa Udekwu, BSN., RN., LNC
Today’s patients are highly informed and empowered. They know they have choices in their healthcare, which can put healthcare providers under a lot of pressure to provide solutions and meet their patients’ expectations.
Just like any customer, patients embark on a journey that begins before they ever contact the provider. This makes understanding the journey and where improvements can be made extremely important. Mapping the patient journey can help practitioners provide better care, retain a solid customer base, and ultimately identify ways to improve patient health.
- What is the patient journey?
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end.
The patient journey continues through consultation, where they meet the potential caregiver. That portion of the journey includes interactions with a doctor and support staff, how long they wait to be seen, and the steps taken for diagnosis and treatment.
The patient’s post-care journey includes follow-ups from the healthcare provider, post-treatment care, and billing. For example, if the patient has questions about post-surgery care or how to read their invoice, how quickly their questions are answered and their problems resolved will impact their satisfaction.
Mapping the patient journey helps healthcare providers improve patient satisfaction at every step of the way. By collecting data at each stage and conducting an in-depth analysis, providers can identify patient concerns and make the necessary improvements to meet their patient satisfaction goals.
What is another name for the patient journey?
The term “patient funnel” describes the journey patients take from first learning about a healthcare provider or healthcare product to actually making an appointment or purchase. This “funnel” can be applied to any type of business, describing the stages a customer goes through to obtain a service.
Get a demo from a Dovetail expert
Our team can give you a demo, help you choose the right plan and ensure you get the most out of Dovetail.

- Understanding the stages of the patient journey
Each stage of the patient journey is essential to a positive patient experience . Gathering and analyzing data can alert healthcare providers to potential issues throughout the journey.
Data collection at each of the following stages will give healthcare providers the information they need to make the necessary improvements:
1. Awareness
Awareness is where the patient journey begins. This is when they first research symptoms and identify the need to see a medical professional.
They may consider at-home remedies and get advice from friends, social media, or websites. Once they identify the need for a healthcare provider, they continue their research via review sites, advertising campaigns, and seeking referrals from friends and family.
Determining the way patients become aware they need healthcare and the sources they use for research is important. The data collected at this stage could suggest your organization has an insufficient social media presence, inadequate advertising, or a website in need of an update.
To remedy these shortcomings, you might consider adding informational blogs to your website, performing a social media analysis, or closely monitoring customer reviews.
This stage in the patient journey is where the patient schedules services with the healthcare provider.
This engagement is essential for acquiring new patients and retaining current patients. Patients will contact you in several ways to schedule an appointment or get information. Most will call on the first attempt to schedule an appointment.
This is a crucial touchpoint in the journey. A new patient may become frustrated and move on if they find it difficult to access your services or are placed on hold for a long period or transferred numerous times.
Patient engagement occurs in other ways, such as your online patient portal, text messages, and emails. Your patients may interact differently, so it’s important to gather data that represents their preferred means of communication. Work to make the improvements required to correct access issues and ensure efficient communication.
The care stage can include everything from your patient’s interaction with the front desk to how long they have to wait in the examination room to see a doctor.
Check-in, check-out, admissions, discharge, billing, and of course, the actual visit with the healthcare provider are other touchpoints in the care stage.
There are a couple of ways to gather and analyze this data. Most organizations choose to analyze it holistically, even if it’s collected separately. For example, you might gather data about the patient’s interaction with the front desk, the clinical visit, and the discharge process, but you may want to analyze the care segment as a whole.
4. Treatment
Treatment may be administered in the office. For example, a patient diagnosed with hypertension may have medication prescribed. That medication is the treatment. Gathering information at this stage is critical to see how your patient views the healthcare provider’s follow-up or responses to inquiries.
In most cases, treatment extends beyond the initial clinical visit. For example, a patient might require additional tests to get a diagnosis. Providing the next steps to a patient in a timely manner and letting them know the test results is crucial to patient satisfaction .
5. Long term
A satisfied patient results in a long-term relationship and referrals to friends and family. Most of the data collected at this stage will be positive since the patient is continuing to use your services.
Gathering data after the treatment stage allows you to expand on the qualities that keep patients returning for your services in the long term.
- Benefits of patient journey mapping
The patient benefits from their healthcare provider understanding their journey and taking steps to improve it. Healthcare providers also reap several benefits, including the following:
1. Efficient patient care
When they understand the patient journey, healthcare providers can provide care more efficiently and spend less time and money on unnecessary, unwanted communications.
2. Proactive patient care
Proactive patient care is aimed at preventing rather than treating disease. For example, women who are over a certain age should have an annual mammogram, smokers may be tested for lung disease, and elderly women may need a bone density study. These preventative measures can help keep disease at bay, improve health outcomes, and build trust with patients.
3. Value-based patient care
Patients don’t want to feel they are being charged unfairly for their healthcare. Focusing on the individual patient promotes satisfaction and yields positive outcomes.
The Center for Medicare and Medicaid Services (CMS) has issued recent guidelines for participants that help offset the costs of high-quality care through a reward system.
4. Retention and referrals
Patients who are happy with their journey will keep returning for healthcare, and happy patients equal voluntary referrals. Many providers offer rewards to incentify referrals.
- How to get started with patient journey mapping
Follow the steps below to start the patient journey mapping process:
Establish your patient personas
Journey mapping is a great way to identify your patient’s characteristics so that their experience can be further enhanced.
Some of the following determinations can help you pinpoint your patient’s persona and establish protocols to provide a better service:
How do your patients prefer to communicate? Are they more comfortable with phone calls, texts, or other methods?
How are most patients finding your services? Are they being referred by friends or family members, or are they seeing advertisements?
Would the patient prefer in-person communication or telecommunication?
What are the patient’s expectations of care?
This data can be complex and widespread, but it can give you the information you need to more effectively and efficiently communicate with your patients.
Understand the entire patient lifecycle
Each patient is unique. Understanding the patient lifecycle can avoid confusion and miscommunication.
To positively engage the patient, you’ll need to gather data not only about communication methods but where they are in the patient journey, their health issue, and their familiarity with the healthcare provider’s procedures and treatment options.
Understand the moments of truth
With a few exceptions, most people seek healthcare services when they are ill or have a healthcare issue. These situations can cause patients to feel stressed and anxious. It’s these moments of interaction where compassion, knowledge, and understanding can provide relief and reassurance.
When patients see their healthcare provider, they are looking for solutions to problems. It’s the provider’s opportunity to identify these moments of truth and capitalize on them.
Get the data you need
Healthcare providers can collect vast amounts of data from patients, but the data collected rarely goes far enough in analyzing and determining solutions.
Your patients have high expectations regarding personalized treatment based on data. They want personalized, easy access to medical information and records, responsive treatments and follow-up, and communication in their preferred format.
You need more than clinical data to give patients what they want. You also need personal data that sets each patient apart and ensures a tailored experience.
For example, it might be challenging for parents of small children to contact the clinic and schedule appointments at certain times of the day. As a healthcare provider, you’ll need to be aware of the best times to contact this individual and offer simple methods for scheduling appointments.
Another example is patients with physical disabilities. You can take steps to improve their access to and experience at the healthcare facility.
Encourage referrals and loyalty
Although engagement on social media and online forums is becoming more and more common, the best way for new patients to find you is through referrals. Referrals stem from satisfactory experiences and trust.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze patient research?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 29 June 2023
Last updated: 27 June 2023
Last updated: 22 July 2023
Last updated: 18 July 2023
Last updated: 2 August 2023
Last updated: 14 July 2023
Last updated: 19 July 2023
Last updated: 31 July 2023
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next.

Users report unexpectedly high data usage, especially during streaming sessions.

Users find it hard to navigate from the home page to relevant playlists in the app.

It would be great to have a sleep timer feature, especially for bedtime listening.

I need better filters to find the songs or artists I’m looking for.
Log in or sign up
Get started for free
Understanding the Patient Journey through Treatment and Recovery
By Kayla Zawislak, LSW, CADC, Director of Patient Engagement, Addiction Policy Forum
There is a common saying in the field of addiction science: “Nothing about us, without us.” An important reminder during Recovery Month and every month working in the addiction field. Yet there is still a pronounced absence of systematic feedback from patients in recovery and receiving treatment for substance use disorders (SUDs). Barriers to engaging individuals in recovery can include social stigma, confidentiality concerns, and fear of exposure or retribution. And yet patients have a wealth of information and guidance on treatment for SUDs and long-term recovery that can benefit the research community, clinicians, and providers, as well as other patients and families.
To help tell this story, our team at Addiction Policy Forum developed a Patient Journey Map for the substance use disorder treatment and recovery experience. Patient journey mapping is a process common in the healthcare field that helps visualize the process patients go through to receive care for a specific illness. It is meant to help identify and understand the details of all patient touch points within a specific treatment experience.
Our patient journey map underscores the obstacles and positive points patients encounter across seven distinct phases. The qualitative study included 60 individuals in recovery across 22 states and Canada.
We at the Addiction Policy Forum knew that each patient's journey to treatment and recovery is unique, and sharing diverse experiences across different types of substance use disorders, genders, races, ethnicities and ages was critical. We conducted one-on-one life course history interviews to empower patients with lived experience to tell their unique stories in a semi-structured interview process with time to reflect and describe their journeys.
To create a meaningful visualization, we created a layered map that spanned seven distinct phases from onset and progression, trigger events, getting help, care begins, treatment and recovery, lifestyle changes, and ongoing support. The map highlights bright spots that were helpful to the patients within each of these phases, as well as pain points or challenges those individuals faced. Our map also focused on reinforcing the finding through patient quotes – telling the story through their own words. These important testimonials were included in the map to center the data on the lived experience of persons in recovery. Each quote gives a face and experience to every data point that is shared, which gives the viewer a deeper understanding of the patient journey.
1. Significant barriers encountered as patients try to find help.
Barriers include high levels of stigma; the complexity of navigating the substance use disorders care system; long wait times; the high costs of treatment; red tape payer policies such as fail first and prior authorization; and transportation difficulties.
One patient shared: “I think stigma is a really big one, though, just within myself, not with seeking help outside, but in having to confront that I have this thing that is frowned on in society.”
2. Children and family are cited most frequently as the bright spots early in treatment.
Bright spots, or positive moments early in treatment, included children and family, relief, hope for change, and encouragement from others. This is important because addiction is an isolating disease that can easily cloud one’s future. Therefore, it is imperative that individuals have connections with meaningful people within their lives, begin to see that their life can be different, and know that they are not alone.
3. Patients utilize multiple services, not a single intervention.
On average, patients utilized four different services for treatment and recovery support, not a single treatment or intervention. Patient feedback shows the need for layered interventions across three critical domains: 1) physical health, 2) psychological, and 3) social interventions. Lifestyle changes are also cited by patients to be as critical to success as treatment and recovery services, such as changing friends, avoidance of high-risk people, places, and things, becoming honest and accountable, new hobbies, and developing self-care habits around exercise, nutrition, and sleep.
We believe this feedback from a diversity of patients is the key to advancing care and innovation for addiction. Our team even analyzed word usage in the patient journey interviews. The themes and most common words describing active addiction included homelessness, job loss, trauma, children and custody issues and health challenges. In contrast, common themes related to recovery include improved relationships, experiencing life, freedom, health and wellness and words like good, love and amazing.
One patient shared: “This feeling of worth and a feeling of accomplishment for what I've done... It makes you feel good about yourself.”
It is our hope that the patient journey map can help inform clinicians, families, individuals in recovery, and so many others about the key components of treatment and recovery and understand the barriers and pain points we face as a community. Above all, we hope this project celebrates the freedom and beauty of recovery from substance use disorders.
Author Bio: Kayla Zawislak, LSW, CADC has worked at APF for the last four years where she is the Director of Patient Engagement. She works closely with those with a substance use disorder and their loved ones through APF's helpline, smartphone application, virtual recovery meetings, and research projects. Connect with her on LinkedIn or via email at [email protected]
Root out friction in every digital experience, super-charge conversion rates, and optimize digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Explore the platform powering Experience Management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Artificial Intelligence
- Market Research
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results, live in Salt Lake City.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Sector Specific
- Patient Experience
- Patient Journey Mapping
Try Qualtrics for free
Your complete guide to patient journey mapping.
15 min read Healthcare organizations can increase patient retention and improve patient satisfaction with patient journey mapping. Discover how to create a patient journey map and how you can use it to improve your organization’s bottom line.
What is the patient journey?
The patient journey is the sequence of events that begins when a patient first develops a need for care. Rather than focusing on service delivery, the patient journey encompasses all touchpoints of a patient’s healthcare experience–from locating healthcare providers and scheduling appointments, to paying the bill and continuing their care after treatment.
Examining the patient journey is essential to improving the patient experience. Not all interactions a patient has with your organization are weighted the same. Gathering patient feedback and understanding perceptions all along the patient journey can help you to identify moments of truth : the touchpoints that have the biggest impact on patient loyalty.
Download eBook: The 3 steps to driving human-centered healthcare experiences
The patient journey vs. the patient experience
Unlike traditional patient experience measurement, the patient journey looks not only at service delivery but also at the steps the patient takes before and after they engage directly with your organization. It recognizes that patient interactions with a healthcare system go well beyond the walls of the medical facility itself.
What are the stages of the patient journey?
There are several stages along the patient journey. When gathering patient feedback, you should make sure to capture insights at each of these stages.
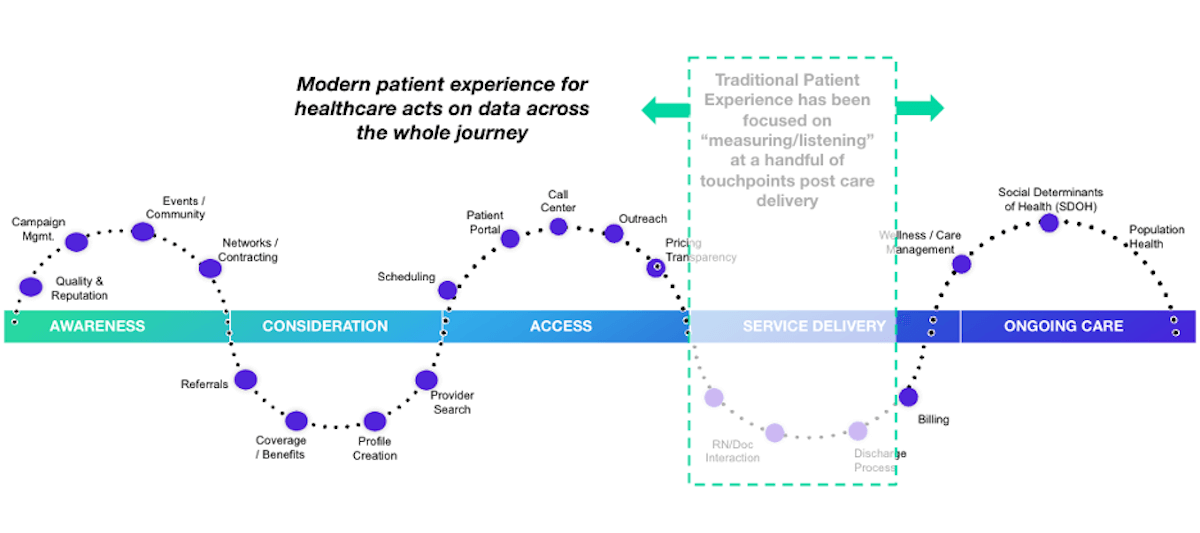
Stage 1: Awareness
The patient journey starts with awareness. In this stage, the patient identifies a need for care and begins searching for care providers. Examples of how patients learn about healthcare providers include online searches, review sites, marketing campaigns, networking, and community involvement.
Stage 2: Consideration
In the consideration stage, the patient weighs their options to determine if your health system can meet their needs. Factors patients consider include referrals, coverage and benefits, recommendations, access, and ratings and reviews. Often in this stage, patients interact with your website or social media pages or contact you via phone or email during this stage.
Stage 3: Access
The access stage is where the patient decides to schedule services with your healthcare organization. Direct patient engagement with your organization increases during this stage. You’ll engage with patients in a variety of ways including phone calls, the patient portal, text messages, and emails as part of the scheduling and new patient acquisition process.
Stage 4: Service delivery
The service delivery stage relates to the clinical care provided to your patients. Encompassed in this stage are the clinical visit itself, check-in and check-out, admission and discharge, and billing. Traditional patient satisfaction measurement centers around this stage of the patient journey.
Stage 5: Ongoing care
The ongoing care stage of the patient journey involves patient engagement that occurs after the interactions directly related to service delivery. In addition to wellness and care management, this stage may address social determinants of health and population health.
What is a patient journey map?
The best way to utilize the patient journey to enhance patient experiences is by journey mapping. A patient journey map is a visual tool that illustrates the relationship a patient has with a healthcare organization over time.
Patient journey mapping helps stakeholders to assess the patient experience from multiple perspectives. Journey maps provide a way to visualize the internal and external factors affecting patient flow and the different paths patients must take in order to reach their care goals.
What are the benefits of patient journey mapping?
Patient journey mapping can help you to visualize all of the steps patients take throughout the entire process of seeking, receiving, and continuing care. Creating a patient journey map is useful to identify pain points and gaps in care. Mapping the patient journey makes it easier to develop solutions that make a more seamless experience within your healthcare system.
Patient journey mapping benefits include:
- Creating shared ownership of the patient experience
- Refining your patient listening strategy
- Aligning your organization with a common view of the patient experience
- Measuring gaps between the intended experience for your patients versus the actual experience
- Identifying and resolving common pain points for your patients
Four types of patient journey maps
When creating a patient journey map, there are four types to consider. Each type of map has an intended purpose. You might start your patient journey mapping with only one type and incorporate the others as your efforts progress.
Current state
A current state journey map tells the story of what patients do, think, and feel as they interact with your organization today. This type of patient journey map is ideally created using patient data and observational data.
The current state journey map is best for driving incremental improvements to enhance the patient experience.
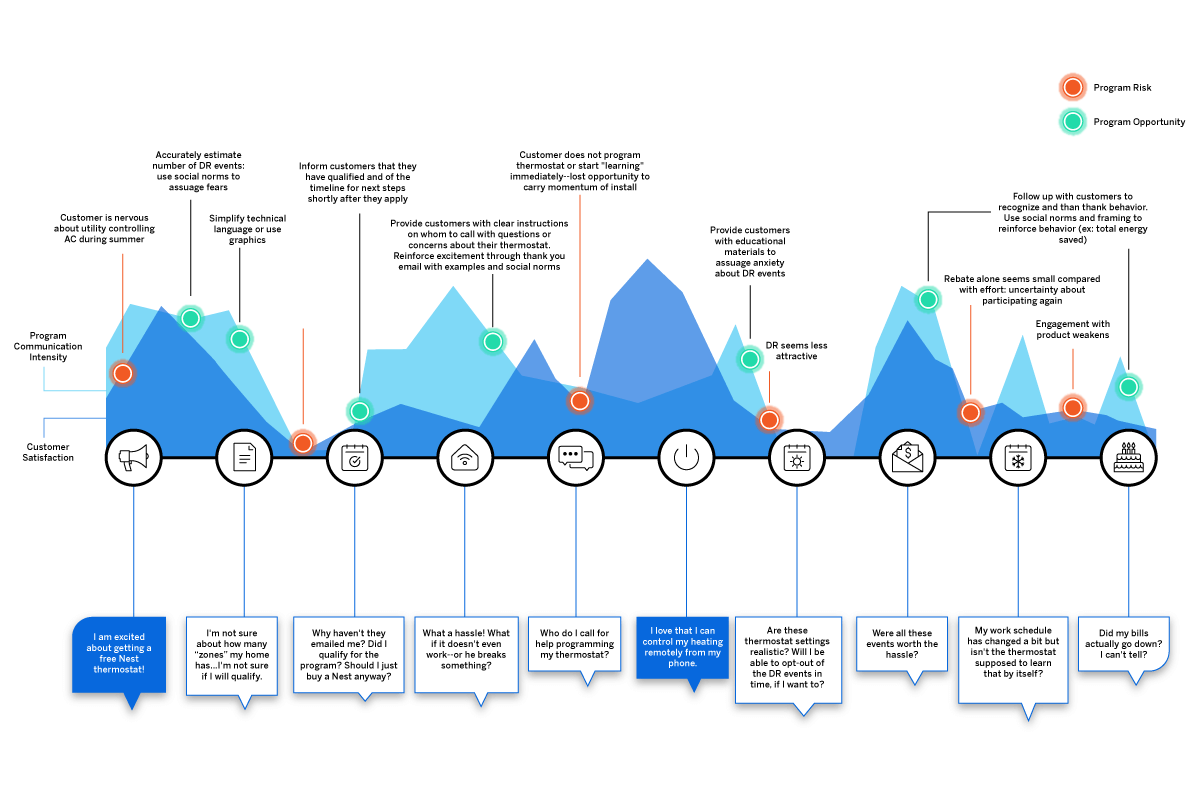
Future state
A future state patient journey map tells the story of what you want your patients to do, think, and feel as they interact with your organization in the future. This type of map should capture the ideal journey you’d like to see for your patients.
The future state journey map is an effective tool to drive strategy, align teams, and communicate your visions for new services, processes, and experiences.
Day in the life
A day in the life patient journey map illustrates what your patients do, think, and feel today, within a specific area of focus. Patient personas are particularly useful when creating day in the life maps; these are discussed in greater detail below.
This type of patient journey map is intended to capture what your patients experience both inside and outside of the healthcare system. Day in the life maps are valuable to address unmet needs and determine how and when you can better engage your patients.
Service blueprint
A service blueprint is a simplified diagram of a current state or future state patient journey map. In the service blueprint, you add layers to illustrate the systems of people, processes, policies, and technologies surrounding each patient touchpoint.
For current state patient journey maps, the service blueprint can help to identify root causes of pain points. For future state, the service blueprint is helpful to visualize the systems or processes that can be put in place to support the intended patient experience.
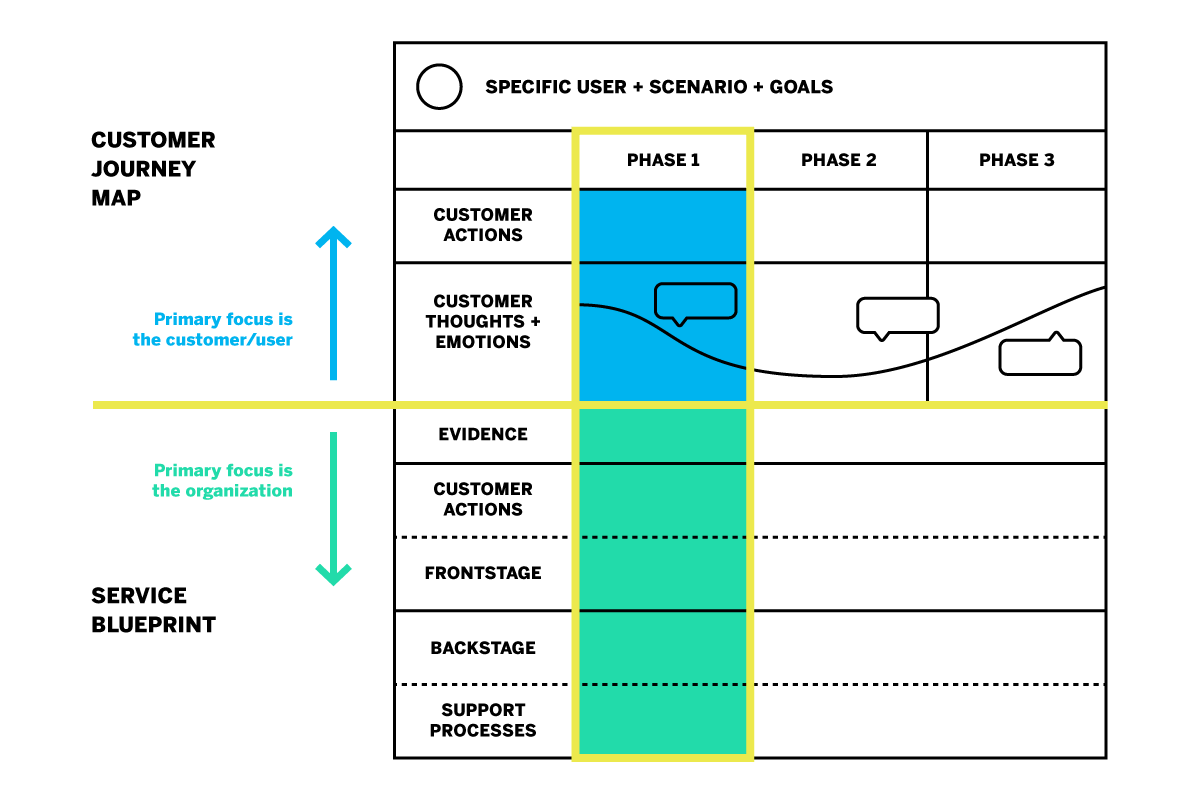
How do you create a patient journey map?
Now that you know about the different types of patient journey maps and their roles in driving patient experience improvement, how do you get started on creating your own?
The most useful maps are those which can expound upon each touchpoint of the healthcare journey with operational data, such as patient demographics, as well as real patient insights and perspectives. Using a platform that can capture this data will aid significantly in your patient journey mapping process.
Patient journey mapping: getting started
Before you get started, it’s a good idea to engage individuals across all departments and include input from multiple stakeholders. Once you’re ready, follow these steps to begin creating an effective patient journey map.
Identify your target audience
What type of patient journey will you be mapping? There may be varying patient journeys within your organization; for instance, an oncology patient’s journey will look very different from that of an expectant mother. The journey of a patient with health insurance will differ from that of a patient without insurance. To map the patient journey, you’ll want to create robust patient profiles you can use to segment and track like-populations throughout the healthcare experience.
Establishing patient personas and segments
Not every patient will have the same healthcare goals. Creating patient personas based on behaviors and preferences is a good way to differentiate the needs and more clearly understand the perspectives of the unique populations you serve.
The ideal patient persona will include the following information.
- Demographic information such as age group, gender, or location
- Healthcare-specific goals, conditions, and treatments
- Healthcare-specific challenges/pain points
- Engagement patterns and expressed feedback
- How your services fit into their life
- Barriers to care
Specify a goal for the patient’s journey
The patient personas you create will all have unique goals within the care journey. The patient has a specific goal in mind when they initiate contact with your organization, whether it is treatment of symptoms, a diagnosis for chronic issues, or surgery.
Every interaction along the patient journey influences how successful the patient feels about achieving this goal. When mapping the patient journey, you’ll want to consider how the various touchpoints affect the patient’s ability to meet this goal.
Identify the patient’s steps to accomplish their target goal
This step is about how the patient views their care journey within your health system–not about the actual processes and systems your organization has in place. Effective patient journey mapping requires you to see how the patient navigates the journey through their point of view.
Omni-channel listening is a valuable strategy in this step of journey mapping. Listening to your patients across all the channels can provide a clearer picture of their perceptions and behaviors as they engage with your organization.
Some steps the patient takes may not even include your organization, but might still affect how they are interacting with you directly. For example, if a patient logs into their health insurance portal to check coverage for healthcare services, they are not engaging with your organization but this is still a part of their care journey that may feed into their interactions with your organization later on.
Uncover perceptions along the journey
Gather patient feedback along the touchpoints of the care journey to identify key emotional moments that may disproportionately shape attitudes. These insights shed light on what’s working and what’s not; they can also be used to highlight the moments of truth that contribute to patient loyalty.
Patient perceptions are an important piece of patient journey mapping; it will be difficult to drive action without them.
Additional tips for creating the ideal patient journey map
Patient journey mapping is a continuous process. Creating the map is the first step, but the true value is dependent upon maintaining the map as you continue to gather insights and refine processes.
This leads to the second tip: be ready to take action! You can use a patient journey map to draw conclusions about your patients’ experiences within your organization, but awareness alone will yield no benefits. The journey map is a valuable tool to be used in your wider improvement efforts.
How do you drive action using a patient journey map?
Once your patient journey mapping is complete, it’s time to put it to good use. Here are five ways patient journey maps can be used to drive action.
Identify and fix problems
The visual layout of a journey map makes it ideal to identify gaps and potential pain points in your patient journeys. This will give you a better understanding of what’s working and what’s not. It will also help you to visualize where and how improvements can be made.
Build a patient mindset
Patient journey mapping enables you to incorporate more patient-centric thinking into your processes and systems. Use your map to challenge internal ideas of what patients want or need. Invite stakeholders to navigate the touchpoints along the healthcare journey to gain perspective.
Uncover unmet patient needs
By mapping the patient journey, you can build stronger patient relationships by listening across all channels to determine where experiences are falling short or where unmet needs emerge. This enables you to look for opportunities to expand alternatives, streamline initiatives, and create new, engaging ways for your patients to share feedback.
Create strategic alignment
Utilize your patient journey map to prioritize projects or improvement efforts. It can also help you to better engage interdepartmental staff to better understand policies and work together toward patient experience goals.
Refine measurement
Patient journey mapping is a great resource to use when defining patient satisfaction metrics and identifying gaps in how you currently gather insights.
How does patient journey mapping increase your bottom line?
Patient journey mapping can increase your bottom line by laying the foundation for improved patient satisfaction and higher retention.
Organizations across all industries are looking to understand customer journeys in order to attract and retain customers by gaining deeper insights into what drives the consumer experience.
As healthcare becomes more consumer-driven, health systems must similarly map the patient journey to improve the patient experience and boost retention. The cost of patient acquisition, combined with the fact that patients are willing to shop around for the best healthcare experience, means success depends on creating the most seamless patient journey possible.
The tools for success
For the most impactful patient journey mapping experience, you’ll want the ability to link your operational and experience data to your journey map’s touchpoints. Insights about what has happened at each touchpoint, as well as why it is happening, empower you to create experiences that meet patient expectations and drive up satisfaction.
Here are some best practice considerations as you develop your patient journey mapping strategy:
- Create a shared understanding throughout your health system of how your patients interact with your organization, and you’ll know the roles and responsibilities of your different teams
- Design a unique patient journey based on multichannel, real-time feedback from the patient
- Consider the frequency with which topics emerge in feedback, as well as the emotional intensity behind them to zero in on what improvements can drive the greatest impact
- Develop empathy and collaboration between teams, working together to achieve the same outcome
- Drive a patient-centric culture by developing a shared sense of ownership of the patient experience
- Connect your operational patient data with your patient experience feedback in one system
- Leverage a closed-loop feedback system that triggers actions for immediate responses to patient concerns
Qualtrics’ XM Platform™ is designed to support all of these actions throughout the journey mapping process.
The 3 steps to driving human-centered healthcare experiences
Related resources
Patient feedback 15 min read, healthcare branding 13 min read, patient journey 10 min read, patient experience 12 min read, symptoms survey 10 min read, nurse satisfaction survey 11 min read, cahps surveys 6 min read, request demo.
Ready to learn more about Qualtrics?

Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps
The Patient's Voice | HCM: Understanding the Patient Journey From Diagnosis to Treatment
Cardiology Magazine

As with any disease, the first step towards treatment starts with a diagnosis. Along with feeling seen and heard, starting to have answers helps to relieve concerns and empowers patients to manage their symptoms. Unfortunately, for patients with hypertrophic cardiomyopathy (HCM), the gap between the onset of symptoms and official diagnosis can be long and frustrating. A survey of patients with diagnosed HCM conducted by the ACC and the Hypertrophic Cardiomyopathy Association (HCMA) offers a closer look at some of the challenges along the path to HCM diagnosis and management in an effort to close this gap and optimize care and outcomes.
According to estimates, between one in 500 and one in 250 patients have HCM, but only about 100,000 patients have been formally diagnosed with the disease. One reason could be the disparities in cascade or family screening, which could catch HCM before symptoms appear. Of the 608 patients surveyed, only 13% had pursued medical care because a family member was diagnosed with HCM or experienced a sudden cardiac arrest, while only 10% listed a family history of heart disease as their reason for seeking a medical appointment. Notably, only a very small number of those surveyed took part in cascade or family screening (3%) or genetic testing (14%).
In contrast, experiencing symptoms consistent with HCM was the most common reason (for 89%) for seeking medical care: dyspnea in 48%, heart murmur (36%), arrhythmia (35%), dizziness (35%), reduced exercise capacity (27%) and fatigue and weakness (27%). Chest pain/pressure when exercising as well as chest pain/pressure at rest were reported by about a quarter of respondents. About two-thirds said they had multiple symptoms.
Dyspnea was more commonly reported by women than men (52% vs. 39%) and those who reported worse health in the past year (57%). In addition, dyspnea was more frequently reported as the initial symptom by patients ultimately diagnosed with obstructive HCM and mid-cavity HCM.
Time to Diagnosis
According to estimates, between one in 500 and one in 250 patients have HCM, but only about 100,000 patients have been formally diagnosed with the disease.
From the start of symptoms to the time of HCM diagnosis, it took five years or more for nearly 50% of patients. Most patients (two-thirds) surveyed experienced symptoms by the time they were 40 years old, but only about 40% gained a diagnosis by that age.
Women were more likely than men to report a gap or delay of five years or more between initialing experiencing symptoms and being diagnosed (52% vs. 37%).
Once patients sought care for their symptoms, with the majority seeing a cardiologist (43%), followed by a family or primary care physician (33%), two-thirds reported receiving a correct diagnosis, with more than half saying it took less than one year. The data indicate a true opportunity to improve time to diagnosis for nearly a third of the patient community.
The majority of those surveyed noted that echocardiography and ECG were the most common tests conducted (72% and 66%, respectively), followed by Holter/event monitoring, exercise stress testing and cardiac MRI. Those who received genetic testing, cascade MRI or cascade screening were among those most likely to report a correct diagnosis.
Some 37% of patients noted receiving an incorrect diagnosis or no diagnosis at all. Of the incorrect diagnoses, heart murmur was the most common, followed by hypertension, anxiety/panic attacks and asthma.
Of note, a correct diagnosis of HCM was more likely for patients who first saw an HCM specialist (only 3% of those surveyed) or a cardiologist, than those who initially saw a primary care or internal medicine physician.
HCM Takes a Toll
The Hypertrophic Cardiomyopathy Association (HCMA) has been serving the HCM spectrum disorder community since 1996.
The survey conducted by the ACC/HCMA on the patient experience shows a high level of emotional and psychological toll on patients with HCM. While it is important to ensure patients have strong clinical support for their physical symptoms, we must also ensure support for the significant emotional burden of having a chronic genetic cardiac disease.
The HCMA has programs to support patients and their families through the uncertainty that life with HCM can present. Learn more about the HCMA at 4hcm.org .
The survey highlights important opportunities for continued clinician and patient education on HCM, whether it's understanding the many signs and symptoms which can be unpredictable or knowing when to seek screening based on risk factors like family history. Only 33% of those surveyed felt they could find a clinician who understands HCM and could treat it.
Developing tools to help friends, family and others support those living with HCM is also an opportunity for closing gaps in care. More than half of respondents said their friends and family do not understand the disease and how it affects daily life. Helping patients navigate diet and exercise is another area for growth. For example, while 81% of patients said they knew exercise is good for them, 62% were afraid of pushing their heart too much. This was especially true among women and those who had indicated worsening health status in the past year. The HCMA has been suggesting that exercise prescriptions by the physician for patients with HCM would contribute to teaching patients how to safely be active and that this may improve their overall quality of life.
Living with HCM is exhausting said half of respondents and managing stress and depression is challenging. For younger patients, it was more challenging to manage the risks, feel in control of the disease and to plan ahead, and they are concerned about sudden death, a lifetime of uncertainty, emotional distress, access to experts and the impact on children and family. Compared with the past year, a third of a patients said their health status was worse, while better outcomes were reported by patients who saw an HCM expert or went to a center of excellence.
According to one patient, "It has been confusing living with the symptoms (dyspnea, weight gain, tiredness/weakness). I, admittedly attributed the worsening symptoms to getting older, gaining weight, and COVID keeping me from getting out and going to the gym. I was shocked to find out there was a real reason for feeling the way I did. I am grateful to have a cardiologist who recognized HCM and who recommended surgery when the medicines no longer controlled the disease. It's a bit of a 'hidden disease' and I'm sure I'm not alone in saying that you tend to hide the symptoms and keep a lot of it to yourself. The HCMA has been a valuable resource navigating this disease."
Financial burdens are also great, with one-third of survey respondents noting HCM taking a toll on their pocketbooks as a result of high costs associated with medications, procedures and/or travel to see an expert. In the past six months alone, nearly half of all participants reported a major event that required either an urgent appointment with their physician, a trip to the emergency department, overnight hospitalization and/or missed work for 14%.
HCM Toolbox
Looking for more on HCM? Add these ACC clinician and patient resources to your toolbox.
- ACC HCM Guideline Hub
- JACC Interactive HCM Genetic Screening Tool
- Free Online Course: ACC Raising Awareness and Understanding of HCM
- CardioSmart Patient Education: HCM
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Prevention, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Echocardiography/Ultrasound, Magnetic Resonance Imaging, Diet, Exercise, Stress
Keywords: ACC Publications, Cardiology Magazine, Quality of Life, Cardiologists, Depression, Dizziness, Exercise Tolerance, Financial Stress, Friends, Panic Disorder, Physicians, Primary Care, Uncertainty, Cardiomyopathy, Hypertrophic, Echocardiography, Electrocardiography, Genetic Testing, Magnetic Resonance Imaging, Cine, Risk Factors, Emergency Service, Hospital, Psychological Distress, Patient Outcome Assessment, Internal Medicine, Hospitalization, Family, Heart Murmurs, Prescriptions, Primary Health Care, Weight Gain, Weight Gain, Surveys and Questionnaires, Arrhythmias, Cardiac, Chest Pain, Dyspnea, Anxiety, Asthma, Fatigue, Diet, Exercise
You must be logged in to save to your library.

The Latest From Cardiology
Read the entire July issue by clicking the links below!
Editor's Corner | Transplanting Ourselves Into Summer
Cover Story | Trends in Advanced Heart Failure Therapy: Update on Cardiac Transplantation
Feature | ACC OutFront: Empowering Practice Change Through Education and Action
Conversations With Experts | Dual Antiplatelet Therapy Post PCI: When and How to De-Escalate
Feature | The U.S. Medical Soccer Team: Building a Physician Community Through Soccer
Peripheral Matters | Transforming Acute PE Care: Standardizing Management to Improve Outcomes
From the Members Sections | Call to Action: Protecting the Hearts of the Unhoused
Quality Improvement For Institutions | NCDR Research Guides Practice, Improves Outcomes
Prioritizing Health | Know Before They Go: Helping Patients Navigate Summer Travel
The Pulse of ACC
Heart of Health Policy
Number Check | By The Numbers: It's Summer. Its Vacation Time!
Just One More | ACC Statement on Gun Violence and Workplace Safety
JACC in a Flash
Journal Wrap
JACC Journals on ACC.org
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Contact Member Care
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
Understanding the Cancer Patient’s Treatment Journey

Cedars-Sinai Tower Hematology Oncology
The intricate interplay between the built environment and its occupants is particularly vital in the context of healthcare. To truly advance healthcare facility design, it is essential to examine how the design of the physical space directly impacts patient health outcomes. By synthesizing this effort with insight into our clients’ evolving challenges, architects can improve the treatment experience through research-informed design. This approach is especially imperative for the design of cancer treatment centers.
Advisory Board analysis indicates cancer cases are projected to increase 13% nationwide over the next decade, disproportionately affecting states with growing elderly populations. As demand for cancer care increases, health organizations face greater challenges than ever before. Staff shortages and financial instability , exacerbated during the COVID-19 pandemic, continue to strain our healthcare systems. Accordingly, new cancer facilities must be flexible, cost-effective, and innovative, with a laser focus on patient experience and high-quality care to make the most of capital investment.
With this objective in mind, I pursued a research project through SmithGroup’s Exploration Grant program. My investigation focused on the relationship between the cancer patient’s treatment journey and their preferences in infusion therapy environments, asking the core question: do space preferences change over the course of treatment?
To gain greater insight into the patient experience, I conducted a comprehensive review of the existing research and initiated a pilot program to survey patients undergoing infusion treatments in SmithGroup-designed cancer centers. The synthesis of existing research with my preliminary survey findings uncovered a nuanced perspective on infusion environments—one that has the potential to drive more informed programming strategies and more accommodative, economical, and flexible design solutions.
What the Existing Research Shows A literature review of cancer center environments and patient experiences reveals three major themes. These themes offer a framework for analyzing variables that influence patient preferences for healing environments beyond prescribed infusion therapy.
Patient-Caregiver Relationships. The patient-caregiver relationship is crucial for trust, communication, and support. Because infusion therapy can be mentally and physically taxing, caregivers play a vital role beyond clinical duties. Staff who show genuine interest in patients’ well-being and provide empathetic support uplift the patients’ experience. Newer patients benefit and learn from conversations with caregivers and fellow patients. Both the physical proximity of caregivers to patients and the visibility of the care station during treatment contribute to patient perceptions of safety and a more positive treatment experience.

Social Environment. Social interactions among patients are shown to positively impact their well-being and experience. Some studies indicate that connecting with fellow patients can be even more influential than the physical environment. However, infusion environments need to offer a balanced experience; privacy, confidential interactions, and rest are also important factors for patients.
Physical Environment. The treatment environment can significantly affect patient stress and anxiety. Patients spend many hours in these spaces. Creating a sense of home, through natural light, operable windows, and control over the environment, can positively contribute to the treatment experience. Comfort, security, privacy, and autonomy over their physical environment all support the patient’s healing journey.
Patient Survey I worked with a Michigan-based cancer center to develop and deploy the pilot patient survey, exploring the dynamic between the cancer patient’s treatment journey and preferences in treatment spaces. The anonymized survey was live for one month, empowering patients to provide valuable insight into the core research question, plus the patient-caregiver relationship, the social and physical environments, and other feedback related to their experience inside the facility.
Patient Treatment Space Preferences. To test the relationship between the treatment journey and space preference, patients were asked various questions, including their personality type, how long they have been visiting the facility, their baseline preference of treatment space, and whether that preference changed over time. Responses showed that patients identifying as extroverted tend to prefer semi-private treatment spaces. Although there was a varying range of treatment tenure among the respondents, their preference of treatment space did not change over time.
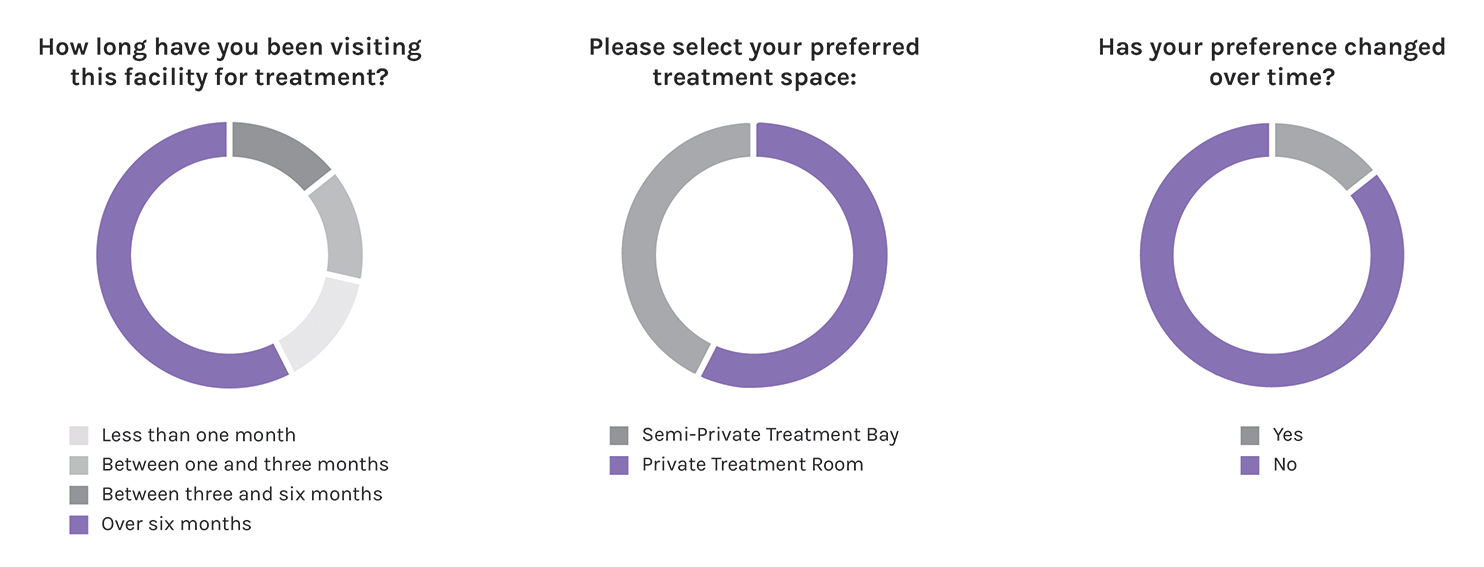
Patient Responses to Literature Review Themes. The survey asked about the patients’ experience, including communication with staff, opportunities for socialization, and the infusion room itself. Patient feedback shows that private communication with staff alleviated stress and contributed positively to their experience. Patients responded less positively to the social environment. Responses show that less than half of patients were able to make a social connection with their neighbors. Of the respondents who made a connection, only one-third found that it strongly enhanced the treatment process.
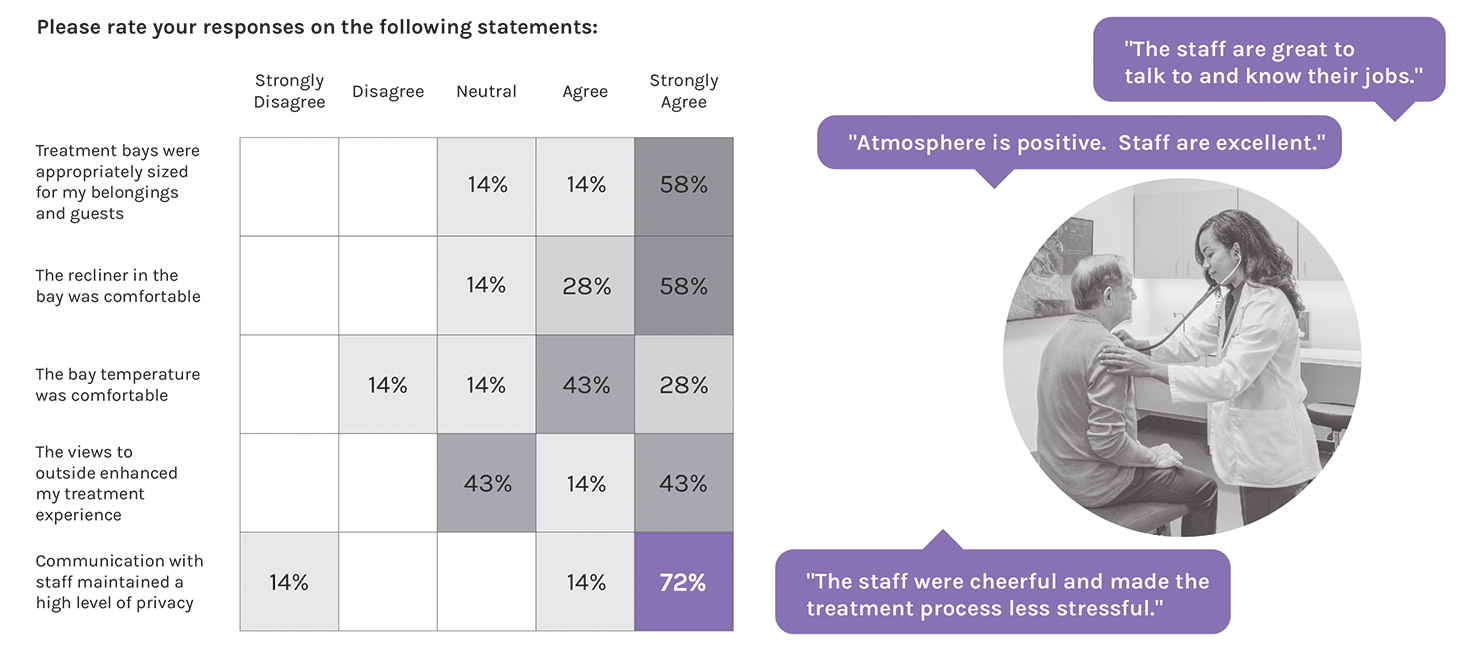
Finally, patients were asked to select what they liked most about their preferred treatment space: a private room or a semi-private treatment bay. Private room responses indicated that noise reduction, thermal comfort, and proximity to the care station are top priorities. Semi-private treatment bay responses identified privacy control, access to daylight and views, and opportunities for socialization as their top preferences.
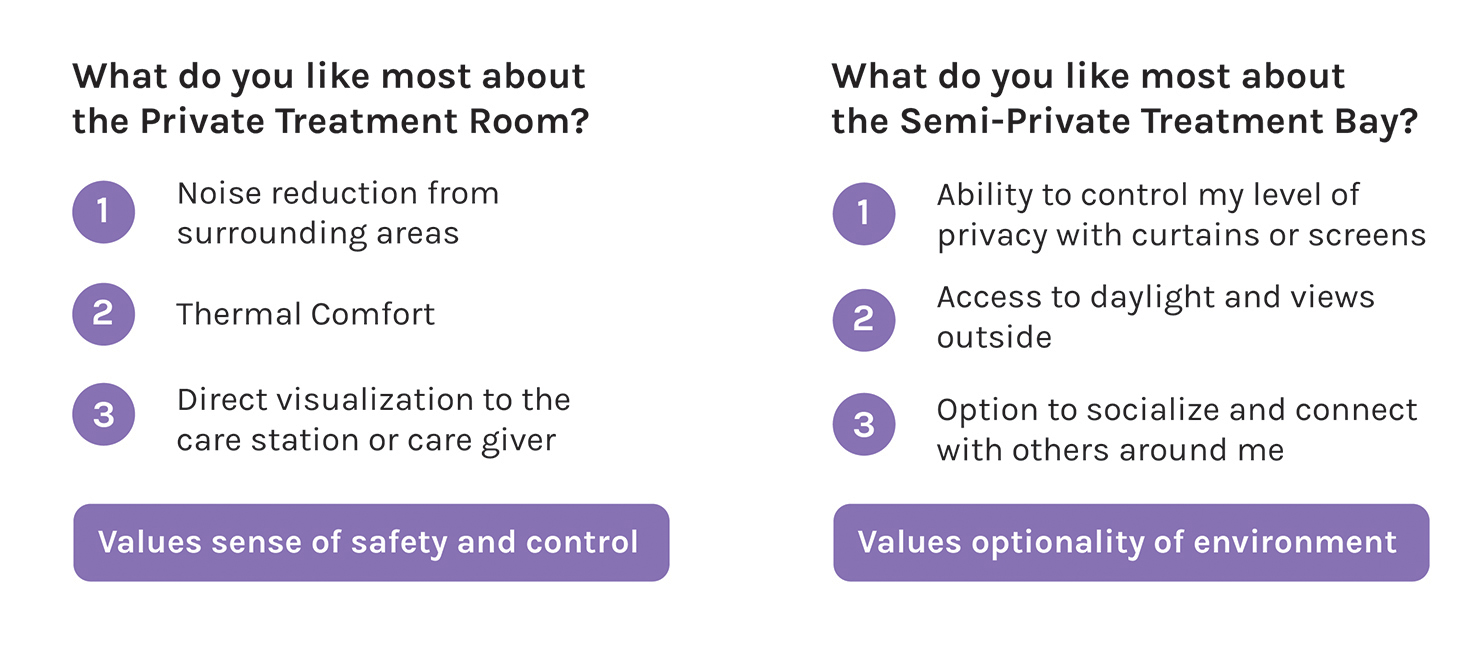
Analysis of Survey Findings Contrary to my initial hypothesis, patient preferences toward their therapy environment remained consistent throughout their treatment journey. This indicates that caregivers should empower patients to choose their preferred therapy space at the start of their treatment journey, and healthcare facilities should offer diverse options. Additional findings include:
- Physical adjacency and visual connection between the caregiver station and patient infusion play a vital role in providing a positive treatment experience.
- The patient-caregiver relationship has a significant impact on the patient’s overall satisfaction with the treatment process and can be supported by treatment space design.
- The patient-to-patient social dynamic was not as important as previous research indicated, potentially due to a multitude of factors, including the paradigm shift in how patients perceive their health and safety in a post-pandemic world.
- Treatment spaces that enable patient control over their own environment provide a more positive experience.

New Inquiries for Future Research Additional focus on the patient-to-patient social dynamic is warranted due to the wide discrepancy in results from my survey compared to the existing research conducted before 2020. This discrepancy may be due to multiple factors, including:
- The design, layout, and treatment room types available for patients in the test site.
- A shift in perception of safety and comfort in a post-pandemic era as immunocompromised patients are less likely to socialize with others.
- Advancements in mobile and smart device technology that provide more options for personal engagement and entertainment during treatment.
- Cultural and regional differences.
Gathering caregiver input on their experiences and perceptions of infusion spaces would help garner insight into patient preferences and add to our understanding of how those environments can better support staff. Nationwide nursing shortages pose significant challenges to the healthcare industry; designing spaces that can reduce burnout and positively impact workplace experience and satisfaction is imperative.
While it is not possible to draw generalizable conclusions from the pilot survey without further study, initial findings point toward the benefits of identifying a patient’s preferred type of therapy space at the start of their treatment journey. As more patient data is gathered, further analysis can establish new findings and insights to inform programming and design strategies.
In the meantime, it is critical that caregivers offer patients agency over the selection of their treatment space. The healthcare facility should support a variety of spaces that balance considerations for privacy, safety, connection, control, and comfort. The most successful treatment journeys for cancer patients, and the most promising design directions for cancer centers, will all begin by posing thoughtful questions emphasizing better patient understanding and empathy.
- Share via Facebook
- Share via Twitter
- Share via LinkedIn
- Share via Email

The Patient Journey: What it is and Why it Matters

- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
Healthcare is under enormous pressure today.
Patient expectations about their service and experience have changed over the years. Patients have more choices about their care, and they’re more empowered with information about what they want their care experience to be. They expect you to interact with them on their terms, not yours. And with COVID-19 turning so much of our lives digital, this trend has only accelerated.
Having a robust marketing automation approach is critical to addressing these challenges in today’s environment. Meeting — and exceeding — patient expectations comes down to managing your patient’s engagement journey.

How can patient journeys improve care?
What patient journeys can do is turn the healthcare experience from a primarily reactive experience to a proactive one.
By building out journeys for your patient personas, you can close gaps in care, establishing robust preventative routines that ultimately help your patients stay as healthy as possible for as long as possible.
Engaging consumers and patients where they are builds trust and confidence that keeps patients in the system and encourages them to refer their friends and family to your practice. According to the Beryl Institute , 70% of patients will share a positive experience with others. But your bigger risk is that 76% will share a negative one. And with a negative experience, 43% of patients won’t go back to that provider, with 37% finding a different doctor altogether.
What is the patient journey?
A patient journey represents the entire sequence of events that a patient experiences within a given healthcare system or across providers, from scheduling an appointment for a regular checkup to receiving treatment for an illness or injury.
A patient journey is an ongoing process that incorporates all parts of the healthcare ecosystem, from hospitals to physicians, specialty care, and outpatient therapy.
While it is easy to think about a patient’s journey as those interactions you have with them before, during, and after an appointment, there are actually many other touchpoints that drive their overall journey. A comprehensive patient engagement strategy touches on all aspects of a patient’s relationship with a healthcare provider, including:
- Onboarding and Access
- Diagnosis and Treatment
- Adherence to Lifestyle or Behavioral Changes
- Ongoing and Proactive Health (Wellness)
- Referrals and Loyalty
How do I create the patient engagement journey?
Every single interaction with a patient is part of the patient engagement journey and a moment of truth for the health system or provider to add value.
In today’s value-based healthcare world, having that personalized experience is more important than ever. A patient engagement journey organizes those communication touchpoints and ensures you’re delivering the right information at the right time to the right person, and leveraging the appropriate communication channel. Millennials and Generation Z, for example, may be more likely to prefer a text, email, or chat to a phone call.
It’s about knowing your patients’ preferences — like that they prefer to be texted during the day while they’re at work or if they prefer an office vs. telehealth visit — and what’s going to make it easier for them, like sending automatic reminders the week and day before an appointment.
Whether it’s making sure you follow up with cardiac patients about weighing themselves daily after surgery to catch any water retention issues or asking colonoscopy patients whether or not they’ve been following post surgery protocols after discharge, it’s about continuity of care once a patient leaves the office or hospital so they have a quality outcome. From there, patients can more proactively drive their own wellness plan.
Here are important areas to focus on when creating your patient engagement journey:
Establish your patient personas
You need to know the different types of patients that are coming into your organization. You want to figure out:
- What are the most relevant needs of your patients?
- What are their communication and care preferences?
- How do they want to engage with you?
- What information do you already know about them?
To be able to craft the best possible patient experience, you first have to know more about your patients.
For example, there’s a well-known healthcare persona out there called the “Medical Mom” (which can, of course, be any individual taking care of themselves, their kids, their spouses, and may also be the caretaker for aging parents).
Let’s say this individual has three children, and they book annual physicals at their pediatrician, which happens to have offices in the same building as their own primary care physician. Wouldn’t it be nice if the office sent them one email reminder to schedule all five appointments, rather than five different emails? And when they do call, scheduling those appointments back-to-back so everyone is in and out in one afternoon?
A spreadsheet is not going to be able to do that for you. Collecting and managing the data required to drive complex, interconnected patient journeys requires more than a spreadsheet. In order to succeed, you’ll need to pay close attention to the entire patient lifecycle.
Understand the entire patient lifecycle
An appointment reminder is a great start to engaging a patient, but it’s just one event in an ongoing patient lifecycle that begins with preventative care and includes diagnostics, delivery of care, and post-operations.
For example, how many patients show up for routine blood work at their physician office and you find out they haven’t fasted for the appropriate amount of time? Sending a patient home is frustrating for them and it’s frustrating for you. If the appointment is at 2:00 PM, then that appointment reminder should have been sent at dinnertime the previous evening, reminding them that they can’t eat anything after a 6:00 AM breakfast the next morning.
You’ll want to tailor your communications based on whether the patient is new or existing, what their preferences are, and whether they have any specific or chronic health issues. From there, you need to…
Understand the moments of truth
The healthcare system is complicated, even for those who have been a part of it for decades. The key to building a great foundation for your patient engagement strategy is to put yourself in a typical patient’s shoes. Most patients don’t engage with the healthcare industry unless they’re feeling sick. That means they’re rarely at their best, and they’re not only anxious about getting better, but about the costs associated with that.
The best healthcare providers understand the moments of truth — opportunities for a positive touchpoint that can alleviate their stress and anxiety and help them get on the road to recovery. Every time you interact with a patient is an opportunity for a moment of truth, whether that be in person or via other channels of communication. It’s not only about establishing accurate moments of truth, but capitalizing on them.
It’s up to you to understand the places people need to be, how you want to communicate to them, and make every one of those touchpoints a positive experience. It doesn’t matter whether they’re physically in your office or not. Your patient engagement journey is what guides your patients to making the best possible decisions on their care so they get better.
The easier you make it for them to engage with you, the higher quality their care will be. Ultimately, you want your patients to be evangelists for your services based on their positive experiences. To do that, you’ll need to…
Get the data you need
Your patients expect personalization.
Personalization in healthcare used to mean created tailored treatment plans and clinical protocols. That’s still important, but patients expect more personalization around the entire experience, from access to communication to quality outcomes. It’s like turning on a light switch in your home: a patient just expects the light to turn on.
Personalization today means being able to see at-a-glance a patient’s healthcare record, communication preferences, and social determinants that may be impacting their overall health to give you a 360-degree picture .
To do this, you need more than clinical data.
You may have patients that constantly miss their appointments. By storing questions that go beyond health risks — say, that they’re a smoker — but to understand that they don’t have a car to get to the appointment in the first place is becoming a more important part of the process. Part of empathetic, compassionate care is understanding these environmental factors that can help patients get the care they need, whether that’s calling a Senior Shuttle, caregiver, or arranging a telehealth appointment instead.
Once you have the data, you can…
Encourage referrals and loyalty
The first place people look for a new doctor isn’t the Internet. It’s their friends and family. In an ideal world, every patient you have should be able to say, “Oh, I loved my experience with…”
Doing that starts with the technology you have. Before a patient ever comes in for treatment, you need to make sure they have a seamless experience that builds trust and encourages referrals and loyalty.
How do I get started with patient journey mapping?
It’s time to move away from the mindset to simply fill the top of the funnel with as many new potential patients and contacts with caregivers as possible. While this is still a requirement, it is just as crucial for organizations to get better at managing and growing relationships at every phase of the patient journey. Providers must engage with consumers in the marketplace to introduce them to their services of course, but it is of growing importance that they offer support throughout the entire diagnostic and treatment process.
As a Salesforce Platinum Partner with deep industry expertise, we have created a Foundation for Patient Engagement package — a complete strategy that starts with Health Cloud and facilitates a 360-degree view of the patient , as well as a comprehensive communication strategy, CTI integration, and the use cases driving patient acquisition, engagement, and loyalty.
Learn more about building your patient journey with Silverline.
From the Blog More articles about Provider

Provider Personalization in Healthcare: 6 Keys To Successful Patient Experiences

Provider Prioritize Patient Experiences with EHR CRM Integration

Provider The Future of AI for Healthcare Providers
We don't support internet explorer.
Please use Chrome, Safari, Firefox, or Edge to view this site.
It seems you are using an outdated browser. Please upgrade to a modern browser to improve your experience on this website.
The Patient’s Journey Through the COPD Treatment
Study Enrollment completed Analysis and reporting in progress Funded by GSK
COPD Foundation Principal Investigator: Barbara Yawn, MD MSc Patient Investigator: Valerie Chang
The Patient Journey Study utilized the COPD Foundation's research infrastructure to:
- identify and recruit all of the study participants;
- facilitate an asynchronous focus group to identify issues in the patient’s COPD treatment journey utilizing a private feature on the COPD Foundation’s COPD360social online community ;
- develop and deploy a survey to the COPD Patient Powered Research Network ( COPD PPRN ), the Foundation’s self-reported registry of over 8000 individuals with COPD or at risk for COPD.
Why is the Patient’s Journey to Diagnosis and Treatment so Important?
COPD is one of the leading causes of disability and disease in the US, and yet a significant proportion of the population with evidence of COPD remain undiagnosed. I addition, even when patients are diagnosed with COPD, they face barriers in receiving the ideal treatment of their disease. This study was designed with the aim to gain a better understanding of the treatment and life journey of people with COPD.
This observational study recruited patients from the COPD PPRN to participate in an online focus group which took place from mid-July to late August 2021. Learnings from the focus group were used to design a survey which was available to members of the COPD PPRN from 2/8/2021 through 3/3/2021. The survey questions covered a range of topics including age and circumstances of diagnosis, current treatment including access to medication and education on how to use therapies.
Completed Activities within the Patient’s Journey Study:
- Pre-Screener: A pre-screener was made available on the COPD PPRN participant portal to assess the eligibility of interested individuals to participate in one of three online focus groups.
- Confirmation of Eligibility: A COPDF research coordinator conducted telephone calls to confirm eligibility for those identified as potentially eligible to take part in the online focus groups. On the calls, potential participants were provided information about the project and had the opportunity to ask questions and confirm their interest in participation.
- Focus Group 1: Identify issues in the patient’s treatment journey related to systemic steroid therapy for the treatment of COPD exacerbations
- Focus Group 2: Identify issues in the patient’s treatment journey related to the use of multiple maintenance inhalers or those on triple therapy (ICS, ICS/LABA, LAMA, LABA/LAMA, ICS/LABA/LAMA)
- Focus Group 3: Identify Issues in the patient’s treatment journey related to a worsening of disease, experienced as exacerbations and/or chronic increase in symptoms Many common topics were explored among the 3 focus groups, including identifying: the classes of maintenance medications used, inhaler devices chosen, patient reported reasons for changes in medications and devices and perceived impact of those changes. Additionally we asked questions specific to how often medication class or device changes are driven by such things as symptom burden, exacerbation occurrence and frequency, patient preference, insurance and formulary issues and device issues will be investigated. Along with various therapies and COPD treatments, it was important to explore how COVID-19 has impacted COPD treatment, including medications prior, during and as the pandemic transitions with special attention to use of inhaled corticosteroids, oral steroids and nebulizer devices as well as access to care during and after pandemic.
- Patient Journey Survey: Based on the analysis of responses from the 3 focus groups, a survey was developed and deployed to the COPD PPRN.
Results and Conclusions
The Patient Journey survey was completed by 669 COPD PPRN participants (mean age of 66) on the online platform, including 41% men and 59% women. Out of the respondents, 79% reported that their illness was called COPD at the time of diagnosis, although 33% reported that they had symptoms for over three years prior to their diagnosis, with another 37% reporting symptoms for 1-2 years. The most common symptoms reported at the time of diagnosis included shortness of breath while exercising or walking up steps, difficulty breathing, frequent coughing, and fatigue. While most patients (79%) reported that they have been shown how to use their inhalers, 46% also reported they have never been asked to demonstrate that they know how to use their devices. 53% of participants reported using nebulized medications, with the most common reason for their use being that "Medicine works better in nebulizer than puffers or inhalers". 65% of participants reported using oral steroids or steroid shots for their COPD, including 13% who stated that they used steroids "regularly, daily, or weekly for several weeks or months".
A large proportion of COPD patients in this survey had symptoms for years prior to their diagnosis. While most patients have been shown how to use their therapies, many have not been asked to demonstrate their ability, which may explain why patients feel nebulized therapies work better. Finally, the regular use of steroids in these patients occurs in a significant minority of patients.
This study reaffirms the value of the patient voice to help educate and further understand the patient journey through COPD diagnosis, treatment and barriers. Further analysis is being conducted to look at rural verses urban and/or primary care versus specialty for diagnosis. The patients provided a wealth of knowledge from their vast experience during the 3-day focus group which is difficult to amass from a survey.
To learn more about the study, contact [email protected] .
Join us on copd360social.
Join the Conversation
Already a Member?
This page was reviewed on October 7, 2021 by the COPD Foundation Content Review and Evaluation Committee .
Patient Experience Factors and Implications for Improvement Based on the Treatment Journey of Patients with Head and Neck Cancer
Affiliations.
- 1 Department of Service Design, Graduate School of Industrial Arts, Hongik University, Seoul 04066, Republic of Korea.
- 2 Department of Industry-Academic Cooperation Foundation, The Catholic University of Korea, Seoul 06591, Republic of Korea.
- 3 Department of Visual Communication Design, Graduate School of Design, Hongik University, Seoul 04066, Republic of Korea.
- 4 Department of Otorhinolaryngology-Head and Neck Surgery, Incheon St. Mary's Hospital, The Catholic University of Korea, Incheon 21431, Republic of Korea.
- PMID: 37190193
- PMCID: PMC10136947
- DOI: 10.3390/cancers15082265
Based on the treatment journey, this study aimed to present insights into improving the patient-centered service experience for head and neck cancer (HNC) patients. We interviewed and observed patients, caregivers, and doctors. We conducted a qualitative content analysis and service clue analysis to identify barriers and enablers to patient care and to derive insights into the patient experience (PE). We received feedback from doctors considering the priority, importance, and feasibility of improvements and classified the insights into three service experience aspects, to suggest improvement directions. As a result, the 'functional' aspect of service experience stressed the importance of a comprehensive guide to the treatment process, delivery of reliable information, use of easy-to-understand terms, repeated summary explanations, the establishment of close and flexible linkages between departments, and the provision of educational programs. Regarding the 'mechanic' aspect, the use of large and clear visuals for patients, to easily understand the care information provided by medical staff was distinguished. In the 'humanic' aspect, patients' psychological stability, trust in doctors, and doctor's encouragement and support through maintaining a positive attitude were prioritized. This qualitative study provided integrative insights into the HNC patient experience, through the application of service design methodologies, such as a patient journey map, participatory research methods, and service experience clues.
Keywords: aspects of service experience; barriers to patient experience; head and neck cancer; patient journey map; patient treatment journey; patient-centered care; user’s integrative perspectives.
Grants and funding
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Breast cancer patient experiences through a journey map: A qualitative study
Roles Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Clinical Psychology and Psychobiology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
Affiliation Medical Oncology Department Hospital Universitario Central of Asturias, Oviedo, Spain
Roles Resources, Validation, Writing – review & editing
Affiliation Social Psychology and Quantitative Psychology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Affiliation Medical Oncology Department, Hospital Universitario Clínico San Carlos, Madrid, Spain
Affiliation Medical Oncology Department, Complexo Hospitalario Universitario de Ourense, Ourense, Spain
Affiliation Medical Oncology Department, Hospital Universitario La Paz, Madrid, Spain
Affiliation Medical Oncology Department, Hospital General Universitario de Elche, Elche, Spain
Affiliation Medical Oncology Department, Hospital Universitario Fundación Alcorcón, Madrid, Spain
Roles Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing
- Laura Ciria-Suarez,
- Paula Jiménez-Fonseca,
- María Palacín-Lois,
- Mónica Antoñanzas-Basa,
- Ana Fernández-Montes,
- Aranzazu Manzano-Fernández,
- Beatriz Castelo,
- Elena Asensio-Martínez,
- Susana Hernando-Polo,
- Caterina Calderon

- Published: September 22, 2021
- https://doi.org/10.1371/journal.pone.0257680
- Reader Comments
Registered Report Protocol
21 Dec 2020: Ciria-Suarez L, Jiménez-Fonseca P, Palacín-Lois M, Antoñanzas-Basa M, Férnández-Montes A, et al. (2020) Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol. PLOS ONE 15(12): e0244355. https://doi.org/10.1371/journal.pone.0244355 View registered report protocol
Breast cancer is one of the most prevalent diseases in women. Prevention and treatments have lowered mortality; nevertheless, the impact of the diagnosis and treatment continue to impact all aspects of patients’ lives (physical, emotional, cognitive, social, and spiritual).
This study seeks to explore the experiences of the different stages women with breast cancer go through by means of a patient journey.
This is a qualitative study in which 21 women with breast cancer or survivors were interviewed. Participants were recruited at 9 large hospitals in Spain and intentional sampling methods were applied. Data were collected using a semi-structured interview that was elaborated with the help of medical oncologists, nurses, and psycho-oncologists. Data were processed by adopting a thematic analysis approach.
The diagnosis and treatment of breast cancer entails a radical change in patients’ day-to-day that linger in the mid-term. Seven stages have been defined that correspond to the different medical processes: diagnosis/unmasking stage, surgery/cleaning out, chemotherapy/loss of identity, radiotherapy/transition to normality, follow-up care/the “new” day-to-day, relapse/starting over, and metastatic/time-limited chronic breast cancer. The most relevant aspects of each are highlighted, as are the various cross-sectional aspects that manifest throughout the entire patient journey.
Conclusions
Comprehending patients’ experiences in depth facilitates the detection of situations of risk and helps to identify key moments when more precise information should be offered. Similarly, preparing the women for the process they must confront and for the sequelae of medical treatments would contribute to decreasing their uncertainty and concern, and to improving their quality-of-life.
Citation: Ciria-Suarez L, Jiménez-Fonseca P, Palacín-Lois M, Antoñanzas-Basa M, Fernández-Montes A, Manzano-Fernández A, et al. (2021) Breast cancer patient experiences through a journey map: A qualitative study. PLoS ONE 16(9): e0257680. https://doi.org/10.1371/journal.pone.0257680
Editor: Erin J. A. Bowles, Kaiser Permanente Washington, UNITED STATES
Received: February 17, 2021; Accepted: September 3, 2021; Published: September 22, 2021
Copyright: © 2021 Ciria-Suarez et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Relevant anonymized data excerpts from the transcripts are in the main body of the manuscript. They are supported by the supplementary documentation at 10.1371/journal.pone.0244355 .
Funding: This work was funded by the Spanish Society of Medical Oncology (SEOM) in 2018. The sponsor of this research has not participated in the design of research, in writing the report, or in the decision to submit the article for publication.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [ 1 ]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [ 2 ]. The 5-year survival rate is currently around 85% [ 3 , 4 ].
Though high, this survival rate is achieved at the expense of multiple treatment modalities, such as surgery, chemotherapy, radiotherapy, and hormone therapy, the side effects and sequelae of which can interfere with quality-of-life [ 5 ]. Added to this is the uncertainty surrounding prognosis; likewise, life or existential crises are not uncommon, requiring great effort to adjust and adapt [ 6 ]. This will not only affect the patient psychologically, but will also impact their ability to tolerate treatment and their socio-affective relations [ 7 ].
Several medical tests are performed (ultrasound, mammography, biopsy, CT, etc.) to determine tumor characteristics and extension, and establish prognosis [ 8 ]. Once diagnosed, numerous treatment options exist. Surgery is the treatment of choice for non-advanced breast cancer; chemotherapy, radiotherapy, and hormone therapy are adjuvant treatments with consolidated benefit in diminishing the risk of relapse and improving long-term survival [ 9 ]. Breast cancer treatments prompt changes in a person’s physical appearance, sexuality, and fertility that interfere with their identity, attractiveness, self-esteem, social relationships, and sexual functioning [ 10 ]. Patients also report more fatigue and sleep disturbances [ 11 ]. Treatment side effects, together with prognostic uncertainty cause the woman to suffer negative experiences, such as stress in significant relationships, and emotions, like anxiety, sadness, guilt, and/or fear of death with negative consequences on breast cancer patients’ quality-of-life [ 10 , 12 ]. Once treatment is completed, patients need time to recover their activity, as they report decreased bodily and mental function [ 13 ], fear of relapse [ 14 ], and changes in employment status [ 15 ]. After a time, there is a risk of recurrence influenced by prognostic factors, such as nodal involvement, size, histological grade, hormone receptor status, and treatment of the primary tumor [ 16 ]. Thirty percent (30%) of patients with early breast cancer eventually go on to develop metastases [ 17 ]. There is currently no curative treatment for patients with metastatic breast cancer; consequently, the main objectives are to prolong survival, enhance or maintain quality-of-life, and control symptoms [ 17 , 18 ]. In metastatic stages, women and their families are not only living with uncertainty about the future, the threat of death, and burden of treatment, but also dealing with the existential, social, emotional, and psychological difficulties their situation entails [ 18 , 19 ].
Supporting and accompanying breast cancer patients throughout this process requires a deep understanding of their experiences. To describe the patient’s experiences, including thoughts, emotions, feelings, worries, and concerns, the phrase “patient voice” has been used, which is becoming increasingly common in healthcare [ 20 ]. Insight into this “voice” allows us to delve deeper into the physical, emotional, cognitive, social, and spiritual effects of the patient’s life. This narrative can be portrayed as a “cancer journey", an experiential map of patients’ passage through the different stages of the disease [ 21 ] that captures the path from prevention to early diagnosis, acute care, remission, rehabilitation, possible recurrence, and terminal stages when the disease is incurable and progresses [ 22 ]. The term ‘patient journey’ has been used extensively in the literature [ 23 – 25 ] and is often synonymous with ‘patient pathway’ [ 26 ]. Richter et al. [ 26 ] state that there is no common definition, albeit in some instances the ‘patient journey’ comprises the core concept of the care pathway with greater focus on the individual and their perspective (needs and preferences) and including mechanisms of engagement and empowerment.
While the patient’s role in the course of the disease and in medical decision making is gaining interest, little research has focused on patient experiences [ 27 , 28 ]. Patient-centered care is an essential component of quality care that seeks to improve responsiveness to patients’ needs, values, and predilections and to enhance psychosocial outcomes, such as anxiety, depression, unmet support needs, and quality of life [ 29 ]. Qualitative studies are becoming more and more germane to grasp specific aspects of breast cancer, such as communication [ 27 , 30 ], body image and sexuality [ 31 , 32 ], motherhood [ 33 ], social support [ 34 ], survivors’ reintegration into daily life [ 13 , 15 ], or care for women with incurable, progressive cancer [ 17 ]. Nevertheless, few published studies address the experience of women with breast cancer from diagnosis to follow-up. These include a clinical pathway approach in the United Kingdom in the early 21st century [ 35 ], a breast cancer patient journey in Singapore [ 25 ], a netnography of breast cancer patients in a French specialized forum [ 28 ], a meta-synthesis of Australian women living with breast cancer [ 36 ], and a systematic review blending qualitative studies of the narratives of breast cancer patients from 30 countries [ 37 ]. Sanson-Fisher et al. [ 29 ] concluded that previously published studies had examined limited segments of patients’ experiences of cancer care and emphasized the importance of focusing more on their experiences across multiple components and throughout the continuum of care. Therefore, the aim of this study is to depict the experiences of Spanish breast cancer patients in their journey through all stages of the disease. To the best of our knowledge, there are no studies that examine the experience of women with breast cancer in Spain from diagnosis through treatment to follow-up of survivors and those who suffer a relapse or incurable disease presented as a journey map.
A map of the breast cancer patient’s journey will enable healthcare professionals to learn first-hand about their patients’ personal experiences and needs at each stage of the disease, improve communication and doctor-patient rapport, thereby creating a better, more person-centered environment. Importantly, understanding the transitional phases and having a holistic perspective will allow for a more holistic view of the person. Furthermore, information about the journey can aid in shifting the focus of health care toward those activities most valued by the patient [ 38 ]. This is a valuable and efficient contribution to the relationship between the system, medical team, and patients, as well as to providing resources dedicated to the patient’s needs at any given time, thus improving their quality of life and involving them in all decisions.
Study design and data collection
We conducted a qualitative study to explore the pathway of standard care for women with breast cancer and to develop a schematic map of their journey based on their experiences. A detailed description of the methodology is reported in the published protocol “Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol” [ 39 ].
An interview guide was created based on breast cancer literature and adapted with the collaboration of two medical oncologists, three nurses (an oncology nurse from the day hospital, a case manager nurse who liaises with the different services and is the ‘named’ point of contact for breast cancer patients for their journey throughout their treatment, and a nurse in charge of explaining postoperative care and treatment), and two psycho-oncologists. The interview covered four main areas. First, sociodemographic and medical information. Second, daily activities, family, and support network. Third, participants were asked about their overall perception of breast cancer and their coping mechanisms. Finally, physical, emotional, cognitive, spiritual, and medical aspects related to diagnosis, treatment, and side effects were probed. Additionally, patients were encouraged to express their thoughts should they want to expand on the subject.
The study was carried out at nine large hospitals located in six geographical areas of Spain. To evaluate the interview process, a pilot test was performed. Interviews were conducted using the interview guide by the principal investigator who had previous experience in qualitative research. Due to the Covid-19 pandemic, all interviews were completed online and video recorded with the consent of the study participants for subsequent transcription. Relevant notes were taken during the interview to document key issues and observations.
Participant selection and recruitment
Inclusion criteria were being female, over 18 years of age, having a diagnosis of histologically-confirmed adenocarcinoma of the breast, and good mental status. To ascertain the reality of women with breast cancer, most of the patients recruited (80%) had been diagnosed in the past 5 years. Patients (20%) were added who had been diagnosed more than 5 years earlier, with the aim of improving the perspective and ascertaining their experience after 5 years.
Medical oncologists and nurses working at the centers helped identify patients who met the inclusion criteria. Participants went to the sites for follow-up between December 2019 and January 2021. Eligible women were informed of the study and invited to participate during an in-person visit by these healthcare professionals. Those who showed interest gave permission to share their contact information (e-mail or telephone number) with the principal investigator, who was the person who conducted all interviews. The principal investigator contacted these women, giving them a more detailed explanation of the study and clarifying any doubts they may have. If the woman agreed to participate, an appointment was made for a videoconference.
A total of 21 women agreed to participate voluntarily in this research. With the objective of accessing several experiences and bolstering the transferability of the findings, selection was controlled with respect to subjects’ stage of cancer, guaranteeing that there would be a proportional number of women with cancer in all stages, as well as with relapses.
Data analysis
The data underwent qualitative content analysis. To assure trustworthiness, analyses were based on the system put forth by Graneheim, and Lundman [ 40 ]. Interviews were transcribed and divided into different content areas; units of meaning were obtained and introduced into each content area; meaning codes were extracted and added; codes were categorized in terms of differences and similarities, and themes were created to link underlying meanings in the categories. All members of the research team (core team, two medical oncologists, three nurses and two psycho-oncologists) reviewed the data and triangulated the outcomes between two sources of data: qualitative data from the interview and non-modifiable information, such as sociodemographic (i.e., age, marital status, having children) and clinical (i.e., cancer stage and surgery type) data. Following this process, we reached saturation of the interview data by the time we had completed 21 interviews.
Ethical considerations
This study was performed in accordance with the ethical standards of the Declaration of Helsinki, and its subsequent amendments. The study was approved by the Research Ethics Committee of University of Barcelona (Institutional Review Board: IRB00003099) and supported by the Bioethics Group of the Spanish Society of Medical Oncology (SEOM) 2018 grant. All participants received a written informed consent form that they signed prior to commencing with the interviews and after receiving information about the study.
Patient baseline characteristics
In total, 21 women with a mean age of 47 years (range, 34 to 61) were interviewed. Most of the study population was married (66.7%), had a college education (66.7%), and had 2 or more children (42.9%). All cancer stages were represented, up to 23.8% tumor recurrence, and most of the primary cancers had been resected (95.2%) (see Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0257680.t001
Description of the breast cancer patient journey
The women diagnosed with breast cancer describe the journey as a process tremendously affected by the different medical stages. Each stage has its own characteristics that condition the experiences, unleashing specific physical, emotional, cognitive, and social processes. Additionally, the patients perceive this entire process as pre-established journey they must undertake to save their life, with its protocols based on the type and stage of cancer.
“ People said to me , ‘What do you think ? ’ and I answered that there was nothing for me to think about because everything is done , I have to go on the journey and follow it and wait to see how it goes” (Patient 6)
Fig 1 displays the various phases of the journey that patients with breast cancer go through; nevertheless, each woman will go through some or others, depending on their type of cancer.
https://doi.org/10.1371/journal.pone.0257680.g001
Throughout the entire patient journey.
Processes of loss and reinterpretation of the new circumstance . What stands out the most in the process these women go through during the diagnosis and treatment of breast cancer is loss; specifically, the loss of health and a reinterpretation of the new circumstance and the new bodily reality. In the most extreme cases, the loss of health emerges with the fear of death that many women report at the time of diagnosis or during treatment, due to the distress generated. The loss of identity seems to be related to the evolutionary (existential) moment in which the woman is; there are patients who report feelings of disability or loss of attractiveness, or fear of not being able to get pregnant in the future, especially the youngest.
I felt a terrifying fear and thought , “You have cancer you tell yourself , you’re going to die tomorrow .” (Patient 6) I feel like after the hysterectomy , as a woman , I no longer have anything , only the physical . Sure , I look great , but I tell myself that it’s just a shell , the shell I inhabit , because as a woman , I only have one breast left . (Patient 6) At that moment , I had to make the decision that I was no longer going to be a mother . (Patient 14)
Personal change . Most of the women report that with the diagnosis of breast cancer, their life stands still and from that point forward, a different journey begins. The sole focus on this journey is the disease and its implications. During all those months, the patients stop working; they focus on their medical treatments, and reflect a lot on their current situation and on life. Most of the participants state, especially those who have already been discharged, that they know themselves better now; they take better care of themselves, and they enjoy their day-to-day and the small moments more, making the most of their time, with more initiatives and fewer trivial complaints.
Clearly , you’re not the same person you were before; I don’t think she’ll ever come back; your mindset changes completely and I have sequelae from all the treatments . (Patient 1) I re-think wasting energy on lost causes; what’s more , I’ve also learnt to say no . If I’m not in the mood to go somewhere , I just say no . (Patient 7) I take much more advantage of the present now , because you realize that things can change on any given day . (Patient 3)
Trust and appreciation for their physician . Most of the interviewees stated that they fully trusted the doctors who care for them, without question or objection to the treatments proposed. They reported that, as they go forward, they discuss the tests and treatments that are going to be performed, as well as possible side effects. Several stated that they are unaware of the stage of their cancer; similarly, most also do not know the benefits expressed in X% of the treatments. A few of the participants claimed that they did talk in detail about the different types of treatments with their oncologists, that they had sought another opinion, and one of them even reported having decided to stop chemotherapy, which was very hard for her, given her physician’s insistence that she continue.
The truth is that the oncologist didn’t say much about percentages; what she told me were the steps that I had to take; I thoroughly trusted her and she gave me a lot of peace of mind . (Patient 5) I told him , “I’m going to do whatever you tell me to . ” It never occurred to me to dispute whatever the oncologist might tell me . I was willing to do whatever was needed . (Patient 8)
Most of the women, at some point during the interview, state that they are grateful for the care they received and that, within the seriousness of their situation, there is a treatment for their condition.
I am super grateful for the treatment I’ve received and with the doctors assigned to me . (Patient 2) I’m very lucky; I’m only on my second line of treatment for metastasis and I’ve got a lot more ahead of me , but I consider myself lucky and I believe things are going very well . (Patient 20)
Role of the woman . We can see that the women adopt a role of care-givers and managers of their surroundings. They worry about the disease negatively affecting the people around them, which is why they make an effort to manage the family’s activity for when they can’t do it and they try to avoid being a physical burden or cause emotional distress to the people around them.
I was very strong ; I made everything easy for people , but making it very easy , doesn’t mean that it was easy for me , but that I made it easy for everyone . (Patient 8) I didn’t want to worry anyone because that’s just the way I am , I push forward and that’s that . (Patient 5)
Support network . In all cases, the family appears to be one of the elements that is most involved in the disease process. Within the family, the partner deserves special mention. The testimonies in this regard reveal a wide spectrum of possibilities that range from the feeling of having had great support to a lack of attention and understanding that, in many situations, causes the relationship to be strained or to end. Friends tend to appear more occasionally.
I can’t complain about my husband; he was up to the challenge , very attentive toward me and he fully understood how I was feeling ; I felt very supported . (Patient 14) We’ve had a period of a lot of arguing; I’ve had to sit down with him and tell him that life had changed for me . (Patient 18) I had a partner I had lived with for five and a half years and he told me , literally , that he looked at me like a little sister , no longer as a woman , and he left me , and that hurt me tremendously . (Patient 6)
On the other hand, many patients commented on the importance of social media, where they have met people in the same situation as them. They report feeling understood and in good company; likewise, they commented on the importance of being able to share their doubts and get to know about other experiences.
It’s a situation that only someone who has gone through can understand; you can have all the good intentions in the world , but if you haven’t gone through it , you can’t even begin to understand . (Patient 8)
Use of complementary treatments . Most patients follow conventional medical treatment. However, many resort to other disciplines that help them improve their quality-of-life, like dietary changes, getting more exercise than usual, visits to a psychologist or physical therapist, or using other integrative therapies, such as acupuncture, yoga, reiki, flowers of Bach, homeopathy, cannabis, or meditation.
I started to read a whole bunch of books to see what I could do to take care of myself in terms of nutrition and exercise ; you consider everything you can do . (Patient 5)
Diagnosis/unmasking.
This phase encompasses the time from when the woman detects some symptom or goes to a check-up until the medical diagnosis is made. For the woman, this is a time of a series of tests and results. We have observed that the procedures, especially the healthcare professionals that deal with the patients, and the timing vary, depending on the medical center where they are being cared for. Emotionally, this is one of the most complicated stages.
Emotional whirlwind . The wait to obtain test results has a huge emotional impact for the women, given that it is a time of great uncertainty and fear.
An entire month with all the anguish of finding out if you have something . (Patient 3) The worst part is waiting 15 days to find out the magnitude of the tragedy , if it’s throughout your entire body or only in your breast; you go through a brutal emotional whirlwind; the wait is horrible because there’s nothing else you can do , so that anguish that you carry inside is dreadful; it was hell for me . (Patient 10)
Additionally, the interviewees described many other emotions that included fear of death, fear of having no time, feeling of unreality, rage, anger, sadness, avoidance, denial…
The first thing I thought was that I was going to die and that I wouldn’t finish watching my children [grow up]; my father had died of lung cancer 25 years ago . (Patient 9) My only aim was to get back to normal , as if there were nothing wrong . (Patient 4) You have a lot of conflicting feelings; you wish this weren’t happening; you want to run away , but you say , “Where am I going to run to ? ” . (Patient 14)
Impact of medical communication . Several women comment that, when given the diagnosis, they dissociate because of the emotional impact and that they don’t listen to all the information that the medical professional is giving them.
I remember that she talked and talked , but I didn’t know what she was saying until she said , “Isabel , you’re going to be cured , okay ?”. (Patient 9)
During the diagnostic testing, the women are highly sensitive to the healthcare professionals’ words and gestures.
I looked at the face of the person who was doing the mammogram and that’s when I started to imagine the worst . (Patient 20) I say to them , “ But , is there a solution to this ? ” , and they say to me , “Don’t worry , I’m sure there is a solution . ” That “sure” is etched in my mind . (Patient 10)
Communication and managing their surroundings . After the diagnosis, the patients feel that they have to tell the people around them about their situation, especially those closest to them, the family. They all agree on how hard it is to share. Normally, the people it’s hardest to tell are their mother and their children. When they do, they try to put the most positive spin on it possible, in an attempt to keep them from worrying.
You no longer think only about yourself , you think , “Good grief , now I’ve got to tell my mother .” It’s hard . (Patient 16) I wanted to tell my kids the way I say things , always trying to look for the upside , and positive , although it was hard , but , anyway , in the end , it went well . When I finished , my husband told me , “You’ve convinced me that it’s no big deal .” (Patient 9) I told my son , “Son , don’t cry , your mom’s going to get over this , this is nothing .” (Patient 1)
During this period, the women contemplate how their situation will affect their surroundings and they try to organize it as much as possible.
I devoted myself to planning everything , to organizing what to do with my daughter , and to thinking about work , too , how I had left things at work . (Patient 4)
Surgery/cleaning out the cancer.
Uncertainty and fear . The participants express that before going into surgery, they are told about the kind of procedure that will be done, but that, depending on what they find and the analysis, it may change. In light of this, they exhibit an enormous feeling of uncertainty and fear. In addition, many voice concern about how the surgery will go.
They tell you conservative surgery , but if we open up and see something we didn’t see on the tests , then everything could change . (Patient 10) Aside from the anesthesia , that I’m terrified of , you spend several hours in surgery and you don’t really know how things will go; when they clean it out , they analyze it , and you go into the operating room and you don’t know what can happen . (Patient 9)
Feeling of loss . Considering that the breast is associated with an intimate, feminine part [of their body], many women experience the operation as a loss. This loss is more acute if the operation is a mastectomy and there is no reconstruction at the same time. The loss also involves a loss of identity, compounded by the side effects of chemotherapy, such as hair loss. The interviewees who had undergone mastectomy say that following surgery, when the bandaging is removed and the scar is revealed, is one of the most critical moments, which is why they express difficulty in managing it and appreciate the caring assistance from the professionals.
It is identification with yourself , you know , it’s what you’ve seen in the mirror , what you think you’re like and , suddenly , you’re no longer like that; there’s an incredible personal crisis because you no longer recognize what you’re seeing . (Patient 11) I closed my eyes and I removed the bandaging and I didn’t dare look … with my eyes , I imagined the worst . (Patient 12)
Acceptance or demand for more aggressive intervention . The patients perceive the surgery as essential to recovering their health, which is why the process is widely accepted. Some patients who demand a more invasive intervention, normally a bilateral mastectomy, do so because that way, they feel safer with respect to a possible relapse, as well as more comfortable esthetically.
If they have to remove my breast , let them take it; what I want is to get better . (Patient 16) They say that I am in full remission , so they only removed the lump , but at first , I said that I wanted my whole [breast] removed ; then they assessed how to do it . (Patient 13) They told me that I had a genetic mutation and more possibilities of developing breast cancer and , since I felt such rejection toward my remaining breast , I decided to get rid of that one , too . (Patient 20)
Chemotherapy/loss of identity.
The chemotherapy phase is one of the phases that affects the women’s lives the most, because of its physical impact and how long it lasts. No differences have been found in how they experience chemotherapy depending on whether it was neoadjuvant or adjuvant.
Negative impact of side effects . Chemotherapy is associated with many side effects that vary from one woman to another. Many indicate that they have suffered physical discomfort, such as fatigue, dysgeusia, pain, nausea and vomiting, mucositis, diarrhea, etc.
One day when I didn’t want to go to bed , I went to bed crying because I had the feeling that I wasn’t going to wake up . That day it was because I felt awful . (Patient 1)
Furthermore, all of the women suffer hair loss, which is one of the most-feared effects. Likewise, their body hair also falls out, especially on their face, and their weight fluctuates. All of these changes lead to a loss of identity that is experienced as taking away from their femininity. It must be remembered that oftentimes, chemotherapy is administered after surgery, further exacerbating this physical change. On top of all that, several women comment having to decide at the beginning of treatment whether to freeze their eggs or not; at that moment, many of them forfeit the possibility of becoming a mother or of becoming a mother again, which also adds to this loss of femininity.
Losing my hair was hard , but when it grew out again , I had an identity crisis . I didn’t recognize myself; people said I was really pretty like that , with my hair so short . I looked at myself in the mirror and I said that I’m not that woman , I can see that that woman is pretty , but it’s just that I don’t recognize myself . That’s not me or , it was like , I looked at myself and I didn’t recognize myself . That’s when I suffered a serious identity crisis , psychologically serious , but also serious because I sobbed because I looked at myself , but it wasn’t me . (Patient 6) Where’s that sexy lady , where is she ?, because you don’t feel good . I didn’t like myself at all . I was several sizes larger and I looked at myself and said , “What a monster . ” I didn’t feel good about myself . (Patient 1)
Many patients say that chemotherapy decreases their libido and dries up their mucous membranes, which is why they prefer not to have sex. For those who live as a couple, this situation can strain the relationship.
Sexually , I just didn’t feel like it , I wasn’t in the mood; not only did I not feel like it , my mucous membranes were dry and , what’s smore , I just couldn’t , I couldn’t , I felt bad for my husband , but he said , “Don’t worry .” (Patient 16)
Finally, some interviewees expressed a feeling of being poisoned by the treatment. These women tend to be highly focused on taking care of their body and have a very natural attitude toward life.
I had to really work my awareness that I was poisoning myself; at night I was at home and I thought that all that red liquid was circulating through my veins … I think I even had nightmares . (Patient 4)
Balance between caring for oneself and caring for others . The patients feel that it is time to take care of themselves, so they prioritize resting when they need it. Moreover, they worry about getting a haircut and, most of the times, they look for turbans and wigs. Some also learn how to put on make-up, which they rate as being very positive. On the other hand, those who have children or another person in their care, try to take care of them as much as they are able.
Around 11 : 00 , I no longer felt good , so I’d go to the armchair to rest and it’s like I had an angel , because I’d wake up a minute before I had to set the table and get lunch for my son who would be coming home from school . (Patient 1) While I was getting chemo , I went with the gadget and I told myself , “I’m going to teach you to apply make-up; for instance , your eyelashes are going to fall out . Make a line like this ” and at that moment when you look in the mirror , and we look like Fester in the Addams family . (Patient 13)
Vulnerability . The women experience great uncertainty and feelings of vulnerability the first times they receive chemotherapy, since they don’t know what side effects they will suffer.
With chemo , I started with a lot of fear and , later on , I became familiar with it little by little until the time comes when you go to the hospital like someone who’s going to pick up a bit of paper . (Patient 9)
In addition, those participants who join a social network or who are more closely tied to the hospital setting, know about the relapses and deaths of people around them diagnosed with breast cancer, which makes them feel highly vulnerable.
There are some people who leave the group because … it’s not like there are a lot of relapses and , geez , I think that it messes with your head . (Patient 13) We were almost always the same people at chemotherapy ; there was one guy who was really yellow who looked terrible and , there was one time when we stopped seeing him and another lady asked and the nurse said that he had died . (Patient 15)
At the same time, given the physical changes, especially those that have to do with body hair, many women feel observed when they leave home.
If I have to go out and take off my scarf because I’m hot or go straight out without any scarf on my head and whoever wants to look… let them ; I think that it’s up to us , the patients , to normalize the situation; unfortunately , there are more and more cases . (Patient 9)
Telling the kids . Since when the chemotherapy stage is going to entail many physical changes, the women look for ways to talk to their children about the treatment. Most of them comment that it is a complicated situation and all of them try to talk to their children in such a way as to protect them as much as possible.
I asked the nurse for help before I started chemotherapy to see if she had any pointers about how to talk about this with the kids and she recommended a story , but when I saw it , I didn’t like it … so , in the end , I decided to do it off the cuff . (Patient 10)
Radiotherapy/transition to normality.
The “last” treatment . When the patient reaches radiotherapy, normally, they have already spent several months undergoing physically aggressive medical procedures, which is why they feel exhausted. There is a physical exhaustion resulting from the previous treatments and made worse by the radiation therapy. Furthermore, many women also report feeling emotionally drained by the entire process. However, this is generally accompanied by joy and relief because they feel that they are in the final stage of treatment.
Emotionally , it’s a marathon that has to end up at some point . (Patient 10) For me , radiotherapy was like a lull in the battle , with a winning mind-set . (Patient 4)
Comparison with chemotherapy . There is a widespread perception that radiotherapy has fewer side effects than chemotherapy, although later, when they receive it, several patients suffer discomfort, above all fatigue and dizziness. Several report that at this point, they are mentally worn out and just want to be done with the process, which is why they have less information than about chemotherapy.
I feel like radiotherapy is unknown , that you think it’s more “light ” and it turns out not to be so light . (Patient 13)
Follow-up care/the “new” day-to-day.
Difficulty in getting back to normal . Once the patients are discharged, many feel that they need some time to recover, that it will be slow, in order to restore a more normalized pace of life. They are still working on their emotional and personal process.
When they tell you that you have cancer , they make it very clear : you have a goal; you have some months of chemo , some months of radio , and when you finish , you say , “And now , what do I do ?”. I say that because now I have to get back to my normal life , but I don’t feel normal . I still don’t feel cured , I’m not 100% . And you’re glad you’ve that you’ve finished it all and you’re alive , but at the same time , you say , “Gosh… this is very odd . ” It was a very strange feeling . (Patient 8)
Most patients report that their quality-of-life has diminished, due to the sequelae from the treatments. Lymphedema is one of the sequelae they name most often, although they also mention other symptoms, like digestive upset, weight issues, eye problems, scar pain, etc. The women who are on hormone therapy also suffer side effects, such as joint and muscle pain.
I have lymphedema and , although I have good mobility , I’m a little bit weak; when I go out for dinner , I generally order fish , because I can’t always cut meat well . (Patient 6)
Several interviewees also express difficulty in their affective-sexual relations. Many of them feel insecure because of all the physical changes; others have sequelae that hinder their relations, and still others are suffering symptoms of early menopause. This can cause problems in the couple and for those who don’t have a partner, suffer many complications when it comes to meeting other people.
I haven’t had sex with my husband for 2 years because , it’s also really complicated to get over; I’ve gone for pelvic physical therapy; I’ve used gels , but nothing works . (Patient 8) It’s taken me many months for me to have a relationship again; it’s been really hard because , even though everyone told me that I looked fine , I didn’t feel fine . My breast cancer had taken away all my attributes as a woman . (Patient 6)
Some women also experience difficulties when it comes to returning to work. Several state that they had been fired when they went back. They also report that when interviewing for a job, it’s complicated for them because they have to explain what happened and they mention the schedule of doctor’s visits that they have. Other women comment that they’ve been given early retirement or disability.
You go to the interview and if you tell them that you’ve had the disease , they look at you like you’re a weirdo . (Patient 13)
Breast reconstruction . How reconstruction is experienced, as well as its timing, are highly contingent upon they type of reconstruction. Each one has its pros and cons, but the opinions collected with respect to the type of reconstruction have been positive.
Although it took 18 months for the entire process to be over , I’m delighted with reconstruction with the expander . (Patient 16)
Some patients state that after the whole process, which has been long and complicated, they prefer not to undergo reconstruction immediately. In these cases, they report having felt a subtle pressure from the outside to undergo reconstruction.
Every time I went for my check-ups , they said , “You’re the only one left [who hasn’t undergone reconstruction]” and in the end , the truth is that I’m really happy because I think I look pretty . (Patient 12)
Check-ups and fear of relapse . Check-ups are one of the times that generate most worry and insecurity. The women remark that, starting a few days before and until they receive the results of the follow-up studies, they are more anxious about the possibility of relapse.
At every check-up my legs start shaking again and my stomach is in knots, although at my last one, everything turned out okay and I’m thrilled. (Patient 6) During the first stage , I did everything I had to do and I got over it , but it’s a lottery . You can do whatever you want , but it’s the luck of the draw and when you start going for check-ups , it’s like going to play Russian roulette . (Patient 8)
Maintenance hormone therapy . Hormone therapy is understood differently depending on age and on the major decision of whether or not to be a mother or to have another child. If the woman does not want to have more children, the treatment is accepted better. The patients who take it also report effects derived from menopause, for instance, joint pain or dry mucous membranes.
I did notice joint pain , but since I exercised , [I felt it] much less than my fellow women , although , for instance , when it comes to getting up from a chair , you get up like an old lady . (Patient 10)
Position of support . Several patients mention that, after discharge, they stay active on social media, they volunteer when they find out about someone or to participate in activities related to breast cancer, with the aim of being able to help other people who are in this situation.
It’s really good to meet other people who are going through the same thing , so , now that I’ve finished , I like it and I always help whenever I can , because I can share what was good for me . (Patient 13)
Relapse/starting over.
Emotional impact . The diagnosis of a relapse is experienced much the same as the initial diagnosis. All of the women report fear, although they also state that they are more familiar with the processes. Other emotions emerge, such as why me, blame, disbelief, etc.
Since they had told me that it wasn’t going to happen again , I believed it , of course , I wanted to believe it and it totally surprised me; I couldn’t stop crying and crying . (Patient 17)
Telling the family again . Patients repeat that telling the family about it again, especially the children and parents, is tough and they try to minimize it in an attempt to protect them emotionally.
On the very same day that I had my mammogram , my mother says that she wants to come a see the kids . We’re in the park , when she arrives , I have to tell her that everything’s fine and when we get home , I tell her everything . My mother’s devastated again and I tell her not to worry , that everything is going to be fine . (Patient 16)
Thinking about whether something could have been done differently . Several women comment that, after their relapse, they think about whether the treatment was enough or there must have been something they could have done to avoid the relapse.
You get furious , because you say , “I wasn’t supposed to get sick , because if , 2 years ago when the first microcalcifications appeared I had had them removed , then I wouldn’t have metastasis , or maybe I would . (Patient 19)
Metastatic breast cancer/time-limited chronic.
Re-interpreting the concept of metastasis . Most of the participants in this stage state that they have had to give new meaning to the word, “metastasis,” since their first perception was directly related to death. In this way, they come to understand that cancer can become chronic, although they now have to take medication and go to the hospital on a regular basis. Nevertheless, they know that their life expectancy may be a few years. The women who are involved in a group point out how hard it is to see their fellow member pass away.
What I now call my “ new normal” consists of lots of visits to the hospital and never going back to work . (Patient18)
They also state that at this stage, they do not identify with the disease generally known socially as “breast cancer”, where there is great emphasis placed on early detection and on their chances of being cured. This causes them to feel more isolated.
These pink ribbon campaigns hurt us because they tend to underscore that everything is going to turn out fine because breast cancer has a very high cure rate; there is huge lack of awareness . (Patient 20)
Physical and emotional discomfort . Most of the women in this stage report side effects from the treatments, although some comment that good quality-of-life can be preserved. On an emotional level, they say that they sometimes feel a certain agony due to not knowing how much longer the treatment will be effective. They live in a state of uncertainty that they try to cope with by focusing on their day-to-day and experience the good times deeply.
When I’m not in pain , I try not to even remember what I have and go out and have fun with my family and live . (Patient 20)
Several women who have children express with regret that they worry about their children enjoying them and remembering them when they were well. They are sad that they won’t be able to grow up in a normal family. Some also comment the impact this diagnosis is having on their partner.
What I don’t want is for them to carry this baggage of having a sick mother . (Patient 18)
A conflict with disability also appears, as many women report their desire to continue working, but feel that they can’t keep up with the pace of work. Additionally, several state that going through the medical board is a strenuous process, given that they look good physically.
It’s hard to deal with , I’m a non-practicing lawyer and I have degrees galore , but I worked the first year and I couldn’t continue . (Patient 21) Every year they call me again for the disability monitoring and they always threaten me . To be honest , the treatment doesn’t make me sick , but I don’t know how long it’s going to be like this . (Patient 19)
Social invisibility . The participants say that they do not have any physical signs of being ill, that they look fine, although they know and feel that inside, they are not well. They say that it is sometimes hard to manage socially, since on occasion, they feel misunderstood and disparaged.
I’m much sicker now , but people think or want to think that I’m fine . When I was doing chemo , it was like wearing a sign that said “cancer . ” (Patient 17)
This study describes the patient journey of women with breast cancer, specifying the different phases with the most relevant aspects of each, as well as the different cross-sectional features they report throughout the entire treatment process.
The results portray breast cancer as a process in which there is a striking feeling of loss of health and self-identity, changes in routines, personal and employment transformation, as well as emotional hardship during and after breast cancer treatment, aspects that are also reported in the literature [ 41 , 42 ]. Earlier studies state that experiencing cancer is highly stressful. It involves a major threat to life or physical integrity, in addition to mental health, interfering with the path, projects, and plans patients have for their life over the short, medium, and, on occasion, long term as well [ 6 ]. Along with reporting adverse physical and psychological impacts, patients also report positive ways in which they have grown psychologically or emotionally from the experience [ 7 , 42 ]. The diagnosis of breast cancer not only impacts the women individually, but also affects their surroundings. As reported in the literature, despite going through a very challenging time, the women struggle to put on a positive face and attempt to conserve the family’s well-being, specifically that of their children [ 7 ]. At the same time, the family is a fundamental source of support and usually provide indispensable support; however, it is not always effective, because family members do not fully understand the stresses involved in living with cancer [ 43 ]. Previous studies also reveal that for some women, their partners are one of their most significant supports; nonetheless, research also suggests that a cancer diagnosis predicts marital breakup more strongly for female survivors than males [ 44 ]. Our results reflect that the women frequently resort to other women in the same situation, possibly because they face significant unmet supportive care needs [ 30 ]. The need for social support may lead patients to seek social support groups consisting of people who are experiencing similar health crises, because such groups allow them to interact with those who best understand their suffering [ 43 ]. Another aspect that appears across the board is the relationship the participants have with the medical team. In this study, we have noted their trust in the medical team and acceptance of the treatments proposed without going into the clinical data of the disease and without needing to know the benefit provided by the treatment. Cancer patients are confronted with a potentially life-threatening [condition], feeling vulnerable, and need to rely heavily on their care providers, expecting the physician to act in their best interests [ 5 ]. Therefore, they need to have a close relationship, as well as comprehensive care [ 30 ]. Patients’ trust in a physician has been associated with a reduction of their fears and anxiety and [increased] satisfaction and adherence to treatment [ 5 , 30 ]. We believe that it would be important to provide patients with accurate information, so as to avoid misunderstandings (such as cancer being synonymous with death, regardless of stage) as several participants in this study have reported, which can lead them to believe that the risk of relapse with and without chemotherapy is much greater than the oncologists estimate [ 45 ]. We believe that in future studies that it would be worthwhile to examine the peculiarities of each kind of patient information with the aim of determining how to break it up and make it both comprehensible and tolerable to promote patients’ well-being.
A breast cancer diagnosis is generally unexpected and practically all patients suffer psychological distress, such as feelings of uncertainty, disbelief, hopelessness, vulnerability, anger, fear, anxiety, and sadness [ 46 , 47 ]. The literature has reported that many women experience peritraumatic distress or dissociation during the medical conversation in which they are given their diagnosis of cancer [ 48 ], which might account for the reactions of the respondents. Given that, when they receive their diagnosis, additional information is generally given to them, such as clinical aspects and preferred treatments. Repeating this information at subsequent appointments could contribute to improving communication with patient, since several participants stated that they found it hard to pay attention to the physician, given the emotional impact. Additionally, breast cancer patients tend to be diagnosed when they are relatively young, and often when they are in the middle furthering their career or raising children [ 12 ]. In spite of everything, the women try to put on as brave a face as they can and focus on maintaining their children’s well-being [ 7 ]. Telling children about their diagnosis is reportedly one of the biggest challenges; parents are usually unsure of how to tell them, because at the same time that they want it to be open and honest and cover their children’s developmental needs, they also want to protect them children [ 49 ].
Once diagnosed, breast cancer patients go through different treatments. The most salient experiences of these phases pertain to the impact of side effects on physical quality-of-life and psychological well-being, which is consistent with the literature [ 11 ]. Moreover, cancer therapy entails physical changes that affect their feminine identity, fertility, self-esteem, sexual functioning, and makes them more vulnerable [ 10 , 50 ]. Women described their inner self as being on an emotional rollercoaster with highs and lows throughout the various phases of treatment [ 7 ]. Given treatment side effects and sequelae, these women are more likely to experience physical symptoms and psychological disorders than patients with other kinds of tumors [ 51 ]. The side effects involve an acute sense of loss of health and quality-of-life, as well as identity and femininity. It would be interesting for future research to explore the therapies used in grief counseling with cancer patients, as understanding and exploring this perspective could comprise an additional clinical aid.
Once the women have completed their treatments, they gradually get back to normal and many contemplate returning to work. However, in line with our results, the literature reveals that even though they want to normalize their lives, female breast cancer survivors feel that they will never return to their baseline status [ 7 ]. A significant number of patients experience difficulties in physical, cognitive, and emotional functioning after their treatment, such as symptoms like lymphedema, fatigue, pain, sleep disorders, cancer-related cognitive impairment, emotional stress, symptoms of depression and anxiety, problems with relationships, reduced sexual identity, fertility problems, and fear of cancer relapse [ 13 , 14 ]. Furthermore, patients with hormone therapy suffer hot flashes, sweats, joint pain, weight gain, decreased libido, and low energy [ 52 ]. A sizeable number of these women also experience changes in employment status which can happen even 5–10 years following diagnosis [ 15 ]. Given that all these changes alter the structure of the woman’s everyday life, personalized care and treatment plans in cancer survivors are highlighted in the literature with extended specialized support being proposed that enables them to make a better psychosocially adjusted transition from treatment to follow-up [ 53 ] and advocating for the patient’s participation in all decisions that affect her during this period [ 54 ]. Further research is needed concerning how to structure the follow-up and support offered to these women during this stage so as to meet their needs and help them adjust to their new reality with the chronic sequelae caused by cancer and its treatment. On the other hand, the personal transformation of the initial stages of the journey are best seen during this phase. The literature shows that women who have had breast cancer report changes in their philosophy of life, such as embarking on a new life path, changing their priorities in life, as well as valuing life in general [ 42 ]. Most of the participants in our study place special emphasis on appreciating life, enjoying it more, and living each day to the fullest. Cancer survivors report being aware of how precarious life is, while also feeling the joy of being alive [ 55 ]. Similarly, they have been found to be more resilient and better able to repair their mood than healthy women [ 56 ].
About 5% of all patients with breast cancer are diagnosed when the disease is metastatic, whereas some 30% have suffered a relapse of an early breast cancer [ 17 ]. We saw that some women suffering a relapse after initial treatment with curative intent tend to wonder if the treatment was sufficient or if they should have done something more to prevent the relapse. Metastatic breast cancer is uncurable, which is why these women’s main psychosocial challenges are not the same as those who are diagnosed in early stages [ 18 ]. Faced with incurability, the women react with shock and fear of imminent death, but this anxiety diminishes once they begin treatment and learn that there are more treatment options [ 17 ]. During this phase, the interviewees reported impaired physical QoL and functioning, being hindered by pain, fatigue, or menopausal symptoms. Emotionally, they report suffering bouts of depression and anxiety, as well as fear because of the spread of their cancer. As for their relational QoL, their children’s welfare is their number one concern, especially for mothers of young children [ 17 , 57 ]. What’s more, these women felt isolated from society in general and, more specifically, from the non-advanced breast cancer community, inasmuch as they feel that nobody understands what they are going through [ 18 ]. A psychosocial approach is especially important in this phase to help these women to continuously adapt to the changes of their individual clinical situation and to the progression of the disease, thereby improving their coping.
Clinical implications
Having first-person information enables us to comprehend in detail the experiences of breast cancer patients, their situation, and emotional state, which favors holistic cancer care for health professionals.
Healthcare professionals should prepare women for a changed life situation, as well as to face prolonged, multimodal treatment (surgery, chemotherapy, hormone therapy, radiotherapy), and to confront physical and psychological sequelae, as well as the fear surrounding an uncertain prognosis. It is important to help them manage their expectations and fears and, to identify and address the issues and concerns that arise at different time points during treatment. The information and support offered should be adjusted to each woman’s individual needs, her life situation, her coping style, and the time and stage of their cancer. This more empathic, understanding outlook can also contribute to improving the physician-patient rapport, promoting communication, understanding, and shared decision-making.
Finally, a comprehensive understanding of the women’s psychosocial support endorses their belonging to groups of women with breast cancer, in which there is a relationship among equals. Further research is needed to specify the type needed so as to decrease both the impact of the death of women in the group, as well as the vast amount of information that they may end up obtaining, without needing it or requesting it.
Limitations
This study was performed with Spanish participants, which is why certain aspects cannot reflect the experiences of breast cancer patients from other countries, given the particularities of both the Spanish healthcare system and Spanish culture. Likewise, the data attained were specific to women with breast cancer, which can scarcely be extrapolated to individuals with other cancers. Moreover, the findings do not reflect men’s experiences with breast cancer and research with this group would enrich the field further. In addition, the age of our participants ranged from 34 to 61 years; hence the results should be interpreted for a middle-aged population and do not reflect the experiences of women diagnosed at very early or very old ages. Finally, we believe that there may be a bias regarding the women who agree to participate, as this group has probably accepted their condition more, as well as having worked on it more.
Despite these limitations, we hope that our findings can contribute to better understanding the experiences of women with breast cancer.
Acknowledgments
The authors are grateful to the investigators of the Neoetic study and the Bioetic Group of the Spanish Society of Medical Oncology (SEOM) for their contribution to this study. We would like to thank all the women who generously shared their experiences with us, the support of HealthyOnco ( www.healthyonco.com ), and Priscilla Chase Duran for editing and translating the manuscript.
- View Article
- Google Scholar
- PubMed/NCBI
Screening & Prevention
Guides & resources, salt lake city, utah county, community clinics, our cancer center, faculty & students, volunteering.

Letter of Hope from Cari Low, MD, FACP
Read Time: 2 minutes Author: Cari Low, MD, FACP , Supportive Oncology and Survivorship

Dear Patients, Families, and Loved Ones,
The phrase, “you have cancer,“ can be the most daunting anyone can hear. It creates uncertainty, fear, and a flood of questions about the future for you and your family. While the journey ahead feels overwhelming, I want to assure you that you are not alone. As part of the Supportive Oncology and Survivorship (SOS) team, we are here to support you every step of the way and help answer each of your questions.
As a palliative medicine doctor, I often encounter misunderstandings about my field. Many are unfamiliar with the term “ palliative medicine ,” confusing it with hospice care. I am not “the hospice doctor.” Instead, I like to think of myself as the “quality-of-life doctor.” My role is to help you manage the physical, emotional, and spiritual challenges through your entire cancer treatment journey.
“Many patients describe their treatment journey as a roller coaster. We are here to help you navigate the ups and downs.”
Our team of doctors, nurses, social workers, and chaplains is focused on helping you live well with your diagnosis, through treatment and beyond. We address symptoms like pain, nausea, depression, and anxiety so that you can focus on the things that bring you joy.
Working closely with your oncologists, we can ease some of the burdens, stress, and worries that come with a cancer diagnosis and its treatments. While they oversee your treatment, we dedicate our time to understanding how your illness and treatment impact your life and loved ones. While there may be difficult decisions to make, we will navigate this journey together with compassion and dignity. Above all, we respect your wishes and are here to ensure you receive care that aligns with what matters most to you. Many patients describe their treatment journey as a roller coaster. We are here to help you navigate the ups and downs.
When patients and families meet with our team, initial misconceptions quickly fall away. Feelings of apprehension are replaced with relief and comfort knowing there is an entire team here to listen, support, and encourage.
I’ve witnessed incredible strength, love, and resilience in patients like you. Your courage is an inspiration, and it is my honor to walk beside you on the path forward.
Sincerely, Cari Low, MD, FACP
Our doctors and researchers are sharing hope with patients and their loved ones. Read more Letters of Hope .
Cancer touches all of us.
- Cancer Care
- Patient And Family Support
- Letter of Hope

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Alcohol's Effects on Health
Research-based information on drinking and its impact.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Treatment for alcohol problems: finding and getting help.
This guide is written for individuals, and their family and friends, who are looking for options to address alcohol problems. It is intended as a resource to understand what treatment choices are available and what to consider when selecting among them. Please note: NIAAA recently launched the NIAAA Alcohol Treatment Navigator. This online tool helps you find the right treatment for you — and near you. It guides you through a step-by-step process to finding a highly qualified professional treatment provider. Learn more at https://alcoholtreatment.niaaa.nih.gov .
When Is It Time for Treatment?
Alcohol-related problems—which result from drinking too much, too fast, or too often—are among the most significant public health issues in the United States.
Many people struggle with controlling their drinking at some time in their lives. More than 14 million adults ages 18 and older have alcohol use disorder (AUD), and 1 in 10 children live in a home with a parent who has a drinking problem.
Does Treatment Work?
The good news is that no matter how severe the problem may seem, most people with AUD can benefit from some form of treatment.
Research shows that about one-third of people who are treated for alcohol problems have no further symptoms 1 year later. Many others substantially reduce their drinking and report fewer alcohol-related problems.
Signs of an Alcohol Problem
Alcohol use disorder (AUD) is a medical condition that doctors diagnose when a patient’s drinking causes distress or harm. The condition can range from mild to severe and is diagnosed when a patient answers “yes” to two or more of the following questions.
In the past year, have you:
Had times when you ended up drinking more, or longer than you intended?
More than once wanted to cut down or stop drinking , or tried to, but couldn’t?
Spent a lot of time drinking? Or being sick or getting over the aftereffects?
Experienced craving —a strong need, or urge, to drink?
Found that drinking—or being sick from drinking—often interfered with taking care of your home or family ? Or caused job troubles? Or school problems?
Continued to drink even though it was causing trouble with your family or friends ?
Given up or cut back on activities that were important or interesting to you, or gave you pleasure, in order to drink?
More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or having unsafe sex)?
Continued to drink even though it was making you feel depressed or anxious or adding to another health problem ? Or after having had a memory blackout ?
Had to drink much more than you once did to get the effect you want? Or found that your usual number of drinks had much less effect than before?
Found that when the effects of alcohol were wearing off, you had withdrawal symptoms , such as trouble sleeping, shakiness, irritability, anxiety, depression, restlessness, nausea, or sweating? Or sensed things that were not there?
If you have any of these symptoms, your drinking may already be a cause for concern. The more symptoms you have, the more urgent the need for change. A health professional can conduct a formal assessment of your symptoms to see if AUD is present. For an online assessment of your drinking pattern, go to RethinkingDrinking.niaaa.nih.gov .
Options for Treatment
When asked how alcohol problems are treated, people commonly think of 12-step programs or 28-day inpatient rehab but may have difficulty naming other options. In fact, there are a variety of treatment methods currently available, thanks to significant advances in the field over the past 60 years.
Ultimately, there is no one-size-fits-all solution, and what may work for one person may not be a good fit for someone else. Simply understanding the different options can be an important first step.
Types of Treatment
Behavioral treatments.
Behavioral treatments are aimed at changing drinking behavior through counseling. They are led by health professionals and supported by studies showing they can be beneficial.
Medications
Three medications are currently approved in the United States to help people stop or reduce their drinking and prevent relapse. They are prescribed by a primary care physician or other health professional and may be used alone or in combination with counseling.
Mutual-Support Groups
Alcoholics Anonymous (AA) and other 12-step programs provide peer support for people quitting or cutting back on their drinking. Combined with treatment led by health professionals, mutual-support groups can offer a valuable added layer of support.
Due to the anonymous nature of mutual-support groups, it is difficult for researchers to determine their success rates compared with those led by health professionals.
Starting With a Primary Care Doctor
For anyone thinking about treatment, talking to a primary care physician is an important first step—he or she can be a good source for treatment referrals and medications. A primary care physician can also:
Evaluate a patient’s drinking pattern
Help craft a treatment plan
Evaluate overall health
Assess if medications for alcohol may be appropriate
Individuals are advised to talk to their doctors about the best form of primary treatment.
Types of Professionals Involved in Care
Treatments led by health professionals.
Professionally led treatments include:

Some are surprised to learn that there are medications on the market approved to treat alcohol dependence. The newer types of these medications work by offsetting changes in the brain caused by AUD.
All approved medications are non-addictive and can be used alone or in combination with other forms of treatment. Learn more about these approved treatments .
Also known as alcohol counseling, behavioral treatments involve working with a health professional to identify and help change the behaviors that lead to heavy drinking. Behavioral treatments share certain features, which can include:
Developing the skills needed to stop or reduce drinking
Helping to build a strong social support system
Working to set reachable goals
Coping with or avoiding the triggers that might cause relapse
Types of Behavioral Treatments
Cognitive–Behavioral Therapy can take place one-on-one with a therapist or in small groups. This form of therapy is focused on identifying the feelings and situations (called “cues”) that lead to heavy drinking and managing stress that can lead to relapse. The goal is to change the thought processes that lead to alcohol misuse and to develop the skills necessary to cope with everyday situations that might trigger problem drinking.
Motivational Enhancement Therapy is conducted over a short period of time to build and strengthen motivation to change drinking behavior. The therapy focuses on identifying the pros and cons of seeking treatment, forming a plan for making changes in one’s drinking, building confidence, and developing the skills needed to stick to the plan.
Marital and Family Counseling incorporates spouses and other family members in the treatment process and can play an important role in repairing and improving family relationships. Studies show that strong family support through family therapy increases the chances of maintaining abstinence (stopping drinking), compared with patients undergoing individual counseling.
Brief Interventions are short, one-on-one or small-group counseling sessions that are time limited. The counselor provides information about the individual’s drinking pattern and potential risks. After the client receives personalized feedback, the counselor will work with him or her to set goals and provide ideas for helping to make a change.
Ultimately, choosing to get treatment may be more important than the approach used, as long as the approach avoids heavy confrontation and incorporates empathy, motivational support, and a focus on changing drinking behavior.
What FDA-Approved Medications Are Available?
Certain medications have been shown to effectively help people stop or reduce their drinking and avoid relapse.
Current Medications
The U.S. Food and Drug Administration (FDA) has approved three medications for treating alcohol dependence, and others are being tested to determine whether they are effective.
Naltrexone can help people reduce heavy drinking.
Acamprosate makes it easier to maintain abstinence.
Disulfiram blocks the breakdown (metabolism) of alcohol by the body, causing unpleasant symptoms such as nausea and flushing of the skin. Those unpleasant effects can help some people avoid drinking while taking disulfiram.
It is important to remember that not all people will respond to medications, but for a subset of individuals, they can be an important tool in overcoming alcohol dependence.
Scientists are working to develop a larger menu of pharmaceutical treatments that could be tailored to individual needs. As more medications become available, people may be able to try multiple medications to find which they respond to best.
“Isn’t taking medications just trading one addiction for another?”
This is not an uncommon concern, but the short answer is “no.” All medications approved for treating alcohol dependence are non-addictive. These medicines are designed to help manage a chronic disease, just as someone might take drugs to keep their asthma or diabetes in check.
Looking Ahead: The Future of Treatment
Progress continues to be made as researchers seek out new and better treatments for alcohol problems. By studying the underlying causes of AUD in the brain and body, the National Institute on Alcohol Abuse and Alcoholism (NIAAA) is working to identify key cellular or molecular structures—called “targets”—that could lead to the development of new medications.
Personalized Medicine
Ideally, health professionals would be able to identify which AUD treatment is most effective for each person. NIAAA and other organizations are conducting research to identify genes and other factors that can predict how well someone will respond to a particular treatment. These advances could optimize how treatment decisions are made in the future.
Current NIAAA Research—Leading to Future Breakthroughs
Certain medications already approved for other uses have shown promise for treating alcohol dependence and problem drinking:
The anti-smoking drug varenicline (marketed under the name Chantix) significantly reduced alcohol consumption and craving among people with AUD.
Gabapentin, a medication used to treat pain conditions and epilepsy, was shown to increase abstinence and reduce heavy drinking. Those taking the medication also reported fewer alcohol cravings and improved mood and sleep.
The anti-epileptic medication topiramate was shown to help people curb problem drinking, particularly among those with a certain genetic makeup that appears to be linked to the treatment’s effectiveness.
Tips for Selecting Treatment
Professionals in the alcohol treatment field offer advice on what to consider when choosing a treatment program.
Overall, gather as much information as you can about the program or provider before making a decision on treatment. If you know someone who has first-hand knowledge of the program, it may help to ask about his or her personal experience.
Here are some questions you can ask that may help guide your choice:
What kind of treatment does the program or provider offer? It is important to gauge whether the facility provides all the currently available methods or relies on one approach. You may want to learn if the program or provider offers medication and if mental health issues are addressed together with addiction treatment.
Is treatment tailored to the individual? Matching the right therapy to the individual is important to its success. No single treatment will benefit everyone. It may also be helpful to determine whether treatment will be adapted to meet changing needs as they arise.
What is expected of the patient? You will want to understand what will be asked of you in order to decide what treatment best suits your needs.
Is treatment success measured? By assessing whether and how the program or provider measures success, you may be able to better compare your options.
How does the program or provider handle relapse? Relapse is common, and you will want to know how it is addressed. For more information on relapse, see Relapse Is Part of the Process .
When seeking professional help, it is important that you feel respected and understood and that you have a feeling of trust that this person, group, or organization can help you. Remember, though, that relationships with doctors, therapists, and other health professionals can take time to develop.
Additional Considerations
Treatment Setting—Inpatient or Outpatient?
In addition to choosing the type of treatment that’s best for you, you’ll also have to decide if that treatment is inpatient (you would stay at a facility) or outpatient (you stay in your home during treatment). Inpatient facilities tend to be more intensive and costly. Your healthcare provider can help you evaluate the pros and cons of each.
Cost may be a factor when selecting a treatment approach. Evaluate the coverage in your health insurance plan to determine how much of the costs your insurance will cover and how much you will have to pay. Ask different programs if they offer sliding scale fees—some programs may offer lower prices or payment plans for individuals without health insurance.
An Ongoing Process
Overcoming alcohol use disorder is an ongoing process, one which can include setbacks.
The Importance of Persistence
Because AUD can be a chronic relapsing disease, persistence is key. It is rare that someone would go to treatment once and then never drink again. More often, people must repeatedly try to quit or cut back, experience recurrences, learn from them, and then keep trying. For many, continued follow up with a treatment provider is critical to overcoming problem drinking.
Relapse Is Part of the Process
Relapse is common among people who overcome alcohol problems. People with drinking problems are most likely to relapse during periods of stress or when exposed to people or places associated with past drinking.
Just as some people with diabetes or asthma may have flare-ups of their disease, a relapse to drinking can be seen as a temporary setback to full recovery and not a complete failure. Seeking professional help can prevent relapse—behavioral therapies can help people develop skills to avoid and overcome triggers, such as stress, that might lead to drinking. Most people benefit from regular checkups with a treatment provider. Medications also can deter drinking during times when individuals may be at greater risk of relapse (e.g., divorce, death of a family member).
Mental Health Issues and Alcohol Use Disorder
Depression and anxiety often go hand in hand with heavy drinking. Studies show that people who are alcohol dependent are two to three times as likely to suffer from major depression or anxiety over their lifetime. When addressing drinking problems, it’s important to also seek treatment for any accompanying medical and mental health issues.
Advice For Friends and Family Members
Caring for a person who has problems with alcohol can be very stressful. It is important that as you try to help your loved one, you find a way to take care of yourself as well. It may help to seek support from others, including friends, family, community, and support groups. If you are developing your own symptoms of depression or anxiety, think about seeking professional help for yourself. Remember that your loved one is ultimately responsible for managing his or her illness.
However, your participation can make a big difference. Based on clinical experience, many health providers believe that support from friends and family members is important in overcoming alcohol problems. But friends and family may feel unsure about how best to provide the support needed. The groups for family and friends listed below may be a good starting point.
Remember that changing deep habits is hard, takes time, and requires repeated efforts. We usually experience failures along the way, learn from them, and then keep going. AUD is no different. Try to be patient with your loved one. Overcoming this disorder is not easy or quick.
Pay attention to your loved one when he or she is doing better or simply making an effort. Too often we are so angry or discouraged that we take it for granted when things are going better. A word of appreciation or acknowledgement of a success can go a long way.
Professional help
Your doctor. Primary care and mental health practitioners can provide effective AUD treatment by combining new medications with brief counseling visits. To aid clinicians, NIAAA has developed a guide for younger patients, Alcohol Screening and Brief Intervention for Youth: A Practitioner’s Guide . This guide and other resources are available at https://www.niaaa.nih.gov/health-professionals-communities .
Specialists in AUD. For specialty addiction treatment options, contact your doctor, health insurance plan, local health department, or employee assistance program. Other resources include:
Medical and non-medical addiction specialists
American Academy of Addiction Psychiatry 401–524–3076
American Psychological Association 1–800–964–2000 (ask for your state’s referral number to find psychologists with addiction specialties)
American Society of Addiction Medicine 301–656–3920 (ask for the phone number of your state’s chapter)
NAADAC, the Association for Addiction Professionals 1–800–548–0497
National Association of Social Workers (search for social workers with addiction specialties)
Treatment facilities
Substance Use Treatment Facility Locator 1–800–662–HELP
Mutual-support groups
Alcoholics Anonymous (AA) 212–870–3400
Moderation Management 212–871–0974
Secular AA Calendar of worldwide secular meetings
SMART Recovery 440–951–5357
Women for Sobriety 215–536–8026
Groups for family and friends
Al-Anon Family Groups 1–888–425–2666 for meetings
Adult Children of Alcoholics 310–534–1815
Information resources
National Institute on Alcohol Abuse and Alcoholism 301–443–3860
National Institute on Drug Abuse 301–443–1124
National Institute of Mental Health 1–866–615–6464
Research shows that most people who have alcohol problems are able to reduce their drinking or quit entirely.
There are many roads to getting better. What is important is finding yours.
Understanding the available treatment options—from behavioral therapies and medications to mutual-support groups—is the first step. The important thing is to remain engaged in whatever method you choose.
Ultimately, receiving treatment can improve your chances of success.
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- Medical Devices
- Products and Medical Procedures
- Dental Devices
Dental Implants: What You Should Know
Dental implants are medical devices surgically implanted into the jaw to restore a person's ability to chew or their appearance. They provide support for artificial (fake) teeth, such as crowns, bridges, or dentures.
On this page:
Recommendations for patients, benefits and risks.
- Reporting Problems to the FDA
Additional Resources
When a tooth is lost due to injury or disease, a person can experience complications such as rapid bone loss, defective speech, or changes to chewing patterns that result in discomfort. Replacing a lost tooth with a dental implant can significantly improve the patient's quality of life and health.
Dental implant systems consist of a dental implant body and dental implant abutment and may also include an abutment fixation screw. The dental implant body is surgically inserted in the jawbone in place of the tooth's root. The dental implant abutment is usually attached to the implant body by the abutment fixation screw and extends through gums into the mouth to support the attached artificial teeth.
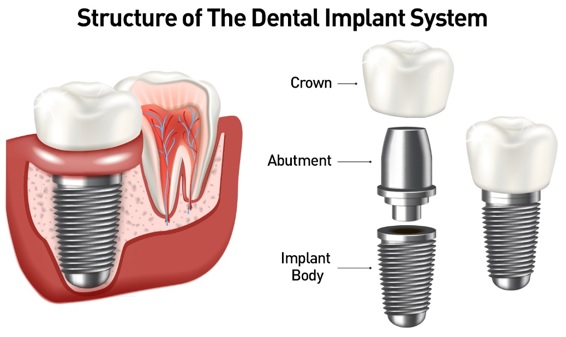
Figure 1. Structure of The Dental Implant System
Before choosing dental implants, talk to your dental provider about the potential benefits and risks, and whether you are a candidate for the procedure. Things to consider:
- Your overall health is an important factor in determining whether you are a good candidate for dental implants, how long it will take to heal, and how long the implant may stay in place.
- Ask your dental provider what brand and model of dental implant system is being used and keep this information for your records.
- Smoking may affect the healing process and decrease the long-term success of the implant.
- The healing process for the implant body may take several months or longer, during which time you typically have a temporary abutment in place of the tooth.
After the dental implant procedure:
- Carefully follow the oral hygiene instructions given to you by your dental provider. Regularly cleaning the implant and surrounding teeth is very important for long-term success of the implant.
- Schedule regular visits with your dental provider.
- If your implant feels loose or painful, tell your dental provider right away.
Dental implants can significantly improve the quality of life and the health of a person who needs them. However, complications may sometimes occur. Complications can occur soon after dental implant placement or much later. Some complications result in implant failure (usually defined as implant looseness or loss). Implant failure can result in the need for another surgical procedure to fix or replace the implant system.
Benefits of Dental Implant Systems:
- Restores the ability to chew
- Restores cosmetic appearance
- Helps keep the jawbone from shrinking due to bone loss
- Preserves the health of the surrounding bone and gums
- Helps keep adjacent (nearby) teeth stable
- Improves quality of life
Risks Associated with Dental Implant Systems:
- Damage to surrounding natural teeth during implant placement
- Injury to the surrounding tissues during surgery, such as sinus perforation
- Injury during surgery (for example, fracture of surrounding jawbone)
- Inadequate function, such as feeling like the teeth do not bite together normally
- A sensation that the tooth is loose or twisting in place resulting from an abutment screw loosening
- due to systemic infection, which may be more likely in patients with uncontrolled diabetes
- due to local infection in bone and gums supporting the implant body
- due to delayed healing, which may be more likely in patients who smoke
- Difficulty cleaning the gums around the implant, resulting in poor oral hygiene
- Untreated periodontal disease
- Post-surgical numbness due to nerve impingement or damage
- Always notify health care providers and imaging technicians that you have dental implants before any magnetic resonance imaging (MRI) or x-ray procedures. Dental implants can distort or interfere with these images. FDA is not aware of any adverse events reported for MRI or x-ray procedures with dental implants.
Ways Dental Implants are Evaluated for Safety
Dental implants systems are typically made of materials that follow international consensus standards of the International Organization for Standardization (ISO) or ASTM International. These standards have details of what makes a safe material. Most dental implant systems are made of titanium or zirconium oxide. Other materials such as gold alloys, cobalt-based alloys, titanium alloys, or ceramic materials are sometimes used. The safety profiles of these materials are well-known.
Dental implant systems are evaluated according to international consensus standards. Biocompatibility testing, to show that bodily contact with the device does not cause complications like irritation or allergic reaction, is part of the evaluation that helps ensure the materials in the dental implant system are safe and do not cause adverse effects when implanted in people.
For manufacturers to market dental implant systems in the United States, they must first show the FDA their systems are as safe and as effective as dental implant systems already on the market.
Reporting Dental Implant System Problems to the FDA
Prompt reporting of adverse events can help the FDA identify and better understand the risks associated with medical products. If you have problems associated with your dental implant system including the dental implant body, the dental abutment, or the dental abutment screw, we encourage you to file a voluntary report through MedWatch , the FDA Safety Information and Adverse Event Reporting program.
To help us learn as much as possible about the adverse events associated with dental implant systems, please include the following information in your report, if available:
- Date of device implantation
- Identification of dental implant system used
- Description of the problem including date of onset, and any diagnosis and follow-up treatment
- Description of medical or surgical interventions taken, including prior interventions, if any
- Pertinent medical and dental history
- American Dental Association (ADA), "PatientSmart Patient Education Center: Dental Implants"
- American Academy of Periodontology (AAP), "Dental Implants"
We use cookies to improve your experience. By using our site, you agree to this. Legal Notices
Mobile Menu
- Careers/Jobs
- Contact/Appointments
- Find A Doctor
- Medical Records
- MyGillette (portal)
Wyatt’s Journey Through Clubfoot Treatment
By Emma Willms and Ben Brewer (photos)
June 11, 2024
Wyatt Krentz’s path to a diagnosis of clubfoot began early—in fact, the process started before he was even born. “We had an ultrasound in October of 2022, at 20 weeks [of pregnancy], where my doctor said that there was a strong possibility that Wyatt would be born with clubfoot,” shares Wyatt’s mom, Katie. “It was confirmed at a [second] ultrasound in December.”
What is clubfoot?
Clubfoot —also known as talipes equinovarus—is a condition that affects infants at birth. Some children have one affected foot, while others experience the condition in both feet. In mild cases, the foot might be quite flexible. In more severe situations, the foot is more rigid. If left untreated, clubfoot can cause difficulties with walking. The condition affects about one out of every 1,000 children, and ultrasound technology can sometimes detect clubfoot before birth. While the exact cause of clubfoot is not yet known, it is a highly treatable condition.

Any diagnosis can sound scary when there’s a child involved. Katie says, “At first, it was just heartbreaking. Hearing about the diagnosis, I was scared at first … I just wasn’t sure I could handle something like clubfoot.” Wyatt was to be the fourth Krentz child to join the family, and Katie was concerned about what caring for a baby with clubfoot might look like.
Fortunately, Gillette Children’s was with Wyatt and his family every step of the way. Thanks to Gillette’s clubfoot clinic—conducted by our internationally recognized pediatric orthopedic experts —as well as an in-house casting team, Wyatt was able to go through the entire clubfoot treatment process on site. “All of our clubfoot appointments have been conducted at Gillette. Wyatt began the serial casting process on May 1, 2023. He got new casts every Monday for eight weeks, until his tenotomy procedure on June 26,” Katie offers.
Phase 1: Wyatt Receives Clubfoot Casting at Gillette
From his first Gillette appointment, Wyatt has been seen by board-certified orthopedic surgeons, pediatric orthopedic surgery specialists, and physician assistants who specialize in the treatment and correction of clubfoot in the youngest of patients—Wyatt began the serial casting process for clubfoot at just a month and a half old. “I was scared,” Katie shares, “but he has been a dream. He went through eight weeks of casting, and I believe he slept through at least the first four casting procedures that he had!”
Wyatt’s care team includes Megan Haselbauer, PA-C , and Alison Schiffern, MD . “Usually, babies tolerate the casting part of the treatment quite well,” Dr. Schiffern says. She notes that the weekly casting phase of clubfoot often lasts anywhere from five to eight weeks, “but it can vary between patients. We determine casting needs based on the progress the foot is making each week, and each week make a determination of when the baby is ready for next steps."
Wyatt’s treatment being in such capable hands helped put Katie’s mind at ease. “Our casting nurse, Tianne, was such a welcome presence each week at our casting appointments. Her calming support made me feel like we would get through this process just fine. Dr. Schiffern and Megan Haselbauer have been outstanding. They take their time when meeting with us, and clearly explain what we could expect at each appointment. I appreciate a medical professional who can talk to families and make us feel heard.”
Wyatt's family documented each phase of his treatment for clubfoot.
Phase 2: Wyatt Undergoes an Achilles Tenotomy for Clubfoot
Following the casting phase, Wyatt was ready to undergo an Achilles tenotomy . The Achilles is the thick tendon located at the back of the leg, near the ankle. In babies with clubfoot, this tendon (along with the calf muscles) is usually very tight and needs to be lengthened with surgery. A tenotomy lengthens the Achilles tendon and improves flexibility in the ankle. Due to his age, Wyatt had his tenotomy performed in the clinic with local anesthesia (numbing medicine). Local anesthesia is often an option for babies up to about six months of age. If the child has the tenotomy after the age of six months, they will often be sedated or put under general anesthesia for the procedure.
Phase 3: Wyatt Eases Into the Clubfoot Bracing Process

Once Wyatt had recovered from his tenotomy, he began the bracing phase of the treatment process—also known as the “boots and bar” phase.
Dr. Schiffern says, “The transition to bracing—the bar and shoes—is often harder for families and babies to get used to. After the initial adjustment period, bracing is usually well tolerated if families are compliant with doing it every night, so the child gets used to it.”
Katie and the rest of Wyatt’s family were relieved to find that Wyatt tolerates this third phase of clubfoot treatment just as well as the first two. “He hates having things put over his head, which is hard because he’s a baby and we have to change his clothes often,” says Katie. “But he seems to be OK with the boots and bar—he plays with the bar while we put the [boots] on, and then when it’s time for us to put the bar on, that’s when he gets to hold his toothbrush.” Wyatt will wear his boots and bar setup part-time until he is four years old, according to his care team.
For Wyatt’s most recent boots and bar appointment, he was joined by one of his older siblings—sister Harper, age 10, who dotes on him. “He is SO loved by his siblings. Wyatt has always had a special bond with Harper. From early on he has always smiled at her, he looks for her and will crawl after her. We are so lucky to have her help!” Other siblings Amelia, age 7, and Aiden, age 5, love to hold Wyatt and give him kisses whenever he passes by. “We are incredibly blessed having such amazing big siblings for our baby!” Katie gushes.
Katie Shares Her Advice for Parents of Children with Clubfoot
Katie and the rest of Wyatt’s family have learned a lot from Wyatt’s journey through the clubfoot treatment process. “If I could give some advice to families newly diagnosed with clubfoot, I would just say to snuggle your baby. Whenever Wyatt was uncomfortable, or adjusting to a new step in the process, we would snuggle him, and everything seemed to be just fine.”
Katie credits the professionals at Gillette for making a daunting process go smoothly. “Trust yourselves as parents and trust the amazing team at Gillette. Now, on the other side of the most intensive part of this journey, I am breathing a sigh of relief that nothing was as hard as I had imagined it would be. Our love for Wyatt far outweighed any sort of challenge or obstacle that stood in our way.”
Pediatric Expert Consults
Do these symptoms sound familiar? Our 30-minute consult appointment could help get answers.
Request An Appointment
Request an appointment to connect with Gillette providers.
Find the Right Care
Meet a care team provider , find a location , learn how to get a second opinion , and more.
Gillette kids fuel our mission. You provide the spark. Donate today.
- Close the Gap
- SurvivorNetTV
- Clinical Trials
Rapper Turned Country Singer Jelly Roll, 39, and Wife, Bunnie XO, 44, are Starting Their IVF Journey & Striving to be Healthier: ‘I Just Want to Feel Good’ SHARE
- Acute Myeloid Leukemia (AML)
- Bladder Cancer
- Breast Cancer
- Chronic Lymphocytic Leukemia (CLL)
- Chronic Myeloid Leukemia (CML)
- Colon Cancer
- Endometrial Cancer
- Esophageal Cancer
- Heart Failure
- Hypertrophic Cardiomyopathy (HCM)
- Liver Cancer
- Lung Cancer
Multiple Myeloma
Discover local multiple myeloma resources:.
- Multiple Sclerosis (MS)
- Myelodysplastic Syndrome (MDS)
- Myeloproliferative Neoplasms
- Non-Hodgkin Lymphoma
Ovarian Cancer
Discover local ovarian cancer resources:.
- Prostate Cancer
- Rare Diseases Cold Agglutinin Disease (CAD) Transthyretin Amyloid Cardiomyopathy (ATTR-CM) Von Hippel-Lindau Disease
- SN Guides: Critical information from SurvivorNet's experts
- Mental Health: Helping patients find the balance critical to treatment and recovery
- Clinical Trial Finder: Search for clinical trials that fit your profile
Multiple Myeloma: Main Page
Discover local multiple myeloma resources:, ovarian cancer: main page, discover local ovarian cancer resources:.
- Cold Agglutinin Disease (CAD)
- Mental Health
- Transthyretin Amyloid Cardiomyopathy (ATTR-CM)
- Von Hippel-Lindau Disease
- Newsletters and Guides
Rapper Turned Country Singer Jelly Roll, 39, and Wife, Bunnie XO, 44, are Starting Their IVF Journey & Striving to be Healthier: ‘I Just Want to Feel Good’
- Save This Video
Weight, Cancer Risk, and Fertility
- Rapper turned singer Jelly Roll and his 44-year-old wife, Bunnie XO, revealed they have embarked on an in vitro fertilization journey (IVF).
- Their hope to have a child comes after Jelly Roll recently lost 70 pounds and has been working on feeling better both physically and mentally.
- Many couples, at one point or another, experience infertility. According to the Centers for Disease Control and Prevention (CDC), within the U.S., “about one in five” married women between the ages of 15 to 49 with no prior births are unable to get pregnant after trying for a year. Additionally, “one in four” women in this group struggle to get pregnant or carry the pregnancy to term.
- Although, Jelly Roll and Bunny XO have not battled cancer, fertility struggles are something many who have gone through cancer can relate to, as certain cancer treatments can cause infertility. Fortunately, in many cases, efforts can be made before beginning treatment to help preserve fertility.
The 39-year-old Tennessee native—who married his wife back in 2016, has two kids from previous relationships, and supported his late father-in-law’s courageous stage four cancer battle —spoke about trying to have kids and why he’s working harder than ever on getting fit in a recent podcast episode.
View this post on Instagram A post shared by Bunnie Xo. (@xomgitsbunnie)
Jelly Roll, who has two children from previous relationships, 16-year-old Bailee Ann and 7-year-old Noah Buddy, opened up about him and his wife’s fertility journey after looking back on what motivated him to lose 60 pounds, saying, “I think it was realizing that I just want to feel good.”
He explained, “I thought that every problem I ever had in life would be solved if I ever found any kind of success and stability. And then I started to get success and stability and still none of those problems are solved.
Helping Patients With Fertility Resources
- After A Cancer Diagnosis: Getting Fertility Hormone Injections
- How Does Chemotherapy Affect Fertility?
- New Evidence That IVF Is Linked To Higher Rates Of Breast Cancer– A Leading Expert Explains Why Women Shouldn’t Necessarily Be Alarmed
- Preserving Fertility During Cancer Treatment: What Are the Options?
“My plan was never to be 60. It was to be, like, 55. But now I’m like, ‘Well, I’d like to see my 60s.’ You know what I mean? And that really lit it up.”
RELATED: Major Reduction in Cancer Risk by Following Old Standbys Diet and Exercise
His wife also offered some insight into their fertility journey by re-sharing her husband’s podcast interview on Instagram and writing in overlay text, “We had planned on doing this privately, but decided our IVF journey needed to be shared because we’ve always been so open. And w/ all odds stacked against us, it’s already been hard & we have only just begun.
“J & I are so excited & scared all at the same time. We genuinely never thought we’d want to add to our family but something changed this year & we both just want a piece of us together to add to our already perfect family with Bailee & Noah.”
“God Willing- Baby DeFord 2026,” Bunnie XO wrote alongside the post.
Last year, Jelly Roll spoke with Fox News Digital during the 2023 CMA Awards, saying, “I don’t even have a goal when it comes to health.
“I just want to keep doing the right thing and feeling better. I’m starting to find a will to live and I wanna lean into that, that’s it. I just want to be happier.
He added, “Weight is normally directly related to mental health, so I’m trying to get that under control and the rest is following that.”
Guidance for Staying Healthy
We admire Jelly Roll for staying dedicated on his weight loss journey as he strives to live a longer life. It’s important to remember that working out and being nutritious doesn’t need to a scary experience.
In order to stay healthy, taking just a little time out of your day can make a huge difference.
Here are a few tips to be proactive:
- Take a little time to work out. This could be a walk around the block or light yoga class.
- Incorporate more fruits and vegetables into your diet.
- Cut down on alcohol intake. Moderation is key.
- Try substituting foods with sugar and carbs with healthier alternatives.
- Get up and move a few times a day.
Krista Maruschak explains how cutting “pro inflammatory” foods can decrease cancer risk
How Cancer Treatment Impacts Fertility
Although Jelly Roll and Bunny XO have not battled cancer, fertility struggles are something many who have gone through cancer can relate to, as certain cancer treatments can cause infertility. Fortunately, in many cases, efforts can be made before beginning treatment to help preserve fertility.
What’s more, many otherwise healthy couples, at one point or another, experience infertility. According to the Centers for Disease Control and Prevention (CDC), within the U.S., “about one in five” married women between the ages of 15 to 49 with no prior births are unable to get pregnant after trying for a year. Additionally, “one in four” women in this group struggle to get pregnant or carry the pregnancy to term.
Infertility may affect many cancer patients undergoing treatment due to cancer treatment’s impacts on the body. Various cancer treatments, including chemotherapy and radiation, can affect both men’s and women’s fertility. Before undergoing cancer treatment, patients should speak to their doctors about fertility preservation if they wish to have a family in the future.
Dr. Terri Woodard explains fertility preservation options patients have when going through cancer treatment.
Cancer’s Impact on Male Fertility
Cancer treatments like chemotherapy can damage sperm in men, and hormone therapy can decrease sperm production, according to the National Cancer Institute . Radiation treatment can also lead to lower sperm count and testosterone levels, impacting fertility.
These possible side effects of cancer treatment should be discussed with your doctor before starting treatment. Men may have the option to store their sperm in a sperm bank before treatment to preserve fertility.
This sperm can then be used later as part of in vitro fertilization (IVF), a procedure in which a woman’s egg is fertilized with sperm in a lab. The embryo is then transferred to a woman’s uterus to develop.
Cancer’s Impact on Female Fertility
Just as cancer treatment can impact men’s fertility, women may also be affected. Some types of chemotherapy can destroy eggs in the ovaries. This can make it impossible or difficult to get pregnant later. Whether or not chemotherapy makes a woman infertile depends on the type of drug and her age since egg supply decreases with age.
“The risk is greater the older you are,” reproductive endocrinologist Dr. Jaime Knopman told SurvivorNet. “If you’re 39 and you get chemo that’s toxic to the ovaries, it’s most likely to make you menopausal. But, if you’re 29, your ovaries may recover because they have a higher baseline supply.”
Radiation to the pelvis can also destroy eggs. It can damage the uterus, too. Surgery to your ovaries or uterus can hurt fertility as well.
Meanwhile, endocrine or hormone therapy may block or suppress essential fertility hormones and may prevent a woman from getting pregnant. This infertility may be temporary or permanent, depending on the type and length of treatment.
If you are having a treatment that includes infertility as a possible side effect, your doctor won’t be able to tell you for sure whether you will have this side effect. That’s why you should discuss your options for fertility preservation before starting treatment.
Research shows that women who have fertility preserved before breast cancer treatment are more than twice as likely to give birth after treatment than those who don’t take fertility-preserving measures.
Most women who preserve their fertility before cancer treatment do so by freezing their eggs or embryos.
After you finish your cancer treatment , a doctor who specializes in reproductive medicine can implant one or more embryos in your uterus or the uterus of a surrogate with the hope that it will result in pregnancy.
If you freeze eggs only before treatment, a fertility specialist can use sperm and your eggs to create embryos in vitro and transfer them to your uterus.
Contributing: SurvivorNet Staff
Learn more about SurvivorNet's rigorous medical review process.
Danielle Cinone is a writer at SurvivorNet. Read More
Watch the first TV channel for survivors. Stories of hope, courage, and perseverance.
SurvivorNetTV. Hope. Science. Inspiration.
Related articles.
Life After Hardship—Mom Who Had ‘Rainbow Baby’ Via Surrogate ‘Enjoying Transitioning Into Thriving Mode’ After Battle With Synovial Sarcoma
Motherhood After Cancer: Actress Christina Applegate, 52, Had Her Daughter After Battling Breast Cancer— Other Women Are Likely To Have Similar Success, New Study Reveals
Managing Chronic MS, ‘The Sopranos’ Star Jamie-Lynn Sigler, 42, Suggests Style Change to Adult Diapers To Support Her ‘Mood’ While Living With MS
Inspired By Kate Middleton— ‘Leverage Redemption’ Star Gina Bellman, 57, Now ‘Has The Courage’ To Share Her Breast Cancer Diagnosis
Get SurvivorNet in Your Inbox
Our newsletter – vital information, hope, and healing, delivered weekly.
Introducing, the Journey Bar
Use this bar to access information about the steps in your cancer journey.
Sign Up for SN+
Sign up now for access to powerful tools, top experts, and customized information to help you fight cancer.
- Personalized content tailored to your profile and disease type
- Access exclusive patient guides
- Breaking treatment information and expert perspectives
- and more...
Already have an account? Sign In
- Sign-In with Facebook
- Sign-In with Google
Don't have an account? Sign In
Sign In to SN+
Username or email address *
Remember me
Lost your password?
Not a member yet? Register now.
Don't have an account? Sign Up
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cancers (Basel)
- PMC10136947

Patient Experience Factors and Implications for Improvement Based on the Treatment Journey of Patients with Head and Neck Cancer
1 Department of Service Design, Graduate School of Industrial Arts, Hongik University, Seoul 04066, Republic of Korea; rk.ca.kignoh@ookry
Eunjeong Kim
2 Department of Industry-Academic Cooperation Foundation, The Catholic University of Korea, Seoul 06591, Republic of Korea; [email protected]
3 Department of Visual Communication Design, Graduate School of Design, Hongik University, Seoul 04066, Republic of Korea; moc.revan@ujny8130
Innchul Nam
4 Department of Otorhinolaryngology-Head and Neck Surgery, Incheon St. Mary’s Hospital, The Catholic University of Korea, Incheon 21431, Republic of Korea
Associated Data
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Simple Summary
Understanding the patients’ problems is essential to improve their quality of life. Through interviews and observations with patients, caregivers, and medical staff, we aimed to identify the various issues experienced by head and neck cancer patients during the treatment process and suggest improvement directions. As a result, the patients wanted to obtain comprehensive and reliable information during the treatment process. The patient also wished the medical staff could explain things easily so they could understand. For continuing long-term treatment, it was important for medical staff to encourage the patients and build a relationship with them. To successfully treat head and neck cancer patients, we need to consider what information should be delivered, how we should provide it, and how we can encourage them to support their emotions.
Based on the treatment journey, this study aimed to present insights into improving the patient-centered service experience for head and neck cancer (HNC) patients. We interviewed and observed patients, caregivers, and doctors. We conducted a qualitative content analysis and service clue analysis to identify barriers and enablers to patient care and to derive insights into the patient experience (PE). We received feedback from doctors considering the priority, importance, and feasibility of improvements and classified the insights into three service experience aspects, to suggest improvement directions. As a result, the ‘functional’ aspect of service experience stressed the importance of a comprehensive guide to the treatment process, delivery of reliable information, use of easy-to-understand terms, repeated summary explanations, the establishment of close and flexible linkages between departments, and the provision of educational programs. Regarding the ‘mechanic’ aspect, the use of large and clear visuals for patients, to easily understand the care information provided by medical staff was distinguished. In the ‘humanic’ aspect, patients’ psychological stability, trust in doctors, and doctor’s encouragement and support through maintaining a positive attitude were prioritized. This qualitative study provided integrative insights into the HNC patient experience, through the application of service design methodologies, such as a patient journey map, participatory research methods, and service experience clues.
1. Introduction
Patient-centeredness is one of the critical elements of high-quality care [ 1 ], and hospitals increasingly emphasize a patient-centered approach [ 2 , 3 ]. Patient-centered care (PCC) provides meticulous care in response to patient preferences and values, and patient opinion must be considered when making treatment decisions [ 1 , 4 , 5 ]. Understanding PE factors helps provide quality care in various respects, such as improved health outcomes, increased patient satisfaction, and reduced health costs [ 4 , 5 ]. PCC encompasses diverse aspects of healthcare, such as the hospital system (transitional care, coordination, care access), information and communication, and caregiver support [ 5 ]. This approach is essential to facilitate the various interactions between stakeholders, such as patients, caregivers, family members, and medical staff.
Due to the importance of PCC, many centers are trialing a user-centered approach through collaborations with designers, to improve PE [ 3 , 6 ]. This entails designing new processes based on a product or service for a patient-centered experience [ 7 ] and effectively identifying improvements to existing problems [ 3 , 8 , 9 , 10 ].
Service design aims to understand the user experience and suggest meaningful insights for a user-centered solution. It is a practical approach to PCC in healthcare [ 11 ] and includes the various stakeholders, such as the patients, caregivers, and medical staff [ 12 ]. It focuses on efficiently improving various problems in the interaction between stakeholders [ 7 ], by employing participatory research methods through patient engagement. As an effective way to engage patients in complex healthcare problem-solving processes, design ethnography, such as observation and interviews to gain understanding of the patient, can be applied to record PE and collect related data. This helps to understand the underlying meanings the patient may not express directly. A patient journey map (JM) is also a valuable method of providing medical services from a user-centered point of view, by actively managing the patient’s perspective [ 13 , 14 , 15 , 16 ]. Previous studies have confirmed the importance of understanding the patient journey, by translating intangible data into a concrete structure [ 3 , 8 , 17 , 18 , 19 ]. A JM is a visual representation of the sequence of a service process [ 11 ] and helps in understanding the service system and gaining insights into the journey stages [ 3 , 13 , 14 , 15 , 20 ]. A JM considers the overall process of the patient journey from a holistic viewpoint, such as actions, emotions, and touchpoints (a contact point of interaction between a user and a service provider, system, or product). It facilitates understanding and communication among stakeholders for problem-solving. A JM identifies and visualizes the patient treatment journey and analyzes the behavior, emotions, and tangible and intangible experiences through patient contact, to collect PE data using interviews or observations [ 3 ].
Meanwhile, it is crucial to understand what types of service are provided to patients to improve healthcare. Since one small and specific clue can significantly impact the evaluation of the patient’s medical service experience, service clue management is critical to improving the patient’s healthcare service satisfaction and the service experience. Service clues are related to various aspects of service experience, depending on their type. It is necessary to understand the types of clues and seek service improvement plans accordingly. Berry et al. [ 21 ] introduced service experiences, including ‘functional’, ‘mechanic’, and ‘humanic’ aspects, which contain valuable information that provide insights for creatively transforming the user service experience [ 22 ]. A ‘functional’ aspect is the technique used in providing a PE service; a ‘mechanic’ aspect is an object or environment delivered through the senses; and ‘humanic’ aspects include the interactions, attitudes, emotions, and behaviors between users [ 21 ].
Head and neck cancer (HNC) is relatively rare compared to other cancers, with limited access to treatment information. Due to the anatomical characteristics of HNC, a loss of the essential functions of eating, speaking, and breathing occurs [ 23 ]; patient quality of life deteriorates, and most experience physical and psychological atrophy [ 24 ]. HNC patients often require combinations of several treatments, such as surgery, chemotherapy, and radiation therapy. The treatment duration is long, and rehabilitation entails functional deficits after treatment, so it takes longer to return to everyday life [ 25 ]. Patients undergoing such a long treatment journey often have decreased psychological well-being and physical health. The incidence rate is high in elderly patients and people with low socioeconomic status, resulting in a poor understanding of the disease and the treatment process [ 26 ]. Therefore, providing quality, patient-centered treatment for these patients is crucial. However, few authors have conducted studies on improving the experience of HNC patients [ 1 ].
Thus, improving the physical and psychological well-being of patients with HNC is crucial to improving the overall patient experience, increasing satisfaction with medical services, increasing treatment adherence, and encouraging positive treatment outcomes. Therefore, we aimed to analyze the PE throughout the patient journey of patients with HNC and present a service design strategy for improving the PE at each journey stage. In this regard, the specific research questions were as follows:
- RQ1. What are the enablers and barriers to patient experience at each stage of the treatment journey for patients with HNC?
- RQ2. Which service design strategies be suggested to improve the experience of head and neck cancer patients at each stage of the treatment journey?
2. Materials and Methods
Service design methods such as interviews, observations, and journey maps were used to understand the barriers and enablers (B/E) from the patient’s perspective. Through qualitative content analysis of the patient’s narratives and analysis of service clue types, the patient’s needs at each stage of the treatment journey were visually structured. Since the patient’s treatment journey includes various stakeholders, such as the patients, doctors, families, and caregivers, the opinions of doctors, caregivers, and patients were comprehensively reflected to understand the B/E of the patient’s experience. The study consisted of three phases: (1) identifying the treatment journey of HNC patients, (2) analyzing the B/Es to PE, and (3) drawing insights for improvement ( Figure 1 ). In the first phase, we conducted nine interviews and five observations with 31 participants between August and October 2021 ( Table 1 ).

The flow chart of the research process.
The user research methods and users involved.
Interviews were conducted with doctors, patients, and caregivers, to understand the HNC treatment journey and identify specific actions, touchpoints, and emotions for each journey stage. Interviewees were directly recruited by an otolaryngology specialist from outpatients who had been diagnosed with head and neck cancer. The doctor introduced the purpose and content of the study to the patient and briefly explained the purpose and method of the interview. When the patient and guardian agreed to an interview, an in-depth interview was conducted immediately after outpatient treatment or on a different date. The interview was held in a separate private room in the hospital and lasted about an hour. The interviewees included all patients diagnosed with laryngeal, pharyngeal, or oral cancer who required surgery or were undergoing rehabilitation. The reason for this is that there is little difference in the treatment principles for each subsite, regarding the process that patients experience after treatment, problems and complications, and the needs of patients.
We also made observations during clinical counseling, to precisely understand the users’ activities, physical space, and facility layout, including the furniture, doctor –patient interactions, objects being used, and users’ attitudes and behaviors, if researcher participation was permitted. Based on the user research, a five-phased HNC treatment journey was structured. For the journey map, we identified the specific stages of the HNC treatment journey and analyzed the user’s actions, emotions, and touchpoints related to each stage. The user’s actions were indicated in the order of specific actions that occurred at each stage, and the emotions felt by the patient at each stage were described. A touchpoint is a point of contact where patients, caregivers, and medical staff interact. The touchpoints included various types, such as the pain and emotion of the patient, language to convey information, hospital system, image data, and explanation tools.
In the second phase, we took an inductive approach to analyzing the user research data. Qualitative content analysis and service clue analysis were applied to the semantic analysis of interview data, to understand the B/Es to PE. For the content analysis, following the method introduced by Graneheim and Lundman [ 27 ], we initially divided the full text of the transcript into meaning units matching the topic and purpose we wanted to know about and arranged each unit into a single sentence. A condensed meaning unit was then made by summarizing the keywords, including the manifest meaning unit, which summarizes the direct meaning, and the latent meaning unit, which grasps and interprets the latent meaning. The condensed meaning units were coded based on the core keywords of the semantic structure that was revealed directly or indirectly. The final coded units were plotted onto the JM by classifying negative and positive factors as barriers and enablers to PE. Each coding unit stage was decided considering the comprehensive relationship between the patient’s treatment process, actions, touchpoints, and emotional state. The units were analyzed to determine which service clues corresponded to understanding the characteristics of the service areas to be improved. Finally, based on the identified B/E, we derived insights to improve the PE in phase three. The patient’s B/E and interpreted insights were classified into three service experience aspects, to suggest improvement directions. We received doctor feedback to evaluate the improvement’s priority, importance, and feasibility. For the feedback, we conducted three focus group meetings (one offline and two zoom meetings) and received frequent email feedback. In the first meeting, we reviewed the insights’ appropriateness and discussed whether the patient’s core needs were reflected at each journey stage. In the second meeting, key insights were selected by comprehensively reflecting on the medical service system at the hospital site, the frequency and importance of patient needs based on the patient treatment experience, and the perspectives of medical staff. At the third meeting, the appropriateness of the selected insights and the possibility of additional selections were reviewed, and finally the insights for improvement were confirmed. Confirmed insights were highlighted with **. In the middle of the three meetings, whenever necessary, an email was sent to the medical staff to ask for opinions on the accuracy of terminology, the appropriateness of the content, and the logic of the analysis process. Feedback was reflected in the analysis results as soon as the feedback was received.
3.1. Phase 1—Patient Journey
Interviews were conducted with one specialist and two residents, to understand the treatment process. Based on the interviews, a JM of HNC patients was created, which consisted of five stages: ‘studies for cancer diagnosis and staging’; ‘pre-operative counseling’; ‘getting operation consent’; ‘surgery and recovery’; and ‘rehabilitation and follow-up’ ( Figure 1 ). We also conducted six interviews, five recordings, and two participatory observations with patients and caregivers, to understand the primary touchpoints, actions, and emotions during the patient’s treatment journey.
Table 2 summarizes the patient’s primary actions, emotions, and touchpoints at each stage. Stage 1 (studies for cancer diagnosis and staging) involved four actions: recognizing symptoms, visiting the hospital/consulting, running studies for staging, and checking results/being diagnosed with cancer. As main touchpoints for this stage, the website for navigating cancer information, verbal language between patient and doctor, biopsy and imaging studies for cancer diagnosis, doctor’s attitude toward patients, and patient’s physical pain were identified. Stage 2 (pre-operative counseling) involved four actions (determining treatment methods, explaining and discussing the treatment, and deciding/planning the schedule) and seven touchpoints (evaluation report, body language used by the patient or verbal language between patient and doctor, visual material being used to explain the treatment, doctor’s attitude toward patients, patient’s pain, and hospital system to manage treatment schedule). Stage 3 (getting operation consent) involved four actions (entering the consulting room to sign the operation consent, explaining the surgical process and method, asking questions and answers regarding the consent, and signing the consent), and six touchpoints (consulting room, hand drawings, and image data used to explain the operation consent, body language and verbal language between patient and doctor, and consent paper form). Stage 4 (surgery and recovery) involved three actions (being hospitalized for surgery, recovering after surgery, and consulting other departments), and six touchpoints (doctor’s verbal language, treatment cost, visual material to check the patient’s condition, patient’s pain after the surgery, doctor’s attitude toward patients, and hospital system to support treatment cost and administrative guidance). Stage 5 (rehabilitation and follow-up) involved two actions (undergoing rehabilitation, visiting the hospital for follow-up check) and seven touchpoints (patient’s pain, an education program for patient’s self-care after discharge, hospital system for rehabilitation treatment and education, hospital location/facility, website for continuous information sharing, verbal language, and doctor’s attitude toward patients).
The five stages of the patient journey.
The patient’s emotions showed substantial negative aspects of anxiety and worry throughout the journey. In stage 2, it was found that the patient’s trust in the doctor regarding the surgery revealed a positive desire for treatment. In stages 4 and 5, if the surgical results were good, the will to live was strongly formed as a positive emotion.
3.2. Phase 2—B/E to HNC PE
For each stage of the previously created JM, a content analysis of the data collected during user research was conducted to derive meaning units, which were classified into enablers as positive factors, and barriers as negative factors. Then, each factor was classified according to the corresponding touchpoint and what type of service clue corresponded to each was analyzed. Enablers correspond to a factor that is helpful or necessary to improve the patient’s medical experience. This addresses aspects that need to be further strengthened for providing satisfying HNC PE in the future. On the other hand, barriers correspond to content where users complain of discomfort or have negative evaluations during the treatment process. This refers to the aspects that need to be improved for future PE.
Table 3 (1–5) introduce the enablers and barriers identified at each stage of the five treatment journeys. For each PE factor, the enablers and barriers related to specific actions and touchpoints at each stage were distinguished. Each factor was guided by including the coded source of the interview in parentheses. The service clue corresponding to each factor was identified and marked as (F) as functional clue, (M) as mechanic clue, and (H) as humanic clue. The final insights were derived by synthesizing enablers to overcome barriers. Each insight represents a factor that should be considered for improving the PE for each touchpoint. According to the attributes of each factor, the insights were categorized into information content, information delivery tool, information delivery method, hospital system, patient’s pain, patient’s feelings, doctor’s attitude, treatment cost, education program, and hospital environment.
(1) Journey Stage 1: studies for cancer diagnosis and staging. (2) Journey Stage 2: pre-operative counseling. (3) Journey Stage 3: getting operation consent. (4) Journey Stage 4: surgery and recovery. (5) Journey Stage 5: Rehabilitation and follow-up.
(F), functional aspect; (M), mechanic aspect; (H), humanic aspect. (The full version of this Table 3 containing the reference code numbers for each item is provided in Appendix A — Table A1 ).
For example, considering the touchpoint ‘website’ in Table 3 (1), ‘obtain reliable information from another channel’ as an enabler, ‘lack of information about relatively rare cancers’, and ‘fear of obtaining misinformation’ were found as barriers to PE in stage 1. These three factors were related to ‘obtaining information content’, and insights into the ‘need for reliable information delivery on relatively rare cancer’ could be derived. As the insight related to the subject of ‘information content’ covers the functional technique of providing the PE service, it corresponds to the functional aspect among the three service clues.
The touchpoints of ‘patient’s emotion’, ‘anxiety and worries about life after surgery’, and ‘concerns about a long treatment journey’ were found to be barriers to HNC PE. These two barriers correspond to ‘patient’s feelings’. They can be summarized as an insight into the ‘need to alleviate anxiety and worry about the long-term treatment journey and life after surgery’. This insight represents a humanic clue, because it deals with the emotional aspect of humans.
The following insights were identified at each stage of the journey during the above analysis process.
3.2.1. Stage 1
In Stage 1, from the content analysis of user research data, 13 enablers (ten functional clues, and three humanic clues) and 11 barriers (six functional clues, one mechanic clue, and four humanic clues) were identified. Taken together, 11 insights (seven functional, one mechanic and three humanic clues) were elicited, two of which were identical (marked as *). Thus, the following 10 insights were finally derived, as shown in Table 3 (1): ① delivery of reliable information content about relatively rare cancers (1-5c, 1-19b, 1-20a, 1-20b); ② provision of information delivery media that patients can easily access and use anywhere (1-10, 1-19a, 1-21); ③ description of the need for pre-operative examinations and guidance on the evaluation procedure (1-12a, 1-12b, 1-13a, 1-13b, 1-14b); ④ advance notice on the opportunity to choose evaluation procedure (1-12c); ⑤ * use of terms that are easy for the patient to understand (1-7a); ⑥ establishing close links between departments and staff, to minimize schedule delays (1-5b, 1-13c, 1-16, 1-17); ⑦ information on the overall treatment process, including the cause of cancer (1-8, 1-9, 1-11, 1-14c); ⑧ alleviation of the patients’ psychological shock following cancer diagnosis (1-5a); ⑨ alleviation of anxiety and worry about the long-term treatment journey and life after surgery (1-6, 1-14a); ⑩ inducement of psychological stability and formation of a bond with the patient through information sharing and a positive attitude toward patients (1-1, 1-2, 1-4, 1-15a).
Among these, ① and ③–⑦ correspond to the ‘functional’ aspects of improving PE, such as the content and method of information delivery and the hospital system. Insight ② is related to the ‘mechanic’ aspect of improving visible elements, and ⑧–⑩ involves patient emotion and the interaction between the doctor and the patient, corresponding to the ‘humanic’ aspect.
⑤ “The doctor didn’t use many technical terms in English but explained it in Korean, making it easier to understand and better. It was also good that the doctor didn’t just pass over something like inflammation and checked it properly.” (1-7a)
② “At first, I searched for cancer-related information on the Internet, but there was no detail, just bragging about the hospital they work at. There is no information at all on the internet.” (1-10)
⑧ “It’s the first time I’ve heard of cancer, so I wondered if it couldn’t be done without an incision, and the names of cancers were so diverse and difficult that it was hard to understand. I didn’t know anything, so I pretended to understand and said, ‘Yes, please do well’ when the professor said a lot.” (1-1)
3.2.2. Stage 2
In Stage 2, 22 enablers to strengthen PE (12 functional clues, four mechanic clues, and six humanic clues) and 12 barriers to be improved (five functional clues, three mechanic clues, and four humanic clues) were identified. The synthesized result revealed 17 insights (nine functional clues, two mechanic clues, and six humanic clues) as shown in Table 3 (2): ① accurate diagnosis with clear evidence (2-50); ② comprehensive explanation and general overview of the treatment process and diagnosis with clear explanation of surgical methods, results, and rehabilitation (2-3a, 2-14, 2-16a, 2-13, 2-17b, 2-20); ③ guidance and selection of treatment methods (2-33); ④ use of easy-to-understand terms (2-35b, 2-51a, 2-51b); ⑤ provision of easy-to-understand visuals (2-17a, 2-34, 2-35a, 2-35b, 2-36, 2-38b, 2-42) and comprehensive documentation (2-17b); ⑥ services that identify and support the patient situation and concerns (2-4a, 2-4b, 2-8b, 2-21a, 2-21c, 2-24a, 2-24b); ⑦ access to successful cancer treatment cases (2-10a, 2-10b); ⑧ use of non-language communication tools (2-37a, 2-37b, 2-40); ⑨ alleviation of patient anxiety about surgery and outcomes (2-2b, 2-3a, 2-5a, 2-5b, 2-7a, 2-7b, 2-45, 2-57b, 2-57c, 2-58b); ⑩ empathy for the patient’s concerns and anxiety (2-4c, 2-6, 2-24c, 2-63); ⑪ understanding and empathy with the situation of the patient/caregiver (2-8a, 2-21b, 2-54, 2-56); ⑫ need for positive attitude and words when conveying objective facts (2-44, 2-46, 2-47a, 2-48a, 2-48c, 2-48d); ⑬ iterative explanation of information (2-18, 2-49a); ⑭ sharing cases with other patients (2-53b); ⑮ provision of text message service (2-61a, 2-61b); ⑯ trust building between doctor and patient (2-51c, 2-52, 2-55); and ⑰ emotional stability and expression of desire for long-term treatment (2-53a).
Of these, ①–④, ⑥–⑦, and ⑬–⑮ relate to the ‘functional’ aspect regarding the content and method of information delivery and the hospital system. Points ⑤ and ⑧ relate to tangible tools corresponding to the ‘mechanic’ aspects; ⑨–⑫ and ⑯–⑰ concern the interaction between the doctor and the patient, representing the ‘humanic’ aspect.
② “I think it would be comfortable if the doctor explained, ‘You’re in this condition now, but it will change like this in the future.’ I wonder how long the surgery will take, whether I can return to my daily life after surgery, how the evaluation test is conducted, and whether there is a ward to be hospitalized. It would be nice if the doctor could tell me about how many rounds of chemotherapy should be done after surgery.” (2-3a)
⑤ “It was nice that the doctor looked at my condition through an endoscope to see if I had healed well and explained it well. However, it was difficult to understand the explanation with CT images.” (2-17a)
⑨ “We know it’s the worst, but when the doctor speaks negatively, we lose heart. We hope to be at least a little hopeful.” (2-2b)
3.2.3. Stage 3
Stage 3 involved seven enablers (seven functional clues) and 20 barriers (five functional clues, eight mechanic clues, and seven humanic clues) regarding HNC PE improvement. Together, a total of 14 insights (seven functional clues, five mechanic clues, and two humanic clues) were derived, as shown in Table 3 (3): ① securing a separated space to avoid noise and maintain privacy (3-1b); ② furniture arrangement that allows doctors and patients to interact better and focus on documents); (3-32b, 3-39b, 3-40b, 3-41b); ③ information delivery, considering the hierarchy of content (3-6b, 3-14b, 3-16b); ④ pre-information on treatment direction/postoperative pain management/intensive care in the ICU (3-7e, 3-10e, 3-23e, 3-28e); ⑤ balanced explanation by topic of information content (3-6b, 3-14b, 3-23b); ⑥ use of easy-to-understand terminology (3-13e, 3-24e); ⑦ clear explanation, pointing out the operative site (3-15e); ⑧ use of large clear visuals that are easy to understand and recognizable by older patients (3-2b, 3-30b, 3-31b, 3-32b, 3-37b, 3-41b); ⑨ alleviation of anxiety and worry (3-2b, 3-3b, 3-5b, 3-8b, 3-11b, 3-42b); ⑩ empathy and comfort from caregivers, friends, family, and medical staff (3-4b, 3-6b, 3-7b); ⑪–⑫ support of short-answer or non-verbal communication methods and tools (3-22b, 3-29b); ⑬ improvement of the content system and composition, for effective information delivery (3-16b, 3-17b); and ⑭ improved document design, so that elderly patients can easily see where to sign (3-41a).
Of these, ③–⑦, ⑪, and ⑬ relate to the content and method of information delivery, representing the ‘functional’ aspects; ①–②, ⑧, ⑫, and ⑭ correspond to the ‘mechanic’ aspects, dealing with hospital environment, such as space and furniture arrangement; and ⑨–⑩ are related to the interaction between the doctor and the patient, representing the ‘humanic’ aspect.
③ “The doctor gave an explanation that is difficult to understand at once, but it seemed important. But all of them were hard to understand, so I didn’t even know what was more important, and it was not even in my head. If that’s the case, I think focusing on what’s really important is better.” (3-6b)
⑧ “The text on the consent form was too small to read, the terms were difficult to pronounce, and the explanation took too long. I understood it at first, but later I couldn’t remember anything. I couldn’t even find a place to sign it, so the doctor marked it for me.” (3-2b)
⑨ “From the day I found out he had cancer, I think I am also a cancer patient. I can’t even tell you how hard it was mentally, very much.” (3-3b)
3.2.4. Stage 4
Stage 4 included 12 enablers (six functional clues, three mechanic clues, and three humanic clues) and 12 barriers (four functional clues and eight humanic clues) for HNC PE improvement. When synthesized, 14 insights (five functional, three mechanic, and six humanic clues) were drawn, and two factors were identical (marked as *). Thus, a final 13 insights were determined, as shown in Table 3 (4): ① comprehensive guidance on the overall process of pre-operative treatment/postoperative progress (4-12); ② alleviation of negative feelings and psychological pains (4-4, 4-27b, 4-35); ③ communication and financial support for medical expenses (4-11, 4-26a, 4-26b, 4-27a, 4-27b, 4-28a, 4-28b, 4-29b); ④ comprehensive information guidance on the treatment progress after surgery (4-1, 4-14a, 4-14b, 4-14c, 4-31a); ⑤ use of clear visuals (4-17, 4-18); ⑥ active response to patient pain after surgery (4-7b); ⑦ preparation of measures for nutrition supply (4-5, 4-7a, 4-25a, 4-25b); ⑧ support in maintaining a positive attitude toward treatment and recovery (4-2b); ⑨ empathy and support for the caregiver’s psychological pain (4-9, 4-10); ⑩* simplified procedures through flexible link between departments (4-19, 4-20, 4-29a,4-30a, 4-30b, 4-30c, 4-31b); ⑪ encouragement and psychological support for patients after surgery (4-6); ⑫ information media that can comprehensively guide treatment procedures and content (4-13); ⑬ provision of communication media between patients/caregivers/medical staff (4-22).
Among these, ①–④ and ⑩ correspond to the content of information delivery and the hospital system, representing the ‘functional’ aspects; ⑤ and ⑫–⑬ relate to the provision and use of physical tools, engaging in the ‘mechanic’ aspect; and ②, ⑥–⑨, and ⑪,relate to patient psychology and pain and present insights for improving PE, representing the ‘humanic’ aspect.
① “My brother was in the integrated nursing ward for a month, but I couldn’t visit even once because of COVID-19. So, the nurses in charge informed me of the patient’s condition in detail by text message every evening. I thank them so much.” (4-12)
⑫ “Even the slightest change in the symptoms after the surgery scared me, and I was worried about whether this was normal or a complication. I wish the doctor would let me know in advance that the symptoms will change like this in the future and what is normal.” (4-13)
⑥ “I don’t care about anything else, but it’s uncomfortable to breathe and talk. I need to get treated well and exercise hard from now on. My tongue is still swollen so I can’t speak fluently.” (4-7b)
3.2.5. Stage 5
Stage 5 identified 14 enablers (five functional clues, three mechanic clues, and six humanic clues) and 13 barriers (five functional clues, one mechanic clue, and seven humanic clues) for HNC PE improvement. From these, 17 insights were drawn, as shown in Table 3 (5): ① encouragement to maintain a hopeful attitude toward treatment (5-3a, 5-4, 5-7, 5-8b); ② empathy and encouragement for the caregiver’s feelings (5-8a); ③ taking care of the patient’s nutritional intake and preparing countermeasures (5-1, 5-3b, 5-6b, 5-6c); ④ information related to symptom relief after surgery (5-11); ⑤ guidance on daily activity after surgery (5-22, 5-24); ⑥ flexible links and communication between departments (5-25); ⑦ providing a consultation window in case of additional inquiries (5-10); ⑧ provision of administrative assistance for guidance and reservations (5-20); ⑨ development of rehabilitation training guidelines (5-21); ⑩ provision of programs on the cause of cancer and smoking cessation/abstinence from alcohol (5-23a, 5-23b, 5-23c); ⑪ provision of a program to introduce cancer overcoming cases/medical technology trends (5-19); ⑫ convenient means of transportation to the hospital (5-16); ⑬ establishment of a comfortable and pleasant treatment environment (5-18); ⑭ development of a reliable information medium (5-17a, 5-17b); ⑮ building doctor–patient trust (5-12b, 5-13, 5-14, 5-15); ⑯ creation of an atmosphere in which patients can express their opinions comfortably (5-2); and ⑰ calm and empathetic attitude of medical staff, to relieve anxiety and tension (5-3c, 5-12a).
Of these, ④–⑪ correspond to the ‘functional’ aspects, such as information delivery content, hospital system, and educational programs; ⑫–⑭ relate to physical means, tools, and environments, representing ‘mechanic’ aspects; and ①–③ and ⑮–⑰explain the ‘humanic’ aspects, dealing with patient’s negative feelings and doctor’s empathetic attitude.
⑤ ” No detailed guidance was provided on how to behave and rehabilitate after discharge. I only heard that I should quit drinking and smoking and exercise regularly. That was all I got from the hospital.” (5-22)
⑫ “In fact, if it’s the same way, I’m better off closer to home.” (5-16)
① “The first time I visited the professor after discharge, he encouraged me to say that I had endured the difficult surgery well. He helped and encouraged me a lot. The professor did well with the surgery, so I should have hope while receiving rehabilitation treatment.” (5-3a, 5-4, 5-7, 5-8b)
The result of visually structuring using a JM, by synthesizing the above analysis, is shown in Figure 2 , and the JMs for each stage correspond to Figure 3 (1–5).

The integrated patient journey map consists of five phases.

( 1 ) The patient journey map: Stage 1. ( 2 ) Stage 2. ( 3 ) Stage 3. ( 4 ) Stage 4. ( 5 ) Stage 5.
3.3. Phase 3—Insights by Service Clue Type
In this phase, by reclassifying the PE factors and the related insights identified in phase 2 into the three types of service clues, according to the attributes of the factors, we tried to identify which factors should be considered for PE improvement and what are the implications for improving HNC PE by service clue type. To this end, the ten PE factor categories classified using the attributes were divided into three service clue types. The critical insights derived at each stage of the treatment journey were summarized according to each service clue and factor type, as shown in Table 4 . The implications for PE improvement from relating the PE factor derived for each of the three service clue types to the journey stage were as follows.
Summary of insights based on the HNC patient needs.
(S), Journey stage, **, Key factors and insight evaluated as relatively necessary for improving HNC PE from the doctor’s feedback. (The full version of this Table 4 containing the reference code numbers for each item is provided in Appendix A — Table A2 ).
The ‘functional’ clue dealing with the technical aspect of providing a specific service for improving PE included five PE factors: information delivery content, information delivery method, hospital system, treatment cost, and education program. In information delivery contents, a comprehensive guidance of information related to the overall journey process consisting of five stages was required. For the information delivery method, easy-to-understand terms for patients in journey Stages 1-3, where many explanations about treatment methods and processes are made to the patient, were highlighted. In hospital system, links and communication between departments were emphasized for Stages 1, 4, and 5, to reduce patient waiting times and ensure the consistent delivery of treatment information, in consultation with other departments. In Stage 2, a customized support service for the patient that considered patient circumstances was required, along with a text message service, enabling interactions between the patient, caregiver, and medical staff and for updating the patient’s pre-operative study results. In Stage 5, an additional consultation window with the medical staff, patient continuous communication with the medical staff through administrative support, and discomfort minimization during the long-term treatment process were identified as important issues. Regarding treatment costs, government and insurance support were particularly emphasized in Stage 4. In Stage 5, educational programs were emphasized, regarding providing smoking cessation and abstinence programs, cases of overcoming cancer in other patients, and the latest HNC treatment technology trends.
The ‘mechanic’ clue, dealing with objects or environments perceptible by the senses, for improving PE was related to information delivery tools and the hospital environment. For information delivery tools, a reliable and easily accessible information delivery medium was identified as necessary in Stages 1, 4, and 5. Patients wanted as much information about treatment as possible in the early cancer diagnosis and recovery stages after surgery. In Stages 2–4, the use of clear and visible visual data that elderly patient could easily understand was emphasized. Stages 2 and 3 required a communication tool that could replace language, considering patients with difficulty in communicating verbally. In Stage 4, before and after surgery, a flexible communication tool or medium that enabled active information sharing and emotional expression among patients, caregivers, and medical staff was required. Regarding the hospital environment, in Stage 3, securing an independent counseling space for patient stability and interaction with the doctor was necessary. Thus, the arrangement of space and furniture to improve and support interactions between the patient and the doctor and help the patient focus on obtaining operation consent should be considered. In Stage 5, according to the prolonged rehabilitation treatment, it was necessary to establish convenient means of transportation and a comfortable treatment environment, considering patient convenience.
The ‘humanic’ aspect of PE dealing with user interactions, attitudes, emotions, and behaviors included needs related to the patient’s pain, patient’s feelings, and doctor attitudes. In patient’s pain, attention to nutrition supply, preparation of countermeasures, and active response to patient pain after surgery were required in Stages 4 and 5. Regarding patient’s feelings, active support and encouragement from caregivers and medical staff were needed. It was also necessary for the patient to understand the treatment journey in advance, by guiding them through detailed information for each stage, to alleviate negative emotions and maintain emotional stability. Empathy and encouragement of the caregiver’s grievances about caring for the patient after discharge were also crucial in Stages 4 and 5. In Stages 2 and 5, maintaining a positive attitude toward treatment by building trust with the doctor helps increase patient satisfaction with the PE. For doctor’s attitude, at all stages of the journey, except for Stage 3, the positive attitude of the medical staff, empathy, and encouragement of the patient played a vital role in the PE.
Above, we considered the PE factors and related insights that should be considered to improve HNC PE by service clue type. The insights for each stage of the journey presented in Table 4 reflect the perspectives of patients, caregivers, and medical staff involved in the HNC treatment journey, and it can be seen that various factors should be considered for each service clue.
We conducted three focus group meetings with HNC doctors to identify the relative importance of the factors that should be considered for improving HNC PE. We received feedback on the priorities and importance of the PE factors and related insights from two highly experienced HNC doctors, who both closely directly or indirectly interact with patients and fully understand their situation and needs. As a result, six insights were evaluated as necessary for the functional clue about information content. Three insights for information delivery methods, two for the hospital system, and two for the education program were evaluated as significant. Regarding the mechanic clue, the ‘use of large and clear visuals that are easy to understand and recognizable by older patients’ was evaluated as necessary for the information delivery tool. For the humanic aspect, three insights related to the patient’s feelings and three insights related to the doctor’s attitude were each evaluated as significant. The PE factors evaluated as relatively necessary during the feedback are marked with ** in Table 4 .
Considering these feedback results, the information content that patients acquire during the treatment process is critical to improving the experience of HNC patients. In addition to the method of delivery of this information content, the painful emotions felt by patients during the treatment process, and the positive attitude of medical staff who respond appropriately to them can also be interpreted as key.
In summary, the early stages of the journey (S1–S3) involved the patient’s cancer diagnosis and treatment method delivery ( Table 4 ). Thus, using terms that the patient could easily understand or using visual materials was necessary. Comprehensive guidance for the overall treatment process must be provided from the early stage of the journey. In the later stages (S4–S5) related to the rehabilitation after surgery, as the frequency of contact between the doctor and the patient decreases, the burden on the patient to self-manage increases. Therefore, the preparation of rehabilitation guidelines and educational programs was emphasized. Encouragement and empathy for patient anxiety were required at all journey stages. The need for an information delivery medium that the patient can always find easily was highlighted ( Figure 3 . (1)-(5)).
4. Discussion
In this study, the following results were derived through a three-phased process. In phase 1, user interviews and participatory observation identified a five-staged HNC treatment journey process. For each stage, relevant user experiences were collected, including main actions, touchpoints, and patient emotions.
In phase 2, the barriers and enablers of PE were analyzed for each journey stage through content analysis of the collected user research data. As a result, ten insights were derived from 13 enablers and 11 barriers in the first stage. In stage 2, 17 insights emerged from 22 enablers and 12 barriers. In stage 3, 14 insights were derived from seven enablers and 20 barriers. In stage 4, 13 insights were identified from 12 enablers and 12 barriers. In stage 5, 17 insights were derived from 14 enablers and 13 barriers.
In phase 3, the insights derived from each stage were classified according to the three service clue types and categories of PE factors. The ‘functional’ aspect of service experience included five categories and 40 insights, stressing the importance of a comprehensive guide to the treatment process, delivery of reliable information, use of the easy-to-understand terms, repeated summary explanation, the establishment of close and flexible linkages between departments, and provision of educational programs (smoking/alcohol, and cancer survivor patient stories). Regarding the ‘mechanic’ aspect, two categories and 15 insights were included, such as using large and clear visuals that patients can understand easily. Three categories and 23 insights were included in the ‘humanic’ aspect, highlighting patient’s psychological stability, trust in doctors, and doctor’s encouragement and support by maintaining a positive attitude.
First, for the ‘functional’ aspect, regarding information content, the overall process of the treatment journey for HNC patients should be guided in the early stages of the journey. As framing the holistic picture of the journey from the patient’s perspective (who must undergo a long-term treatment process) can help maintain emotional stability, the information content a patient needs at each journey stage is different. Thus, the information provided at each stage should be classified. An integrated database should also be established to provide the information for each category and to patients in a JM, where the treatment journey can be easily identified.
Second, as part of the ‘functional’ aspect, to maintain long-term and continuous treatment, educational programs should be provided in which patients can participate or receive information after discharge. Through providing a rehabilitation guide booklet and smoking cessation and sobriety education programs that can be referenced after discharge, information for continuous rehabilitation and self-management should be delivered to patients needing psychological support.
Third, with regard to the ‘mechanic’ aspect, stages 1-3 are when a patient first encounters HNC and is inundated with information. For elderly patients with reduced memory, a means to understand and accept information more efficiently is needed. As it is difficult for these patients to understand treatment information verbally, regarding information delivery methods and tools, large and clear visual data, such as human body models or illustration images, should be used as additional explanatory tools.
Fourth, regarding the ‘humanic’ aspect, HNC is a relatively rare cancer that requires long-term and complex treatment, and most patients experience depression and anxiety. To support patient emotions and to alleviate patient anxiety and worries, as well as to encourage a hopeful attitude throughout the treatment process, a video about overcoming cancer or a community for HNC patients could be provided for information exchange and psychological support between patients.
We conducted a convergence study of the medicine and service design by applying the JM methodology. As a result, we could reveal PE barriers and enablers that medical staff were perhaps unaware of. In addition, it was possible to derive realistic improvements through close interaction with the medical staff. As a result of our study, various items at each stage of the HNC patient’s journey were identified as factors related to patient experience improvements, including functional aspects such as information and systems, mechanic aspects related to specific objects or facilities to support function, and humanic aspects such as the emotions and attitudes of patients and caregivers. This aligns with previous research [ 5 ], which revealed that PCC includes various aspects, such as the hospital system, patient–doctor information and communication, and caregiver support. Furthermore, the significance of this study rests in it identifying and introducing more specific factors for PE improvement. In addition, using a JM, the patient interview and observation data were embodied and visually displayed for each stage of the journey. This helped in understanding the intangible patient needs data. This shows that our results are meaningful, as a case study supporting the assertion of previous studies [ 3 , 8 , 17 , 18 , 19 ] that a JM helps convert intangible data into concrete structures. It also supported the usefulness of JMs as a methodology for improving health care.
Since this study conducted interviews with a small number of patients and caregivers, it is difficult to generalize the results. However, a qualitative research analysis was employed to discover in-depth insights into the patients, by conducting repeated observations and interviews over the journey stages for a small group of users who fit the purpose of the study. As Nielsen et al. [ 28 ] mentioned, rather than conducting a single study with many people, it is more effective to repeatedly collect and evaluate data with a small number of people, thus supporting the approach of this study. Lastly, this study was targeted at HNC patients, and the research scope could be expanded to other cancer fields or general cancer patients.
5. Conclusions
Applying service design to the medical field is a critical strategy for providing quality care from a patient’s perspective. Since the patient’s journey is complex and includes diverse aspects, it is essential to interpret the various viewpoints and complex data delicately. A JM is a valuable tool for understanding the relationships and patterns between meanings, by visually structuring complex patient needs. Thus, it is of great help to holistically understand where and how the patient’s treatment experience occurs for each journey. Employing a qualitative methodology that collects patient needs through interviews and observations and systematically analyzing the contents through an inductive approach can provide more in-depth insights than the quantitative measurement of patient satisfaction. The results of this study can be used as reference materials for researchers interested in creative methodologies for improving PE.
By applying the creative methodology of service design, we employed three integrated perspectives to improve the experience of HNC patients. First, rather than dividing the treatment journey of HNC patients into fractured stages, the overall journey flow was examined in an integrated manner, to identify the changes and differences in the patient’s needs at each stage. Second, to improve HNC PE, the perspectives of caregivers and medical staff, and the patient’s perspectives were, directly and indirectly, reflected through a participatory method. Third, to identify the implications for improvement, three aspects of technical support, tangible tools, and human interactions were integrated and viewed, by applying three service experience clues: functional, mechanic, and humanic.
The study’s findings could be applied to real patient-centered treatment. Patients can easily understand the treatment process, maintain a good doctor–patient relationship, and actively participate in their treatment. This might effectively improve the treatment outcomes of difficult-to-treat HNC. It could be widely applied to cancers other than HNC, or other diseases. In that case, the efficiency of medical care would be increased, while maintaining the doctor–patient relationship in the entire medical field.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2021R1I1A4A01059504).
(F), functional aspect; (M), mechanic aspect; (H), humanic aspect.
(S), Journey stage, **, Key factors and insight evaluated as relatively important for improving HNC PE from the doctor’s feedback.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, I.N. and Y.K.; methodology, E.K. and Y.K.; validation, I.N.; formal analysis, E.K.; investigation, E.K. and Y.J.; data curation, E.K. and Y.J.; writing—original draft preparation, E.K.; writing—review and editing, Y.K.; visualization, Y.J.; supervision, I.N. and Y.K.; project administration, Y.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the Catholic University of Korea (OC21RISI0106, 20 August 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.

COMMENTS
Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [ 12 - 14 ]. Many tools may be used to measure and understand patient experience [ 15, 16 ]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and ...
A "Patient Journey" is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed information matrix. The ...
The Experience Journey of the Patient. A recurrent and prominent theme in discussions of the patient experience is centering the patient's perception or perspective on the health care they receive (7,13).Health-care providers who seek to understand the patient's perspective of their experience will obtain a greater understanding of the patient experience.
Patients initiate the recommended treatment plan, experiencing the day-to-day challenges and improvements associated with their patient journey in a hospital. Key considerations: Monitor treatment adherence, side effects, and the patient's overall experience during this active phase.
The "Patient Journey" connects professional expert guidelines—with foreseen medical interventions, screening, treatment—with patient needs -both medical and psychological. Each "Patient Journey" is divided in several stages that are considered inherent to the specific disease. Each stage in the journey is referenced under three ...
We address the patient's need for education at each of the following phases of the care journey: Prevention and wellness. Discovery. Testing. Diagnosis. Treatment. Recovery or management and ...
Process mapping enables the reconfiguring of the patient journey from the patient's perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital. Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the ...
Based on the treatment journey, this study aimed to present insights into improving the patient-centered service experience for head and neck cancer (HNC) patients. We interviewed and observed patients, caregivers, and doctors. We conducted a qualitative content analysis and service clue analysis to identify barriers and enablers to patient care and to derive insights into the patient ...
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end. ... and the steps taken for diagnosis and treatment. The patient's post-care journey includes follow-ups from the healthcare provider, post ...
Patient journey mapping is a process common in the healthcare field that helps visualize the process patients go through to receive care for a specific illness. It is meant to help identify and understand the details of all patient touch points within a specific treatment experience. Our patient journey map underscores the obstacles and ...
A basic patient journey of chronically ill patients usually begins during the pre-service period with the registration of the patient at the outpatient clinic. Following, an intake consult takes place between the patient and the healthcare professional to establish a first relationship and discuss the expectations for the treatment.
What is the patient journey? The patient journey is the sequence of events that begins when a patient first develops a need for care. Rather than focusing on service delivery, the patient journey encompasses all touchpoints of a patient's healthcare experience-from locating healthcare providers and scheduling appointments, to paying the bill and continuing their care after treatment.
Compared with the past year, a third of a patients said their health status was worse, while better outcomes were reported by patients who saw an HCM expert or went to a center of excellence. According to one patient, "It has been confusing living with the symptoms (dyspnea, weight gain, tiredness/weakness).
Patient Treatment Space Preferences. To test the relationship between the treatment journey and space preference, patients were asked various questions, including their personality type, how long they have been visiting the facility, their baseline preference of treatment space, and whether that preference changed over time. Responses showed ...
There is currently no curative treatment for patients with metastatic breast cancer; consequently, the main objectives are to prolong survival, enhance or maintain quality-of-life, and control symptoms ... This study describes the patient journey of women with breast cancer, specifying the different phases with the most relevant aspects of each ...
A patient journey represents the entire sequence of events that a patient experiences within a given healthcare system or across providers, from scheduling an appointment for a regular checkup to receiving treatment for an illness or injury.
The Patient Journey Study utilized the COPD Foundation's research infrastructure to: identify and recruit all of the study participants; facilitate an asynchronous focus group to identify issues in the patient's COPD treatment journey utilizing a private feature on the COPD Foundation's COPD360social online community;; develop and deploy a survey to the COPD Patient Powered Research ...
Based on the treatment journey, this study aimed to present insights into improving the patient-centered service experience for head and neck cancer (HNC) patients. We interviewed and observed patients, caregivers, and doctors. We conducted a qualitative content analysis and service clue analysis to …
The mean cost per patient for the entire HCC treatment journey for the common patient group was $94,419 ± $56,844. The mean cost per patient per year was $51,649, with a mean duration of treatment, from first treatment to last treatment, of 21.9 months. The cost driver was the LRTs in which the mean cost per patient was $60,382 ± $38,841 and ...
This is the story of my journey from diagnosis through treatment to survivorship; a journey marked by medical and emotional challenges but also by profound personal growth and resilience. ... Having a dual perspective as both a patient and a healthcare professional offered a unique vantage point. I understood the medical language, the treatment ...
Background Breast cancer is one of the most prevalent diseases in women. Prevention and treatments have lowered mortality; nevertheless, the impact of the diagnosis and treatment continue to impact all aspects of patients' lives (physical, emotional, cognitive, social, and spiritual). Objective This study seeks to explore the experiences of the different stages women with breast cancer go ...
Many patients describe their treatment journey as a roller coaster. We are here to help you navigate the ups and downs. When patients and families meet with our team, initial misconceptions quickly fall away. Feelings of apprehension are replaced with relief and comfort knowing there is an entire team here to listen, support, and encourage.
This online tool helps you find the right treatment for you — and near you. It guides you through a step-by-step process to finding a highly qualified professional treatment provider. ... Alcohol use disorder (AUD) is a medical condition that doctors diagnose when a patient's drinking causes distress or harm. The condition can range from ...
Introduction. Cancer is a leading cause of morbidity and mortality worldwide. In 2013, there were ∼1,660,290 new cancer cases and 580,350 cancer deaths in the United States. 1 A diagnosis of cancer is still very stressful and frightening for the majority of patients and families 2-4 although the number of patients living with cancer has increased threefold since 1971. 5 According to the ...
Recommendations for Patients. ... Description of the problem including date of onset, and any diagnosis and follow-up treatment; Description of medical or surgical interventions taken, including ...
From his first Gillette appointment, Wyatt has been seen by board-certified orthopedic surgeons, pediatric orthopedic surgery specialists, and physician assistants who specialize in the treatment and correction of clubfoot in the youngest of patients—Wyatt began the serial casting process for clubfoot at just a month and a half old. "I was scared," Katie shares, "but he has been a dream.
There isn't any treatment to stop perimenopause. Perimenopause is a natural part of life. The "cure" for perimenopause occurs when your periods stop and you enter menopause. But your healthcare provider may recommend over-the-counter or prescription perimenopause treatment to help ease symptoms. Your provider may recommend:
When studying the patient journey using administrative claims, analyses typically limit the analysis to specific elements of the patient journey, for instance, categorizing the first-line treatment after condition onset, or looking at the first 3 events of the treatment pathway. 31, 32 Claims have also been used to measure outcomes of pathway ...
Jelly Roll is working hard at getting healthier as he and his 44-year-old wife Bunnie XO have embarked on an IVF journey. ... Infertility may affect many cancer patients undergoing treatment due to cancer treatment's impacts on the body. Various cancer treatments, including chemotherapy and radiation, can affect both men's and women's ...
First, rather than dividing the treatment journey of HNC patients into fractured stages, the overall journey flow was examined in an integrated manner, to identify the changes and differences in the patient's needs at each stage. Second, to improve HNC PE, the perspectives of caregivers and medical staff, and the patient's perspectives were ...